Archive for June, 2016
CDC Recommendations for Subsequent Zika IgM Antibody Testing
Thursday, June 23rd, 2016This is an official
CDC HEALTH UPDATE
Distributed via the CDC Health Alert Network
June 21, 2016, 1140 EDT (11:40 AM EDT)
CDCHAN-00392
CDC Recommendations for Subsequent Zika IgM Antibody Testing
Summary
Testing for Zika virus infection using real-time reverse-transcription polymerase chain reaction (rRT-PCR)
molecular assays is now commercially available. When requesting Zika rRT-PCR testing from a
commercial laboratory, providers should be aware that commercial laboratories performing rRT-PCR
currently do not also offer Zika IgM enzyme-linked immunosorbent assay (ELISA) or confirmatory
serologic testing (plaque reduction neutralization test, or PRNT). Therefore, if possible, providers should
store a serum aliquot for subsequent Zika IgM ELISA testing if the rRT-PCR assay is negative. Otherwise,
collection of an additional serum sample may be necessary.
Recommendations
• rRT-PCR (molecular) testing should be performed for patients possibly exposed to Zika virus who
have symptoms consistent with Zika virus infection
• Providers who request molecular testing for Zika virus infection from a commercial testing
laboratory are advised to retain and store in a refrigerator (2-8°C) an aliquot of the patient’s
serum for subsequent Zika IgM ELISA testing if the rRT-PCR is negative
• For specimens that are rRT-PCR negative from the commercial laboratory and no stored serum
specimen is available, another serum specimen should be collected within 12 weeks of symptom
onset for Zika IgM ELISA testing
• Appropriate samples for molecular testing are serum samples collected <7 days and urine
samples collected <14 days after symptom onset. Urine should always be collected with a
patient-matched serum specimen.
Background
Molecular assays for detection of Zika virus RNA are now commercially available under Emergency Use
Authorizations (EUAs) issued by the Food and Drug Administration (FDA). CDC recommends molecular
testing using rRT-PCR for serum samples collected <7 days and urine samples collected <14 days after
symptom onset. A positive rRT-PCR test is confirmation of Zika virus infection. However, because of the
decline in the level of viremia over time and possible inaccuracy in reporting of dates of illness onset, a
negative rRT-PCR result does not exclude Zika virus infection. In such cases, CDC recommends
serologic testing by ELISA for Zika IgM antibody.
Currently, commercial laboratories that offer rRT-PCR testing do not provide Zika IgM ELISA testing with
PRNT confirmation and have no routine process to forward specimens to another testing laboratory.
Therefore, when requesting Zika rRT-PCR testing from a commercial laboratory, providers should retain
an aliquot of the serum for Zika IgM ELISA testing if the rRT-PCR testing is negative. Blood should be
collected and processed per routine guidelines (collected in a serum separator tube with serum aliquots
transferred to new vials), and one of the serum aliquots should be stored in a refrigerator (2-8°C) until it is
known if additional IgM testing is indicated. If a serum aliquot cannot be stored or is not available, but
further testing is indicated, a new blood sample should be collected. Serum samples for IgM testing
should be collected from patients within 12 weeks of symptom onset. Providers should contact their local
health department to discuss IgM testing of stored or newly collected serum from patients who are rRTPCR
negative.
For More Information
• Zika virus specimen collection:
http://www.cdc.gov/zika/hc-providers/body-fluids-collection-submission.html.
• Interim guidance for Zika virus testing of urine:
http://www.cdc.gov/mmwr/volumes/65/wr/mm6518e1.htm
The Centers for Disease Control and Prevention (CDC) protects people’s health and safety by preventing and
controlling diseases and injuries; enhances health decisions by providing credible information on critical health
issues; and promotes healthy living through strong partnerships with local, national, and international
organizations.
____________________________________________________________________________________
Categories of Health Alert Network messages:
Health Alert Requires immediate action or attention; highest level of importance
Health Advisory May not require immediate action; provides important information for a specific incident or situation
Health Update Unlikely to require immediate action; provides updated information regarding an incident or situation
HAN Info Service Does not require immediate action; provides general public health information
##This message was distributed to state and local health officers, state and local epidemiologists, state
and local laboratory directors, public information officers, epidemiologists, HAN coordinators, and clinician
organizations##
Across the India state of Bihar, lightning has killed 56 people, mostly farm laborers, and injured 24 others when thunderstorms and monsoon rains lashed the region
Wednesday, June 22nd, 2016PAHO late last week reported 21,200 new chikungunya cases, to bring the 2016 total in the Americas to 148,453 infections.
Wednesday, June 22nd, 2016
The Kingdom of Saudi Arabia notified WHO of 6 additional cases of MERS-CoV infection, including 1 death.
Wednesday, June 22nd, 2016Middle East respiratory syndrome coronavirus (MERS-CoV) – Saudi Arabia
Between 15 May and 15 June 2016, the National IHR Focal Point for the Kingdom of Saudi Arabia notified WHO of 6 additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including 1 death.
Details of the cases
- A 49-year-old female from Buridah city developed symptoms on 9 June and was admitted to a hospital on 10 June. She tested positive for MERS-CoV on 12 June. The patient has comorbidities. Investigation of history of exposure to the known risk factors in the 14 days prior to the onset of symptoms is ongoing. Currently she is in critical condition admitted to ICU.
- “…After emergency department triage she was admitted to a vascular surgery ward, where MERS-CoV wasn’t suspected and the woman was treated without isolation in a multi-bed room. The woman apparently died from her infection, according to an MOH update yesterday.The setting exposed 49 healthcare workers and patients to the virus, the WHO said. Saudi Arabia’s MOH first reported her illness on Jun 15.
After the woman’s MERS-CoV infection was detected, health officials sent a rapid response team, and intensive contact tracing and screening in the hospital and household identified 20 people who were positive for the virus. The group includes 17 healthcare contacts and 3 household contacts; 18 of the 20 have asymptomatic infections.
Of the hospital contacts, 11 are healthcare workers, including 3 who cared for the index patient. All are expats, and all but 1 are women. Six of the cluster cases are current or recently discharged hospital patients.
The only patient in the hospital cluster with symptoms is a 69-year-old Saudi woman who had been hospitalized since late February with an unrelated medical condition. She is listed in stable condition.
The WHO said the hospital closed the vascular surgery ward, rescheduled elective procedures, and established control measures….”
- “…After emergency department triage she was admitted to a vascular surgery ward, where MERS-CoV wasn’t suspected and the woman was treated without isolation in a multi-bed room. The woman apparently died from her infection, according to an MOH update yesterday.The setting exposed 49 healthcare workers and patients to the virus, the WHO said. Saudi Arabia’s MOH first reported her illness on Jun 15.
- A 68-year-old male from Madinah city developed symptoms on 8 June and was admitted to a hospital on 13 June. He tested positive for MERS-CoV on 15 June. The patient has comorbidities and a history of frequent consumption of raw camel milk. He has no history of exposure to the other known risk factors in the 14 days prior to the onset of symptoms. Currently the patient is in stable condition admitted to a negative pressure isolation room on a ward. The Ministry of Agriculture was informed and investigation of camels is also ongoing.
- A 54-year-old male from Alkharj city developed symptoms on 7 June and was admitted to a hospital on 11 June. He tested positive for MERS-CoV on 13 June. The patient has comorbidities and a history of frequent contact with camels and consumption of their raw milk. He has no history of exposure to the other known risk factors in the 14 days prior to the onset of symptoms. Currently the patient is in stable condition admitted to a negative pressure isolation room on a ward. The Ministry of Agriculture was informed and investigation of camels is also ongoing.
- A 59-year-old male from Tabuk city developed symptoms on 1 June and was admitted to a hospital on 6 June. The patient tested positive for MERS-CoV on 8 June. The patient had comorbidities and a history of frequent contact with camels and consumption of their raw milk. He had no history of exposure to the other known risk factors in the 14 days prior to the onset of symptoms. The patient passed away on 12 June. The Ministry of Agriculture was informed and investigation of camels is also ongoing.
- An 85-year-old female from Riyadh city developed symptoms on 27 May and was admitted to a hospital on 1 June. A nasopharyngeal swab was collected on 1 June and tested positive for MERS-CoV on 2 June. The patient has comorbidities. Investigation of history of exposure to the known risk factors in the 14 days prior to the onset of symptoms is ongoing. Currently the patient is in stable condition admitted to a negative pressure isolation room on a ward.
- A 72-year-old male from Hail city developed symptoms on 8 May and was admitted to a hospital in Riyadh on 12 May. The patient tested positive for MERS-CoV on 14 May. The patient has comorbidities and a history of frequent contact with camels and consumption of their raw milk. He has no history of exposure to the other known risk factors in the 14 days prior to the onset of symptoms. Currently the patient is in stable condition admitted to a negative pressure isolation room on a ward. The Ministry of Agriculture was informed and investigation of camels has been performed.
Globally, since September 2012, WHO has been notified of 1,739 laboratory-confirmed cases of infection with MERS-CoV, including at least 629 related deaths.

WHO risk assessment
MERS-CoV causes severe human infections resulting in high mortality and has demonstrated the ability to transmit between humans. So far, the observed human-to-human transmission has occurred mainly in health care settings.
The notification of additional cases does not change the overall risk assessment. WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to animals or animal products (for example, following contact with dromedaries) or human source (for example, in a health care setting). WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV early because like other respiratory infections, the early symptoms of MERS-CoV are non-specific. Therefore, health-care workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures.
Until more is understood about MERS-CoV, people with diabetes, renal failure, chronic lung disease, and immunocompromised persons are considered to be at high risk of severe disease from MERS‐CoV infection. Therefore, these people should avoid close contact with animals, particularly camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, or eating meat that has not been properly cooked.
Given the lack of evidence of sustained human-to-human transmission in the community, WHO does not recommend travel or trade restrictions with regard to this event. Raising awareness about MERS-CoV among travellers to and from affected countries is good public health practice.
WHO: Advice for national health authorities and health care providers about practices and measures for travelers visiting Brazil to stay safe and healthy.
Wednesday, June 22nd, 2016Brazil – Health Advice for Travellers to the 2016 Summer Olympic and Paralympic Games
21 June 2016
The XXXI Summer Olympic and Paralympic Games Rio de Janeiro 2016, Brazil, will take place from 5 to 21 August 2016 and from 7 to 18 September 2016 respectively. Five additional cities will be hosting matches of the Olympic football tournament – Belo Horizonte, Brasilia, Manaus, Salvador, and São Paulo.
The following recommendations are intended to advise national health authorities and health care providers about practices and measures for travellers visiting Brazil to stay safe and healthy.
Before departure, travellers should be advised about health risks in the areas they plan to visit and related preventive practices and measures to minimize the probability of acquiring diseases and of having accidents.
Travellers to Brazil should consult the travel advice issued by their national authorities.
Health authorities of Brazil provide health advice for visitors to Brazil on their website in portuguese (see list of websites below). Health services affiliated to the public Unified Health System of Brazil (Sistema Único de Saúde, SUS) are free of charge for all individuals, including visitors.
Vaccine preventable diseases
A medical consultation should be scheduled as early as possible before travel but at least 4–8 weeks before departure in order to allow sufficient time for immunization schedules to be completed for both routine vaccines and vaccines indicated according to the specific destinations. Even when departure is imminent, there is still time to provide both advice and some vaccines.
Routine vaccines
Travellers should be vaccinated according to their national immunization schedule, which will vary from one country to another. Routine immunization schedules, established by national authorities, include vaccination against diphtheria, pertussis, tetanus, polio, measles, hepatitis B, Haemophilus influenzae type b and, in many countries, additional diseases such as rubella, mumps, flu, yellow fever, human papillomavirus, and rotavirus and pneumococcal diseases.
Since July 2015, Brazil has interrupted measles transmission, following an outbreak associated with an imported case. As measles is still endemic or circulating in many countries, measles vaccinations should be up to date to prevent importation of the virus to Brazil. Similar considerations apply for rubella, which was eliminated from Brazil in 2009.
Wild poliovirus has been eliminated from Brazil since 1989. To prevent the re-introduction of polio into Brazil, travellers from countries where polio cases have recently occurred should be fully immunized.
For travellers at risk of serious complications of influenza, vaccination should be considered. WHO recommends seasonal influenza vaccination for pregnant women, the elderly, individuals with specific chronic medical conditions, children aged 6-59 months, and healthcare workers. Note that WHO advices pregnant women not to travel to the Olympics or any area where Zika virus is circulating. The influenza strain currently circulating in Brazil, A(H1N1)pdm09, is included in both the northern hemisphere 2015-2016 and the southern hemisphere 2016 vaccines. The Olympic and Paralympic Games will take place after the influenza season in Rio de Janeiro is expected to have peaked in June and July; however, there are regional variations and cases occur throughout the year in Brazil. At-risk travellers should ideally receive influenza vaccine at least two weeks prior to departure.
Travel-related vaccines
Depending on the specific travel itinerary, additional vaccines might be considered for some travelers. Unvaccinated travellers should be offered such vaccines in accordance to their national recommendations.:
- Hepatitis A: Brazil is an intermediate endemicity country and prone to hepatitis A outbreaks;
- Hepatitis B: The risk of contracting hepatitis B is likely to be low, except for travellers engaging in high risk behaviours such as tattoos and injecting drug use. Hepatitis B vaccine was introduced into the national immunization schedule in Brazil in 1998;
- Typhoid fever: The incidence of typhoid fever in Brazil is highest in the North and North-East, including Amazonas and Manaus which is hosting the Olympic football tournament;
- Rabies: The risk of rabies infection in Rio de Janeiro and the remaining five cities hosting the Olympic football tournament is negligible;
- Yellow fever: A single, lifetime dose of Yellow Fever vaccine is recommended for all travellers older than 9 months visiting areas at risk of yellow fever transmission. The vaccination should be conducted at least 10 days before departure. The vaccine confers lifelong protection. Vaccination is not recommended for travellers limiting their stay to the following cities hosting Olympic and Paralympic Games’ events: Rio de Janeiro, Salvador, São Paulo. Further international spread of the ongoing yellow fever outbreak in Angola could potentially require WHO to adjust these recommendations (see list of websites below for more information).
Mosquito-borne diseases
Personal protective measures
Although the risk of mosquito borne disease is lower during winter, travellers should still take personal protective measures to prevent mosquito bites. These include:
- Whenever possible, wearing clothes (preferably light-coloured) that cover as much of the body as possible during the day;
- Using repellents that contain DEET (diethyltoluamide), or IR 3535, or icaridin andare applied to exposed skin or to clothing and used in strict accordance with the label instructions, especially regarding the duration of protection and timing of re-application. If repellents and sunscreen are used together, sunscreen should be applied first and the repellent thereafter;
- Choosing sanitary accommodations with piped water and physical barriers such as proper window and door screens to prevent mosquitoes from entering rooms;
- Avoiding areas in cities and towns with no piped water and poor sanitation, which constitute ideal breeding grounds for mosquitoes.
Arboviruses transmitted by Aedes mosquitoes
In addition to yellow fever (see above vaccination requirements), mosquito-borne diseases transmitted by Aedes species mosquitoes include chikungunya, and dengue and Zika virus disease.
Dengue and chikungunya
Detailed information about dengue and chikungunya is available on the websites of Brazil’s Ministry of Health, WHO and PAHO/AMRO (see list of websites below). There is no vaccination for chikungunya. Dengue vaccination is not recommended for travellers.
Zika virus disease
Zika virus infection usually causes a mild disease, and many cases of Zika virus infection are asymptomatic. However, following an outbreak of Zika virus in Brazil in 2015 and its subsequent spread in the Americas, an unusual increase in serious neurological disorders was seen in the off-springs of pregnant women who had been infected, including cases of microcephaly and congenital neurological malformations. Cases of Guillain-Barré Syndrome (GBS), a rare but serious form of muscle weakness, were observed among adults. Based on a growing body of research, there is scientific consensus that Zika virus is a cause of microcephaly and Guillain-Barré syndrome. Zika virus is primarily spread by mosquitoes, though sexual transmission has increasingly been documented.
On the basis of current knowledge about Zika virus disease and its complications, the following is recommended to national health authorities and health care practitioners:
- To provide travellers to areas of ongoing Zika virus transmission, including Brazil, with up-to-date advice on appropriate measures to reduce the risk of becoming infected, including by preventing mosquito bites and practicing safe sex (e.g. use condoms correctly and consistently); and on the potential consequences and complications of infection, especially for women who are pregnant or planning a pregnancy; non-barrier forms of birth control will not protect against sexual transmission of Zika virus infection;
- To advise pregnant women not to travel to areas of ongoing Zika virus outbreaks, including Brazil;
- To advise women who inadvertently become pregnant or discover they are pregnant in or shortly after returning from Brazil, and/or other areas with ongoing Zika virus transmission, to contact their health care providers;
- To advise pregnant women whose sexual partners live in or travel to areas with Zika virus outbreaks to ensure safe sexual practices or abstain from sex for the duration of their pregnancy;
- To advise travellers to practice safe sex or abstain from sex during their stay in Brazil, and/or other areas with ongoing Zika virus transmission, and for at least eight weeks after their return. If men experience symptoms of Zika virus disease, they should adopt safer sex practices or abstain from sex for at least six months;
- To advise travellers returning from Brazil, and/or other areas with ongoing Zika virus transmission, not to donate blood for at least four weeks after departure from the area1;
- To advise health care practitioners to be on alert for Zika virus disease in travellers returning from Brazil and/or other areas with ongoing Zika virus transmission;
- National authorities should provide health care practitioners with clear guidance on how to refer travellers with suspected Zika virus infection for suitable clinical management and testing where appropriate.
Malaria (transmitted by Anopheles mosquito)
The risk of malaria transmission is negligible or non-existent except in the administrative region of Amazonas, corresponding to the Northern states of Brazil. This includes the city of Manaus which is hosting some of the Olympic football matches.
Plasmodium falciparum infections account for approximately 15% of malaria cases in Brazil. In malaria-affected areas, in addition to mosquito bite prevention (including use of repellents and sleeping under an insecticide treated mosquito net), chemoprophylaxis with atovaquone–proguanil, or doxycycline, or mefloquine should be considered and selected according to reported side-effects and contraindications. Alternatively, for travel to rural areas with low risk of malaria infection, mosquito bite prevention can be combined with stand-by emergency treatment (SBET).
Based on the risk assessment by Brazilian health authorities, the national guidelines do not include recommendations on malaria chemoprophylaxis. Therefore, the access to these drugs while in Brazil will be limited and antimalarial drugs should be purchased before travelling. Travellers who become ill with a fever while traveling in a malaria-risk area within Brazil should seek immediate medical attention (see list of websites below for diagnostic and treatment health centres). Travellers who become ill with a fever for up to one year after their travel should inform their health care practitioners about their travel history. There is no vaccination recommended for malaria.
Sexually Transmitted Infections (other than Zika virus infection)
The risk of infection with HIV, syphilis, gonorrhoea, chlamydia, herpes, Hepatitis B virus (HBV), and other sexually transmitted infections is primarily limited to travellers engaging in sexual risk behaviours, especially unprotected sex and particularly with sex workers and among men who have sex with men and injecting drug users. Therefore, the adoption of safe sex practices, and specifically consistent and correct condom use, is recommended. Brazilian authorities launched a health promotion and prevention campaign in relation with sexually transmitted diseases, AIDS and hepatitis (see list of websites below).
Food and water safety
As gastrointestinal infections can be common in Brazil, health care practitioners should advise travellers to take precautions to avoid illnesses caused by unsafe food and drink. These precautions include: frequent hand washing and always before handling and consuming food; making sure that food has been thoroughly cooked and remains steaming hot; choosing safe water (e.g. bottled water or, if in doubt, water vigorously boiled); avoiding any uncooked food, apart from fruits and vegetables that can be peeled or shelled; avoiding foods at buffets, markets, restaurants and street vendors if they are not kept hot or refrigerated/on ice.
The quality of recreational water in Rio de Janeiro, including in the venues hosting Olympic and Paralympic Games events, has been suboptimal because of sewage contamination. While corrective actions are being taken, travellers should follow the advice issued by competent local authorities (see list of websites below).
Other infectious disease risks
The risk for travellers of acquiring airborne infections, such as tuberculosis and meningitis is limited, unless they stay in overcrowded indoor spaces.
Travellers to the Belo Horizonte area should be aware of the risk of acquiring tickborne Brazilian spotted fever, caused by the bacterium Rickettsia rickettsii, and that might result from contact with an infected rodent called capybara.
Travellers to the Salvador area should be aware of the risk of acquiring leptospirosis, caused by the Leptospira bacterium, which might result from skin and mucosal exposure to water and soil contaminated with the urine of infected animals. A wide range of animals can carry the bacterium.
The risk of leishmaniasis (both cutaneous and visceral), schistosomiasis, lymphatic filariasis, and other neglected tropical diseases is mostly associated with rural areas of the north-eastern region of Brazil.
Safety and security and other health risks
Crime, including theft and violent crime, does occur in Brazil. Travellers should be advised to exercise caution and only use authorized airport taxis or shuttle buses, not travel alone at night, avoid questionable areas, and travel with a companion.
Traffic accidents and injuries, mostly caused by motor vehicle crashes, are the leading causes of death among travellers under the age of 55 years. After heavy rainfall, flash floods and landslides, especially in urban areas, have been a frequent cause of injuries and other emergencies.
Travellers should be aware of the presence of poisonous animals, such as scorpions and snakes, and take precautions to avoid any contact with such animals. Local health authorities can provide more detailed information about specific areas of risk.
It is good practice for health care practitioners to systematically collect the travel history from their patients, taking into account that some travel associated infections have a long incubation period.
List of websites for further information
- National travel and health advice websites
• http://www.who.int/ith/links/national_links/en/ - Health advice for travellers to Brazil on Brazil’s Ministry of Health website
• http://portalsaude.saude.gov.br/index.php?option=com_content&view=article&id=9643#preparando3 - Information on global polio vaccination requirements
• http://www.polioeradication.org/ - Information on influenza in Brazil (in Portuguese)
• http://portalsaude.saude.gov.br/index.php/situacao-epidemiologica-dados-influenza - Information on rabies in Brazil
• http://saude.sp.gov.br/resources/instituto-pasteur/pdf/wrd2015/situacaodaraivanobrasil-eduardopachecodecaldas.pdf - Information on yellow fever vaccination requirements
• http://who.int/emergencies/yellow-fever/en/
• http://www.who.int/ith/2015-ith-county-list.pdf?ua=1
• http://gamapserver.who.int/mapLibrary/Files/Maps/
ITH_YF_vaccination_americas.png?ua=1 - Information on dengue fever
• http://www.who.int/mediacentre/factsheets/fs117/en/
• http://www.paho.org/hq/index.php?option=com_topics&view=article&id=1&Itemid=40734&lang=en - Information on Chikungunya
• http://www.who.int/mediacentre/factsheets/fs327/en/
• http://www.paho.org/hq/index.php?option=com_topics&view=article&id=343&Itemid=40931&lang=en - Information on Zika virus disease
• http://www.who.int/emergencies/zika-virus/en/
• http://www.paho.org/hq/index.php?option=com_content&view=article&id=11585&Itemid=41688&lang=en
• http://www.paho.org/hq/index.php?option=com_content&view=article&id=11603:countries-territories-zika-autochthonous-transmission-americas&Itemid=41696&lang=en
• http://portalsaude.saude.gov.br/index.php/situacao-epidemiologica-dados-zika
• http://combateaedes.saude.gov.br/ and
• http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/secretarias/svs/zika
• http://www.paho.org/hq/index.php?option=com_content&view=article&id=11585&Itemid=41688&lang=en
and at http://www.who.int/emergencies/zika-virus/en/ - Information on Malaria
• http://portalsaude.saude.gov.br/images/jpg/2015/junho/24/Mapa-de-risco-2014.jpg
• http://bvsms.saude.gov.br/bvs/publicacoes/guia_prevencao_malaria_
viajantes.pdf
• http://www.who.int/ith/2016-ith-county-list.pdf?ua=1
• http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/leia-mais-o-ministerio/662-secretaria-svs/vigilancia-de-a-a-z/malaria/12193-centros-para-diagnostico-e-tratamento - Information about the health promotion campaign launched by the Brazilian Government on the occasion of the Olympic and Paralympic Games
• http://www.aids.gov.br/noticia/2016/ddahv-e-unaids-anunciam-campanha-em-parceria-para-os-jogos-rio-2016 - Information on water and sanitation
• http://www.who.int/water_sanitation_health/bathing/statement-rio-water-quality/en/
1 National health authorities/national blood services should put in place and implement appropriate procedures to reduce the risk of transmission of mosquito-borne infections through transfusion, including temporarily deferring donors who are at high risk of infection due to international travel.
As of June 17, 2016, a total of 3,605 patients had been tested for Zika virus in NYC, 182 (5.0%) of which have been confirmed cases of Zika infection; 20 cases were in women who were pregnant at the time of diagnosis, and two cases of Guillain-Barré syndrome were diagnosed.
Wednesday, June 22nd, 2016Lee CT, Vora NM, Bajwa W, et al.
Zika Virus Surveillance and Preparedness — New York City, 2015–2016.
MMWR Morb Mortal Wkly Rep. ePub: 21 June 2016.
DOI: http://dx.doi.org/10.15585/mmwr.mm6524e3.
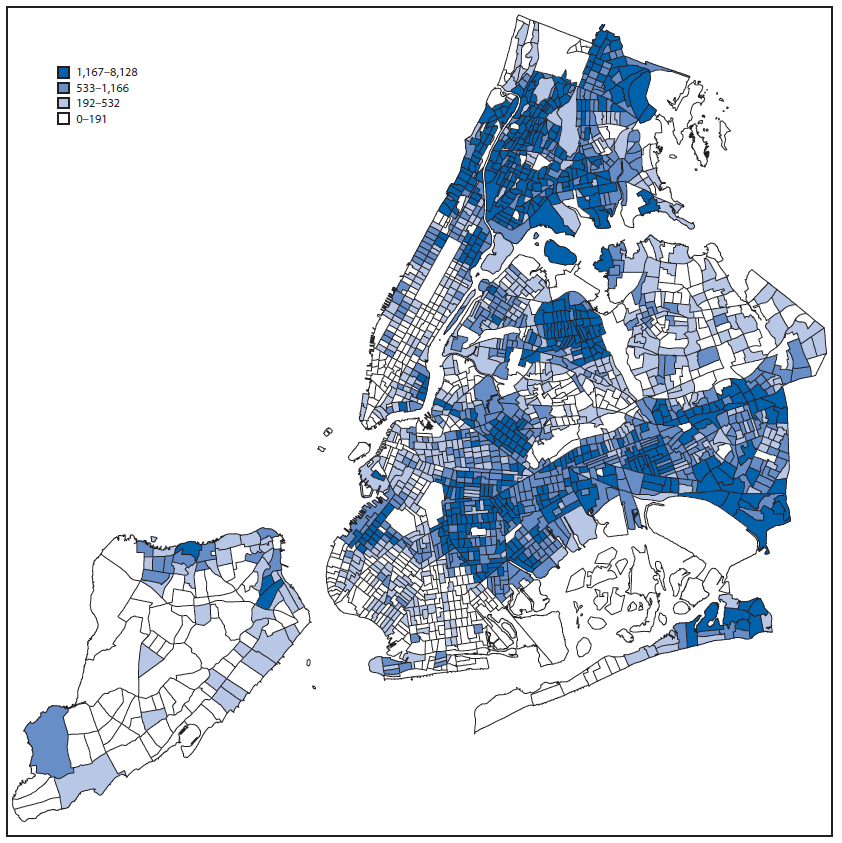
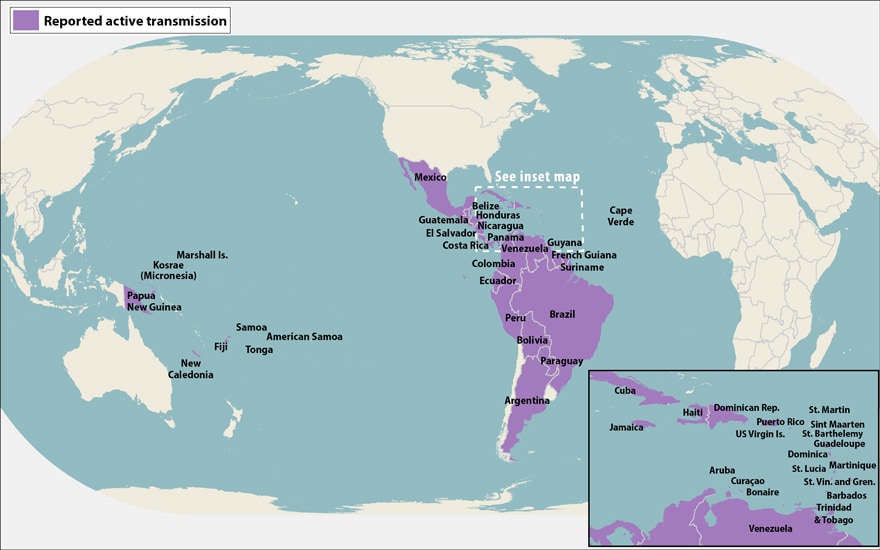
Number of persons born in Mexico, the Caribbean, Central America, and countries in South America with active Zika virus transmission, by U.S. Census tract of residence — New York City, January–February 2016
Over the past 3 days, Saudi Arabia’s Ministry of Health announced 12 new MERS-CoV cases, 9 of them in Riyadh, with at least 8 linked to a quickly growing healthcare outbreak in the city.
Tuesday, June 21st, 2016-1.gif)
Inovio Pharmaceuticals, Inc. and GeneOne Life Science, Inc. announced that they have received approval to initiate a phase I human trial to evaluate Inovio’s Zika DNA vaccine (GLS-5700)
Tuesday, June 21st, 2016New wildfires erupted Monday near Los Angeles
Tuesday, June 21st, 2016National Preparedness Level
Level 2
National Fire Activity
Initial attack activity: Light (100 new fires)
New large incidents: 2
Large fires contained: 1
Uncontained large fires: 15
Area Command Teams Committed: 0
NIMOs committed: 1
Type 1 IMTs committed: 3
Type 2 IMTs committed: 2
Source:
Incident Management Situation Report