Archive for March, 2018
3/25/1911: the Triangle Shirtwaist Company factory in New York City burns down, killing 145 workers
Sunday, March 25th, 2018CDC: During week 11 (March 11-17, 2018), influenza activity decreased in the United States.
Sunday, March 25th, 2018During week 11 (March 11-17, 2018), influenza activity decreased in the United States.
- Viral Surveillance: Overall, influenza A(H3) viruses have predominated this season. However, in recent weeks the proportion of influenza A viruses has declined, and during week 11, influenza B viruses were more frequently reported than influenza A viruses. The percentage of respiratory specimens testing positive for influenza in clinical laboratories decreased.
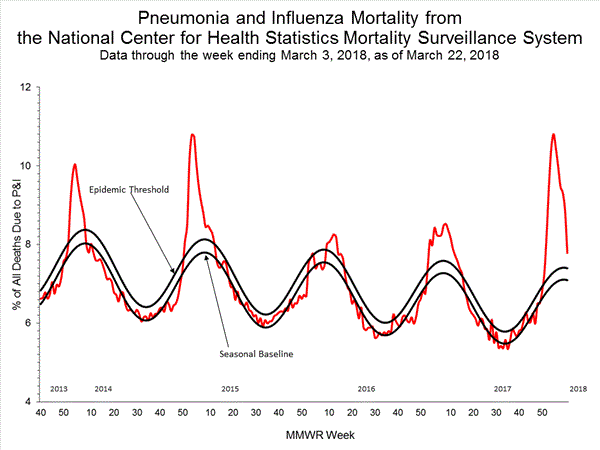
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was above the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
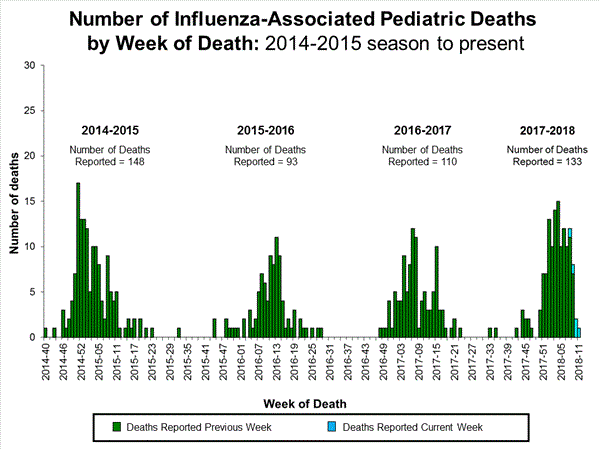
- Influenza-associated Pediatric Deaths: Five influenza-associated pediatric deaths were reported.
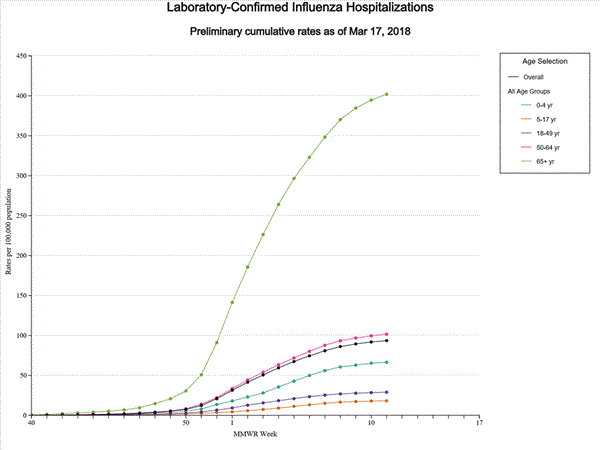
- Influenza-associated Hospitalizations: A cumulative rate of 93.5 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
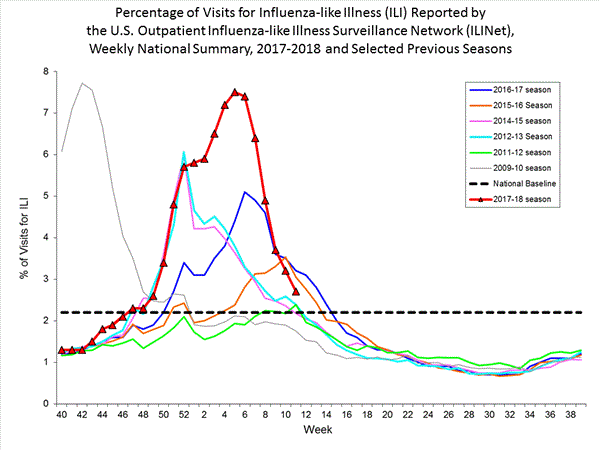
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 2.7%, which is above the national baseline of 2.2%. Nine of 10 regions reported ILI at or above region-specific baseline levels. Six states experienced high ILI activity; nine states experienced moderate ILI activity; New York City, Puerto Rico, the District of Columbia, and 17 states experienced low ILI activity; and 18 states experienced minimal ILI activity.
- Geographic Spread of Influenza: The geographic spread of influenza in 17 states was reported as widespread; Guam, Puerto Rico and 26 states reported regional activity; the District of Columbia and five states reported local activity; and the U.S. Virgin Islands and two states reported sporadic activity.
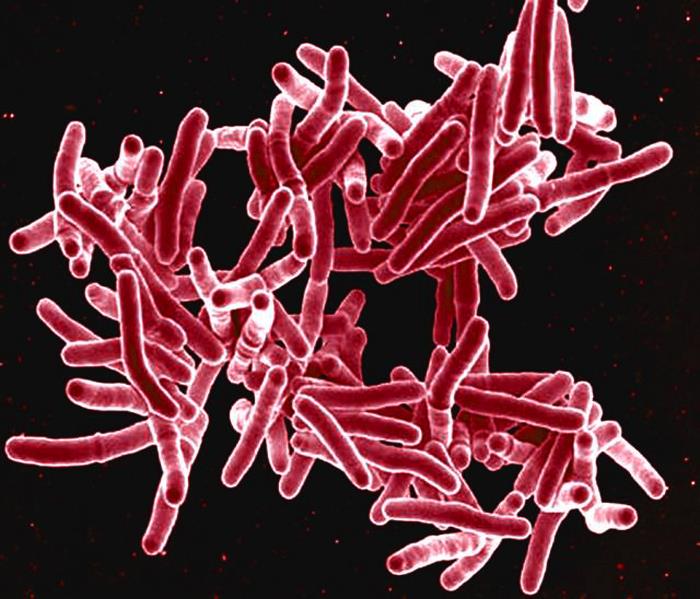
NIH Statement on World Tuberculosis Day 2018
Saturday, March 24th, 2018Friday, March 23, 201
Statement of Christine F. Sizemore, Ph.D., Richard Hafner, M.D., and Anthony S. Fauci, M.D.
Mtb is transmitted through the air and primarily affects the lungs. TB is the leading killer among infectious diseases and among the top 10 causes of death worldwide. The World Health Organization (WHO) estimates that in 2016, TB claimed the lives of 1.7 million people, including 250,000 children, and 10.4 million people were newly infected with Mtb. TB is the primary cause of death for individuals co-infected with HIV. According to the WHO, more than 2 billion people globally are “latently” infected with TB, meaning they carry the bacteria but are currently without symptoms, which would include cough, fever, weight loss and night sweats. People with latent TB infection cannot actively transmit TB bacteria to another person. Up to 13 million people in the United States are estimated to have latent TB infection, according to the U.S. Centers for Disease Control and Prevention. Overall, people with latent TB infection have a 5 to 15 percent lifetime risk of developing active TB disease. This risk increases for people with compromised immune systems, such as those living with HIV, people receiving immunosuppressive therapy (such as individuals being treated for cancer), as well as diabetics, smokers and the malnourished.
WHO’s End TB Strategy envisions an end to TB by 2035. To accomplish this, incremental improvements in understanding the disease and in the tools used to identify, treat, and prevent it will not be sufficient. Rather, accelerated efforts and transformative advances are needed. Recent engagement includes NIAID participation in the first “WHO Global Ministerial Conference on Ending TB in the Sustainable Development Era: A Multisectoral Response” in Moscow. At this November 2017 meeting, the urgent need for a more intensive biomedical research approach to controlling and ultimately eliminating TB was clearly articulated. Specifically, we need a more intensive interdisciplinary systems biology approach (using cutting-edge methods, large data sets, and modeling to understand complex biological systems) to improve our understanding of how Mtb infection causes disease. Additionally, we must work toward improved diagnostics that can detect Mtb in a variety of clinical specimens in addition to sputum. Also, rapid, accurate, and inexpensive “point-of-care” tests to distinguish between drug-sensitive and drug-resistant Mtb must be developed. NIAID investments in research contributed substantially to the WHO-endorsed GeneXpert MTB/rifampicin resistance diagnostic currently in use, and the Institute continues to support the development of next-generation TB diagnostics.
Today’s treatment regimens for TB require too many drugs, often with toxic side effects, that must be taken for six months or longer. With the increasing incidence of multidrug resistant TB (MDR-TB), these regimens often become very lengthy (up to 20 months), more complex, costly, and more prone to failure. Extensively drug-resistant TB (XDR-TB) is even more difficult to treat, and for some patients, no effective treatment regimens exist. Despite the urgent need for new and improved TB treatments, there is a paucity of new drugs in the clinical development pipeline. To address this deficit, NIAID-supported investigators have engaged in cross-disciplinary, international collaborations designed to spur basic science and early-stage TB drug discovery. Additionally, NIAID has used its HIV/AIDS clinical trials networks to enhance TB clinical research by conducting key studies of potential TB treatment strategies. For example, a NIAID-led study found that a one-month antibiotic regimen to prevent active TB disease in people with latent TB infection was as safe and effective as the standard 9-month course in people living with HIV. Additionally, the NIAID-funded HIV/AIDS clinical trials networks have conducted studies of improved regimens for MDR-TB therapeutics geared to treat both HIV-infected and uninfected adults and children.
A broadly effective preventive TB vaccine could avert millions of new Mtb infections; however, critical knowledge gaps have made developing such a vaccine a difficult challenge. The current Bacille Calmette-Guerin (BCG) vaccine, developed in 1921, offers protection against disseminated TB disease and death in children, but this protection does not reliably extend into adulthood. A recent study suggests that revaccination with the vaccine could potentially prevent Mtb infections in high-risk adolescents. To reliably protect against the transmissible pulmonary form of the disease in adults, a new, more effective intervention strategy is needed. NIAID supports basic, preclinical and clinical research to find and develop new, innovative vaccines to prevent TB infection and disease.
The WHO estimates that 53 million lives were saved between 2000 and 2016 through improved TB diagnosis and treatment. Through an intensified research agenda, a sustained commitment to supporting and conducting TB research, and a renewed effort to work with other agencies and organizations, NIAID is dedicated to helping eliminate this disease and improving and saving the lives of people with TB. In September 2018, the United Nations General Assembly will conduct a high-level meeting on TB—representing an important step forward by governments and other partners from around the world in the fight against TB. On this World TB Day, we stand with global leaders in response to the bold call of action to make history and end TB.
Anthony S. Fauci, M.D., is Director of the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health in Bethesda, Maryland. Richard Hafner, M.D., is chief of the TB Clinical Research Branch in NIAID’s Division of AIDS; Christine F. Sizemore, Ph.D., is chief of the Tuberculosis and other Mycobacterial Diseases Section in the NIAID Division of Microbiology and Infectious Diseases.
NIAID conducts and supports research — at NIH, throughout the United States, and worldwide — to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website.
March 24: World TB Day
Saturday, March 24th, 2018Each year, we recognize World TB Day on March 24. This annual event commemorates the date in 1882 when Dr. Robert Koch announced his discovery of Mycobacterium tuberculosis, the bacillus that causes tuberculosis (TB).
Although TB is preventable and curable, many people in the United States still suffer from this disease. Anyone can get TB, and our current efforts to find and treat latent TB infection and TB disease are not sufficient. Misdiagnosis of TB still exists and health care professionals often do not “think TB.”
The U.S. theme for World TB Day 2018 is “Wanted: Leaders for a TB Free United States. We can make history. End TB.” CDC and its domestic and international partners, including the National TB Controllers Association, Stop TB USA, and the global Stop TB Partnership are working together to eliminate this deadly disease. But we need your help.
Be sure to check back for more information and resources as we get closer to World TB Day. You can also follow us on Twitter @CDC_TB and Facebook @CDCTB and sign up for email updates through GovDelivery.
Join CDC’s World TB Day Thunderclap, and share the End TB message March 23rd at 2:00 p.m. EDT/11:00 a.m. PDT, spreading an idea through Facebook, Twitter, and Tumblr that cannot be ignored. We need 100 supporters for the Thunderclap to take effect, so please visit http://thndr.me/5APDuS before March 23 to sign up and learn more.
Get Involved in the Fight to End TB:

World TB Day Resources
Download and share World TB Day graphics, messages, social media tools, and more

U.S. TB Champions
Learn how you and your organization can participate in CDC’s TB Elimination Champions project.

World TB Day Activities
Tell us about your community’s World TB Day activities, and see how others are observing.
Alert – Level 2, Practice Enhanced Precautions in Brazil due to Yellow Fever
Friday, March 23rd, 2018Yellow Fever in Brazil
Key Points
- There is a large, ongoing outbreak of yellow fever in multiple states of Brazil(https://wwwnc.cdc.gov/travel/destinations/traveler/none/brazil). Since early 2018, a number of unvaccinated travelers to Brazil contracted yellow fever; many of these travelers were infected on the island of Ilha Grande (Rio de Janeiro State). Several have died.
- Travelers to Brazil should protect themselves from yellow fever by getting yellow fever vaccine at least 10 days before travel, and preventing mosquito bites.
- In addition to areas in Brazil where yellow fever vaccination has been recommended since before the recent outbreaks, the vaccine is now also recommended for people who are traveling to or living in: All of Espirito Santo State, São Paulo State, and Rio de Janeiro State as well as a number of cities in Bahia State.
- People who have never been vaccinated against yellow fever should avoid traveling to areas of Brazil where yellow fever vaccination is recommended.
- Travelers going to areas with ongoing outbreaks may consider getting a booster dose of yellow fever vaccine if it has been 10 or more years since they were vaccinated.
- Yellow fever vaccine is available at a limited number of clinics in the United States, so travelers should plan ahead to get the vaccine.
What is yellow fever?
Yellow fever is caused by a virus that is spread through mosquitoes. Symptoms of yellow fever (fever, chills, headache, backache, and muscle aches) take 3–6 days to develop. About 15% of people who get yellow fever develop serious illness including bleeding, shock, organ failure, and sometimes death.
What is the current situation?
In early 2017, the Brazilian Ministry of Health reported outbreaks of yellow fever in several eastern states, including areas where yellow fever was not traditionally considered to be a risk. Since the end of 2017, yellow fever cases have reoccurred in several states, especially in the states of Rio de Janeiro, Minas Gerais, and São Paulo, including areas close to the city of São Paulo.
In early 2018, a case of yellow fever was reported in an unvaccinated Dutch traveler who had stayed near the São Paulo metropolitan region. Since then, there have been reports of other unvaccinated travelers to Brazil who visited areas with yellow fever outbreaks and contracted yellow fever; many of these travelers were infected on the island of Ilha Grande (Rio de Janieiro State). Several of these travelers died. None were from the United States.
In response to the outbreak that began in early 2017, the World Health Organization has expanded the list of areas where yellow fever vaccination is recommended for international travelers to Brazil.
In addition to areas in Brazil where yellow fever vaccination has been recommended since before the recent outbreaks, the vaccine is now also recommended for people who are traveling to or living in:
- All of Espirito Santo State
- All of São Paulo State, the city of São Paulo and all coastal islands
- All of Rio de Janeiro State, including the city of Rio de Janeiro and all coastal islands
- A number of cities in Bahia State
Expanded Yellow Fever Vaccine Recommendation Areas in Brazil
The Brazilian Ministry of Health maintains a regular list of all other cities in Brazil for which yellow fever vaccination has been recommended since before the recent outbreaks. This list does not include recently added areas above. It is located at http://portalsaude.saude.gov.br/images/pdf/2015/novembro/19/Lista-de-Municipios-ACRV-Febre-Amarela-Set-2015.pdf.
What can travelers do to prevent yellow fever?
Get yellow fever vaccine
- Yellow fever vaccine is the best protection against yellow fever disease, which can be fatal. Anyone 9 months or older who travels to areas where yellow fever vaccine is recommended should be vaccinated against yellow fever at least 10 days before travel. For most travelers, one dose of yellow fever vaccine provides long-lasting protection. However, parts of Brazil are currently higher risk because of the outbreak. Travelers may consider getting a booster dose of yellow fever vaccine if traveling to areas with yellow fever outbreaks and it’s been 10 or more years since they were vaccinated. Areas with outbreaks include the states of Rio de Janeiro, Minas Gerais, and São Paulo.
People who have never been vaccinated against yellow fever for any reason should avoid traveling to areas of Brazil where yellow fever vaccination is recommended.
Yellow fever vaccine is currently available at only a limited number of clinics in the United States. Travelers should contact a yellow fever vaccine provider well in advance of travel. Search for a yellow fever vaccine provider near you(https://wwwnc.cdc.gov/travel/yellow-fever-vaccination-clinics/search).
Yellow fever vaccine is not recommended for some people. Talk with a health care provider if you have questions about the yellow fever vaccine.
Prevent insect bites
Because yellow fever and other diseases are spread by mosquito bites, all travelers to Brazil should prevent mosquito bites by using insect repellent, wearing long-sleeved shirts and pants when outdoors, and sleeping in an air-conditioned or well-screened room or under an insecticide-treated bed net.
If you get sick during or after travel
Talk to a doctor or nurse if you get sick, especially if you have a fever. Tell them you have been in a country with yellow fever.
Additional Information
Clinician Information
- Yellow Fever in CDC Health Information for International Travel (“Yellow Book”)
- Yellow Fever Vaccination: Information for Healthcare Professionals
- Yellow Fever Vaccine: Recommendations of the Advisory Committee on Immunization Practices (MMWR 2010)
- Yellow Fever Vaccine Booster Doses: Recommendations of the Advisory Committee on Immunization Practices, 2015
Disaster Telemedicine
Friday, March 23rd, 2018MedPage “…..I witnessed the potential first-hand in Puerto Rico after Maria. Less than two weeks after arriving at a location with no potable water and intermittent electrical power, my team had access to a live video link to an academic medical center in the mainland U.S. A specially outfitted laptop and an on-site satellite dish, along with a temperamental but functional generator, meant that my patients and I could communicate with specialists like pediatricians and psychiatrists — vital caregivers that were scarce on the island and unavailable to my team otherwise. We also faced some challenges: a glitchy connection, and a feeling that our tele-resources sometimes didn’t really match our real patients’ needs. Was it worth it? Mostly……”
Abstract
BACKGROUND:
Telemedicine and advanced technologies that ensure telepresence have become common practice and are an effective way of providing healthcare services.
MATERIALS AND METHODS:
The authors conducted a traditional narrative review of English literature through search engines (Medline, Pub Med, Embase, and Science Direct) using mesh terms “telemedicine,” “telepresence,” “earthquake,” “disaster,” “natural disaster,” and “man-made disaster” published between January 1, 1980 and September 30, 2013. For our analysis, only published studies were selected when telemedicine or telepresence was reported for disaster management, both in real life and in mock and simulation situations. Original articles, clinical trials, case presentations, and review articles were considered. Books and book chapters were used as well. Data from the International Disaster Database were included in the review to provide a sense of worldwide disaster occurrence. Symposia and other meetings were searched and used when available.
RESULTS:
Between January 1980 and September 2013, 17,565 disasters recorded. During this study period, 878 articles, chapters, books, and presentations were reported. Of these, only 88 articles and books fulfilled our selection criteria. Six articles described the effectiveness of telemedicine in mock simulations and disaster drills, and 63 presented the need and discussed how telemedicine would be beneficial in disaster response. Only 19 articles provided examples of effective use of telemedicine in disaster response. However, these studies demonstrated telemedicine as a valuable tool for communication between front-line humanitarian aid workers and expert physicians at remote locations.
CONCLUSION:
Telemedicine has not been used thus in the management of disasters, despite its great potential. There is an acute need for establishing telemedicine programs in high risk areas for disasters, so that when these disasters strike, existing telemedicine networks can be used, rather than attempting to bring solutions into a chaotic situation postevent
Today’s storm is the fourth serious snow to wallop the Northeast this month
Thursday, March 22nd, 2018Summary:
• A spring snowstorm is sweeping through the Northeast, the fourth nor’easter of the month.
• A foot or so of snow is expected from the suburbs of Philadelphia to parts of New York City to coastal Connecticut and Long Island, with significant snow from Washington to Boston.
• Nearly 5,000 flights have been canceled and La Guardia Airport suspended all flights.
• Boston schools will be closed.
• More than 35,000 homes in New Jersey have lost power.
NYC on a Thursday morning:
| Good morning on this slushy Thursday. |
| It’s time to get outside and start digging. |
| The spring snowstorm that pummeled our city yesterday shed its final flakes around dawn. At 8.2 inches, it broke one record but left others intact. But more on that in a bit. |
| First, here’s what you need to know before heading out: |
| (For the latest commute news, read New York Today online here.) |
| • New York City public schools are open. |
| • Public transit is up and running. The subway, Metro-North and Long Island Rail Road are operating on regular schedules but could face delays. |
| • New Jersey Transit trains, buses and light rail are operating on regular weekday schedules. Access Link will resume at noon and cross-honoring is not in effect. |
| • Amtrak is running on a modified schedule. |
| • It’s recovery day at the city’s airports. Kennedy, Newark and La Guardia are operational, but check your flight before you go. |
| • The streets are schmutzy. The Sanitation Department has dispatched nearly 1,600 plows since the start of the storm. You can see which streets were plowed, and when, with their plow tracker. |
| • Alternate-side parking rules are suspended for snow removal. Meters remain in effect. |
| With 12 to 18 inches of snow in the forecast, the nor’easter was expected to break the record for the largest spring snowstorm in our history. The previous record, of 10 inches, was set on April 3, 1915. A little after midnight, the ruler in Central Park read 8.2. |
| Your snow-shoveling experience may vary. The snow fell unevenly, dropping 11.7 inches in Bedford-Stuyvesant, 12 in Queens Village, 10 in Gramercy Park, and around 8.5 inches at both La Guardia and Kennedy. |
| “But Staten Island won the lottery,” said Patrick Maloit, a meteorologist at the National Weather Service. Port Richmond is waking up to 13.8 inches. |
| Even though parts of the city saw higher snow totals “the record is still going to the April storm,” Mr. Maloit said. Central Park is used for the official city total because record-keeping there is more extensive and “because, let’s face it, when you think New York City, you think Central Park, not La Guardia or Kennedy,” he said. |
| We did set one record yesterday, though. It was the most snow seen in New York on March 21. |
| And you can take comfort in knowing you lived through a spring snowstorm and the fourth nor’easter in one month, a super extra rare occurrence. The National Weather Service found at least one other instance of four nor’easters taking place in one month — between Dec. 30, 1986, and Jan. 26, 1987 — but that was in the dead of winter. |
| We’d advise against placing any bets on a fifth: Another big nor’easter this season is unlikely, and temperatures are expected to keep climbing in the coming weeks. |
| Today, cloudy with a high near 42. Tomorrow, drizzly, with a high of 44. |
Five Thai migrant workers have been found to be suffering from parasites that can cause meningitis or even blindness after eating raw snails
Thursday, March 22nd, 2018“…..Angiostrongylus cantonensis is mainly found in uncooked snails and slugs, as well as contaminated water sources and lettuce, according to the CDC. The parasite commonly invades the brain and spinal cord, causing various neurological symptoms.
Patients often suffer from meningitis, commonly leading to acute sever headaches. Fever, vomiting, nausea, neck pain and stiffness are some of the other symptoms seen, and the parasite can even cause blindness if it invades a person’s eyeball.….”
Tsai HC1, Chen YS, Yen CM. Human parasitic meningitis caused by
_Angiostrongylus cantonensis_ Infection in Taiwan. Hawaii J Med Public
Health. 2013; 72(6 Suppl 2): 26-7; available at
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689489/>
March 22: World Water Day
Thursday, March 22nd, 2018World Water Day is observed each year on March 22 to promote the responsible use of water and access to safe water for everyone. Around the world, 844 million people still do not have a basic drinking water service.1
Water is one of our most important natural resources. Every day, people, animals, and plants depend on water for their survival. Water is necessary for growing food, energy production, individual well-being, and global health.
Waterborne Disease Prevention Around the World
Clean and safe drinking water sustains human life. Without it, waterborne diseases can spread, sickening and sometimes killing adults and children. CDC’s Global Water, Sanitation, and Hygiene (WASH) experts work to improve global access to safe water, proper sanitation, and hygiene. CDC experts strengthen WASH efforts in response to humanitarian crises and natural disasters and respond to life-threatening outbreaks of waterborne diseases around the world, including outbreaks of cholera, hepatitis, and typhoid fever. CDC also works closely with other U.S. government agencies, foreign Ministries of Health, non-governmental organizations, UN Agencies, private companies, and various international agencies to improve global access to healthy and safe water, proper sanitation, and hygiene.
The United Nations established a sustainable development goal of improving access to safe water and sanitation facilities. Between 2000 and 2015, over 1 billion people gained access to piped water supplies with the potential to deliver safe water for everyday use (for example, tap water in households or public stand posts that provide piped water). Between 1990 and 2015, more than 2 billion people gained access to an improved sanitation facility (a toilet or latrine designed to ensure that people do not come in contact with waste). Despite these improvements, 844 million people still did not have access to a safe drinking water source, and 2.3 billion still did not have access to an improved sanitation facility. Some 892 million people defecate in the open because they do not have access to any type of toilet or latrine.1
Lack of safe drinking water and toilets increases the chance for outbreaks of waterborne diseases like typhoid fever, hepatitis, and cholera. Typhoid, hepatitis, and cholera germs can spread when human waste containing the germs gets into a community’s water supply. That happens when people do not have access to a sanitation facility that can dispose of waste properly. Although rare in the United States, outbreaks of cholera and typhoid continue to occur in low resource countries. Together, these diseases kill from 149,000 to 304,000 men, women, and children each year.2,3
Now is the time to address these challenges to keep the global water supply safe and available for generations to come.
Visit the United Nations’ World Water Day website for more information on World Water Day and ideas on how to get involved.
World Water Day also presents an opportunity to learn about water-related issues that affect us locally. For more information about CDC’s water-related public health efforts in the United States, visit these websites: Drinking Water, Water, Sanitation, and Hygiene-Related Emergency; and Healthy Swimming.
More Information
- World Water Day
- CDC’s Global Water, Sanitation, and Hygiene Website
- CDC’s Safe Water System
- CDC’s Environmental Health Global Water, Sanitation, and Hygiene Website
- CDC’s Global Disease Detection and Emergency Response Website
- CDC and the U.S. Global Health Initiative
- CDC’s Healthy Water Website
- I Am CDC – Anu Rajasingham
References
- UNICEF and World Health Organization. Progress on Drinking Water, Sanitation and Hygiene—2017 Update and SDG Baselines.[4.82 MB] Geneva, Switzerland: World Health Organization; 2017.
- World Health Organization. Cholera Fact Sheet. December 2017
- World Health Organization. Typhoid Fact Sheet. January 2018
- World Health Organization. Hepatitis E Fact Sheet. July 2017
Kabul, Afghanistan: A suicide bomber detonated himself in front of the Ali Abad Hospital, killing 29 and wounding 52
Wednesday, March 21st, 2018“……At the Ali Abad Hospital, there were angry, emotional scenes as families tried to recover the bodies of loved ones, many of them mangled and dismembered.….”


 CDC: “…
CDC: “…