Archive for November, 2018
Reports of 11 more Escherichia coli O157:H7 illnesses linked to the Romaine lettuce outbreak.
Wednesday, November 28th, 2018Based on new information, CDC is narrowing its warning to consumers. CDC is advising that U.S. consumers not eat and retailers and restaurants not serve or sell any romaine lettuce harvested from the Central Coastal growing regions of northern and central California. If you do not know where the romaine is from, do not eat it.
- Romaine lettuce products will be labeled with a harvest location by region. It may take some time before these labels are available.
- If the romaine lettuce is not labeled with a harvest growing region, do not buy, serve, sell, or eat it.
- Check bags or boxes of romaine lettuce for a label indicating where the lettuce was harvested. Romaine lettuce labeled with a harvest region outside of the Central Coastal growing regions of northern and central California (such as the desert growing region near Yuma, the California desert growing region near Imperial County and Riverside County, the state of Florida, and Mexico) is not linked to this outbreak.
- If you do not know where your romaine lettuce was harvested, do not eat it and throw it away.
- This advice includes all types or uses of romaine lettuce, such as whole heads of romaine, hearts of romaine, and bags and boxes of precut lettuce and salad mixes that contain romaine, including baby romaine, spring mix, and Caesar salad.
- If you do not know if the lettuce is romaine or whether a salad mix contains romaine, do not eat it and throw it away.
- Wash and sanitize drawers or shelves in refrigerators where romaine was stored. Follow these five steps to clean your refrigerator.
- Restaurants and retailers should check the label on bags or boxes of romaine lettuce, or ask their suppliers about the source of their romaine lettuce.
- Do not sell or serve any romaine lettuce harvested from the Central Coastal growing regions of northern and central California.
- If you do not know where your romaine lettuce was harvested, do not sell or serve it.
- Hydroponically or greenhouse-grown romaine lettuce has not been linked to this outbreak.
- Take action if you have symptoms of an E. coli infection:
- Talk to your healthcare provider.
- Write down what you ate in the week before you started to get sick.
- Report your illness to the health department.
- Assist public health investigators by answering questions about your illness.
Advice to Clinicians
- Antibiotics are not recommended for patients with E. coli O157 infections. Antibiotics are also not recommended for patients in whom E.coli O157 infection is suspected, until diagnostic testing rules out this infection.
- Some studies have shown that administering antibiotics to patients with E. coli O157 infections might increase their risk of developing hemolytic uremic syndrome (a type of kidney failure), and the benefit of antibiotic treatment has not been clearly demonstrated.
Latest Outbreak Information

At A Glance
- Reported Cases: 43
- States: 12
- Hospitalizations: 16
- Deaths: 0
- Recall: No
- Since the last update on November 20, an additional 11 ill people have been included in this investigation.
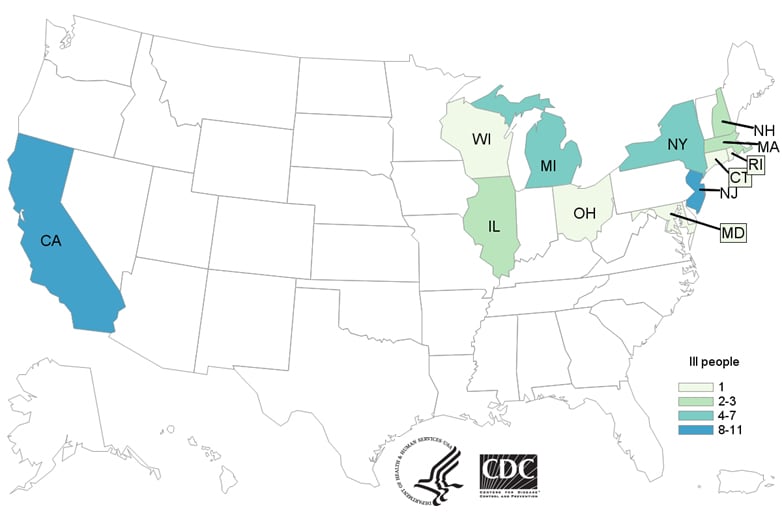
- Forty-three people infected with the outbreak strain of Shiga toxin-producing E. coli O157:H7 have been reported from 12 states.
- Illnesses started on dates ranging from October 8, 2018 to October 31, 2018.
- Sixteen people have been hospitalized, including one person who developed hemolytic uremic syndrome, a type of kidney failure. No deaths have been reported.
- The Public Health Agency of Canada has identified ill people infected with the same DNA fingerprint of E. coli O157:H7 bacteria in Canada.
- Epidemiologic and traceback evidence from the United States and Canada indicates that romaine lettuce harvested from the Central Coastal growing regions of northern and central California is a likely source of the outbreak.
- Ill people in this outbreak were infected with E. coli bacteria with the same DNA fingerprint as the E. coli strain isolated from ill people in a 2017 outbreak linked to leafy greens in the United States and to romaine lettuce in Canada. The current outbreak is not related to a spring 2018 multistate outbreak of E. coli O157:H7 infections linked to romaine lettuce.
- CDC is advising that consumers not eat any romaine lettuce harvested from the Central Coastal growing regions of northern and central California. No common grower, supplier, distributor, or brand of romaine lettuce has been identified.
- This investigation is ongoing, and CDC will provide more information as it becomes available.
Symptoms of E. coli Infection

- People usually get sick from Shiga toxin-producing E. coli (STEC) 2–8 days (average of 3–4 days) after swallowing the germ.
- Some people with a STEC infection may get a type of kidney failure called hemolytic uremic syndrome (HUS).
- E. coli infection is usually diagnosed by testing a stool sample.
- Antibiotics are not recommended for patients with suspected E. coli infections until diagnostic testing can be performed and E. coli infection is ruled out. Some studies have shown that administering antibiotics to patients with E. coli infections might increase their risk of developing HUS, and a benefit of treatment has not been clearly demonstrated.
- For more information, see Symptoms of E. coli Infection.
Investigation Details
November 26, 2018
CDC, public health and regulatory officials in several states, Canada, and the FDA are investigating a multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (E. coli O157:H7) infections.
As of November 26, 2018, 43 people infected with the outbreak strain of E. coli O157:H7 have been reported from 12 states. A list of the states and the number of cases in each can be found on the Map of Reported Cases page.
Illnesses started on dates ranging from October 8, 2018 to October 31, 2018. Ill people range in age from 1 to 84 years, with a median age of 25. Sixty-nine percent of ill people are female. Of 38 people with information available, 16 (42%) have been hospitalized, including one person who developed hemolytic uremic syndrome, a type of kidney failure. No deaths have been reported.
Illnesses that occurred after October 31, 2018, might not yet be reported due to the time it takes between when a person becomes ill with E. coli infection and when the illness is reported. This takes an average of two to three weeks.
Investigation of the Outbreak
Epidemiologic and traceback evidence indicates that romaine lettuce from the Central Coastal growing regions of northern and central California is a likely source of this outbreak.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. Twenty-two (88%) of 25 people interviewed reported eating romaine lettuce. This percentage is significantly higher than results from a survey[PDF – 787 KB] of healthy people in which 47% reported eating romaine lettuce in the week before they were interviewed. Ill people reported eating different types of romaine lettuce in several restaurants and at home.
Preliminary traceback information from the FDA indicates that ill people in this outbreak ate romaine lettuce harvested from the Central Coastal growing regions of northern and central California. At this time, no common grower, supplier, distributor, or brand of romaine lettuce has been identified. CDC is advising that consumers not eat and restaurants and retailers not sell any romaine lettuce from the Central Coastal growing regions of northern and central California.
This investigation is ongoing, and CDC will provide more information as it becomes available.
Statement from FDA Commissioner Scott Gottlieb, M.D., on the current romaine lettuce E. coli O157:H7 outbreak investigation
Tuesday, November 27th, 2018For Immediate Release
November 26, 2018
Statement
The U.S. Food and Drug Administration, along with the Centers for Disease Control and Prevention and state authorities, continues to investigate a multistate outbreak of E. coli O157:H7 infections associated with consumption of romaine lettuce in the U.S. As of Nov. 26, 2018, this outbreak has resulted in 43 people becoming ill in 12 states, with the last reported illness onset date being Oct. 31, 2018. An additional 22 people in Canada have become ill, and the FDA and our partners are also coordinating the investigation with Canadian health and food safety authorities.
As we continue to investigate this outbreak, today the FDA is announcing new steps to help consumers better identify where their romaine is grown through voluntary labeling.
To prevent additional cases of E. coli O157:H7, on Nov. 20, 2018 the CDC advised the public not to consume romaine lettuce and to destroy any romaine lettuce in their homes. At the same time, the FDA requested that all romaine lettuce on the market, including in restaurants and other commercial establishments, should be withdrawn and destroyed. The FDA made this request because initial information available at that time had not identified a likely source for the outbreak that would allow a targeted request, it was likely romaine lettuce contaminated with E. coli O157:H7 that could cause illness was still available on the market, and a market withdrawal was the fastest way to remove potentially contaminated product. The romaine lettuce industry agreed to comply with the FDA’s request to withdraw any romaine lettuce on the market on that date, and available information suggests this action was effective in removing potentially contaminated romaine lettuce from retail establishments.
Over the Thanksgiving holiday, the FDA continued to investigate the outbreak. Our investigation at this point suggests that romaine lettuce associated with the outbreak comes from areas of California that grow romaine lettuce over the summer months, and that the outbreak appears to be related to “end of season” romaine lettuce harvested from these areas. The involved areas include the Central Coast growing regions of central and northern California.
The FDA is continuing tracebacks of romaine lettuce from locations where impacted consumers purchased or consumed romaine lettuce before they became ill in order to identify specific locations that are the likely source of the outbreak and to determine the factors that resulted in contamination. Through laboratory studies we have identified that the E. coli O157:H7 strain causing the outbreak is similar to one that produced an outbreak of E. coli O157:H7 in the fall of 2017 that also occurred in the U.S. and Canada, which was associated with consumption of leafy greens in the U.S. and specifically romaine lettuce in Canada.
Based on further discussions with the leafy greens industry and with agricultural authorities, we have begun to narrow the location in which we believe the contaminated romaine in the current outbreak was grown. At the time of the outbreak, the vast majority of the romaine on the market was being grown in the Central Coast region of California. Since, then harvesting of romaine lettuce from this region has ended for the year. Growing and harvesting of romaine lettuce is now shifting to the winter growing regions of the U.S., which include mainly the California desert region of the Imperial Valley, the desert region of Arizona in and around Yuma, and Florida. Romaine lettuce grown in Mexico is exported to the U.S. during the winter months. Smaller quantities of romaine lettuce are grown in other states. At this time, the FDA has no information to suggest any of these growing areas are involved in the current outbreak, which began well before any romaine lettuce from these winter growing locations was available for harvest. In addition, hydroponic romaine lettuce and romaine lettuce grown in green-houses is also marketed in the U.S., but there is no information to suggest these products are implicated in any identified E. coli O157:H7 outbreak.
The FDA believes it was critically important to have a “clean break” in the romaine supply available to consumers in the U.S. in order to purge the market of potentially contaminated romaine lettuce related to the current outbreak. This appears to have been accomplished through the market withdrawal request of Nov. 20, 2018.
Knowing the growing origin of produce will continue to play an important role in allowing consumers to avoid contaminated products and facilitating market withdrawals and tracebacks. That’s why we previously called on the romaine lettuce industry to provide unambiguous and clear information to consumers regarding where their lettuce was grown and when it was harvested.
To this end, the FDA recently participated in discussions with the major producers and distributors of romaine lettuce in the U.S. and with the major trade associations representing the produce industry regarding product labeling and dating to assure consumers that any romaine lettuce that will come onto the market is not associated with the current outbreak of E. coli O157:H7. The labeling will identify the origin of the romaine based on harvest region, along with the date of harvest. This can improve the ability of the FDA to provide more targeted information to consumers in the event of a future outbreak of illness. The FDA also has commitments from the romaine lettuce industry that such labeling will continue into the future and become the standard for their products.
In addition, the leafy greens industry has agreed to establish a task force to find solutions for long term labeling of romaine lettuce and other leafy greens for helping to identify products and to put in place standards for traceability of product. The task force will also examine information from this outbreak to identify measures that led to its occurrence and how to prevent ongoing safety problems with romaine lettuce. One outcome could be to extend the commitment for labeling for origin and date of harvest to other leafy greens.
Therefore, the FDA is issuing the following updated advice as part of our investigation and public warning:
Based on discussions with major producers and distributors, romaine lettuce entering the market will now be labeled with a harvest location and a harvest date. Romaine lettuce entering the market can also be labeled as being hydroponically or greenhouse grown. If it does not have this information, you should not eat or use it.
If consumers, retailers, and food service facilities are unable to identify that romaine lettuce products are not affected – which means determining that the products were grown outside the California regions that appear to be implicated in the current outbreak investigation — we urge that these products not be purchased, or if purchased, be discarded or returned to the place of purchase.
Romaine lettuce that was harvested outside of the Central Coast growing regions of northern and central California does not appear to be related to the current outbreak. Hydroponically- and greenhouse-grown romaine also does not appear to be related to the current outbreak. There is no recommendation for consumers or retailers to avoid using romaine harvested from these sources.
The FDA has urged growers, processors, distributors and retailers to:
- clearly and prominently label all individually packaged romaine products to identify growing region and harvest date for romaine; and
- clearly and prominently label at the point of sale the growing region when it is not possible for romaine lettuce suppliers to label the package (e.g. individual unwrapped whole heads of romaine lettuce available in retail stores).
We hope that growers, processors, distributors and retailers will join us in our effort to protect consumers by applying these labeling recommendations to their products. We remain committed to identifying ways to decrease the incidence and impact of foodborne illness outbreaks, and will continue to provide updates on our investigation and changes to our advice on romaine lettuce as more information becomes available.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
###
The Camp Fire’s death toll has increased to 88, with 203 remain missing
Tuesday, November 27th, 2018“……The wildfire, the deadliest and most destructive in California’s history, was contained on Sunday after burning for 17 days. It ravaged 153,336 acres (240 square miles). …..”
The National Climate Assessment (NCA) assesses the science of climate change and variability and its impacts across the United States, now and throughout this century.
Monday, November 26th, 2018Fourth National Climate Change Report
FOURTH NATIONAL CLIMATE ASSESSMENT
Summary Findings
These Summary Findings represent a high-level synthesis of the material in the underlying report. The findings consolidate Key Messages and supporting evidence from 16 national-level topic chapters, 10 regional chapters, and 2 chapters that focus on societal response strategies (mitigation and adaptation). Unless otherwise noted, qualitative statements regarding future conditions in these Summary Findings are broadly applicable across the range of different levels of future climate change and associated impacts considered in this report.
1. Communities
Climate change creates new risks and exacerbates existing vulnerabilities in communities across the United States, presenting growing challenges to human health and safety, quality of life, and the rate of economic growth.
The impacts of climate change are already being felt in communities across the country. More frequent and intense extreme weather and climate-related events, as well as changes in average climate conditions, are expected to continue to damage infrastructure, ecosystems, and social systems that provide essential benefits to communities. Future climate change is expected to further disrupt many areas of life, exacerbating existing challenges to prosperity posed by aging and deteriorating infrastructure, stressed ecosystems, and economic inequality. Impacts within and across regions will not be distributed equally. People who are already vulnerable, including lower-income and other marginalized communities, have lower capacity to prepare for and cope with extreme weather and climate-related events and are expected to experience greater impacts. Prioritizing adaptation actions for the most vulnerable populations would contribute to a more equitable future within and across communities. Global action to significantly cut greenhouse gas emissions can substantially reduce climate-related risks and increase opportunities for these populations in the longer term.
2. Economy
Without substantial and sustained global mitigation and regional adaptation efforts, climate change is expected to cause growing losses to American infrastructure and property and impede the rate of economic growth over this century.
In the absence of significant global mitigation action and regional adaptation efforts, rising temperatures, sea level rise, and changes in extreme events are expected to increasingly disrupt and damage critical infrastructure and property, labor productivity, and the vitality of our communities. Regional economies and industries that depend on natural resources and favorable climate conditions, such as agriculture, tourism, and fisheries, are vulnerable to the growing impacts of climate change. Rising temperatures are projected to reduce the efficiency of power generation while increasing energy demands, resulting in higher electricity costs. The impacts of climate change beyond our borders are expected to increasingly affect our trade and economy, including import and export prices and U.S. businesses with overseas operations and supply chains. Some aspects of our economy may see slight near-term improvements in a modestly warmer world. However, the continued warming that is projected to occur without substantial and sustained reductions in global greenhouse gas emissions is expected to cause substantial net damage to the U.S. economy throughout this century, especially in the absence of increased adaptation efforts. With continued growth in emissions at historic rates, annual losses in some economic sectors are projected to reach hundreds of billions of dollars by the end of the century—more than the current gross domestic product (GDP) of many U.S. states.
3. Interconnected Impacts
Climate change affects the natural, built, and social systems we rely on individually and through their connections to one another. These interconnected systems are increasingly vulnerable to cascading impacts that are often difficult to predict, threatening essential services within and beyond the Nation’s borders.
Climate change presents added risks to interconnected systems that are already exposed to a range of stressors such as aging and deteriorating infrastructure, land-use changes, and population growth. Extreme weather and climate-related impacts on one system can result in increased risks or failures in other critical systems, including water resources, food production and distribution, energy and transportation, public health, international trade, and national security. The full extent of climate change risks to interconnected systems, many of which span regional and national boundaries, is often greater than the sum of risks to individual sectors. Failure to anticipate interconnected impacts can lead to missed opportunities for effectively managing the risks of climate change and can also lead to management responses that increase risks to other sectors and regions. Joint planning with stakeholders across sectors, regions, and jurisdictions can help identify critical risks arising from interaction among systems ahead of time.
4. Actions to Reduce Risks
Communities, governments, and businesses are working to reduce risks from and costs associated with climate change by taking action to lower greenhouse gas emissions and implement adaptation strategies. While mitigation and adaptation efforts have expanded substantially in the last four years, they do not yet approach the scale considered necessary to avoid substantial damages to the economy, environment, and human health over the coming decades.
Future risks from climate change depend primarily on decisions made today. The integration of climate risk into decision-making and the implementation of adaptation activities have significantly increased since the Third National Climate Assessment in 2014, including in areas of financial risk reporting, capital investment planning, development of engineering standards, military planning, and disaster risk management. Transformations in the energy sector—including the displacement of coal by natural gas and increased deployment of renewable energy—along with policy actions at the national, regional, state, and local levels are reducing greenhouse gas emissions in the United States. While these adaptation and mitigation measures can help reduce damages in a number of sectors, this assessment shows that more immediate and substantial global greenhouse gas emissions reductions, as well as regional adaptation efforts, would be needed to avoid the most severe consequences in the long term. Mitigation and adaptation actions also present opportunities for additional benefits that are often more immediate and localized, such as improving local air quality and economies through investments in infrastructure. Some benefits, such as restoring ecosystems and increasing community vitality, may be harder to quantify.
5. Water
The quality and quantity of water available for use by people and ecosystems across the country are being affected by climate change, increasing risks and costs to agriculture, energy production, industry, recreation, and the environment.
Rising air and water temperatures and changes in precipitation are intensifying droughts, increasing heavy downpours, reducing snowpack, and causing declines in surface water quality, with varying impacts across regions. Future warming will add to the stress on water supplies and adversely impact the availability of water in parts of the United States. Changes in the relative amounts and timing of snow and rainfall are leading to mismatches between water availability and needs in some regions, posing threats to, for example, the future reliability of hydropower production in the Southwest and the Northwest. Groundwater depletion is exacerbating drought risk in many parts of the United States, particularly in the Southwest and Southern Great Plains. Dependable and safe water supplies for U.S. Caribbean, Hawai‘i, and U.S.-Affiliated Pacific Island communities are threatened by drought, flooding, and saltwater contamination due to sea level rise. Most U.S. power plants rely on a steady supply of water for cooling, and operations are expected to be affected by changes in water availability and temperature increases. Aging and deteriorating water infrastructure, typically designed for past environmental conditions, compounds the climate risk faced by society. Water management strategies that account for changing climate conditions can help reduce present and future risks to water security, but implementation of such practices remains limited.
6. Health
Impacts from climate change on extreme weather and climate-related events, air quality, and the transmission of disease through insects and pests, food, and water increasingly threaten the health and well-being of the American people, particularly populations that are already vulnerable.
Changes in temperature and precipitation are increasing air quality and health risks from wildfire and ground-level ozone pollution. Rising air and water temperatures and more intense extreme events are expected to increase exposure to waterborne and foodborne diseases, affecting food and water safety. With continued warming, cold-related deaths are projected to decrease and heat-related deaths are projected to increase; in most regions, increases in heat-related deaths are expected to outpace reductions in cold-related deaths. The frequency and severity of allergic illnesses, including asthma and hay fever, are expected to increase as a result of a changing climate. Climate change is also projected to alter the geographic range and distribution of disease-carrying insects and pests, exposing more people to ticks that carry Lyme disease and mosquitoes that transmit viruses such as Zika, West Nile, and dengue, with varying impacts across regions. Communities in the Southeast, for example, are particularly vulnerable to the combined health impacts from vector-borne disease, heat, and flooding. Extreme weather and climate-related events can have lasting mental health consequences in affected communities, particularly if they result in degradation of livelihoods or community relocation. Populations including older adults, children, low-income communities, and some communities of color are often disproportionately affected by, and less resilient to, the health impacts of climate change. Adaptation and mitigation policies and programs that help individuals, communities, and states prepare for the risks of a changing climate reduce the number of injuries, illnesses, and deaths from climate-related health outcomes.
7. Indigenous Peoples
Climate change increasingly threatens Indigenous communities’ livelihoods, economies, health, and cultural identities by disrupting interconnected social, physical, and ecological systems.
Many Indigenous peoples are reliant on natural resources for their economic, cultural, and physical well-being and are often uniquely affected by climate change. The impacts of climate change on water, land, coastal areas, and other natural resources, as well as infrastructure and related services, are expected to increasingly disrupt Indigenous peoples’ livelihoods and economies, including agriculture and agroforestry, fishing, recreation, and tourism. Adverse impacts on subsistence activities have already been observed. As climate changes continue, adverse impacts on culturally significant species and resources are expected to result in negative physical and mental health effects. Throughout the United States, climate-related impacts are causing some Indigenous peoples to consider or actively pursue community relocation as an adaptation strategy, presenting challenges associated with maintaining cultural and community continuity. While economic, political, and infrastructure limitations may affect these communities’ ability to adapt, tightly knit social and cultural networks present opportunities to build community capacity and increase resilience. Many Indigenous peoples are taking steps to adapt to climate change impacts structured around self-determination and traditional knowledge, and some tribes are pursuing mitigation actions through development of renewable energy on tribal lands.
8. Ecosystems and Ecosystem Services
Ecosystems and the benefits they provide to society are being altered by climate change, and these impacts are projected to continue. Without substantial and sustained reductions in global greenhouse gas emissions, transformative impacts on some ecosystems will occur; some coral reef and sea ice ecosystems are already experiencing such transformational changes.
Many benefits provided by ecosystems and the environment, such as clean air and water, protection from coastal flooding, wood and fiber, crop pollination, hunting and fishing, tourism, cultural identities, and more will continue to be degraded by the impacts of climate change. Increasing wildfire frequency, changes in insect and disease outbreaks, and other stressors are expected to decrease the ability of U.S. forests to support economic activity, recreation, and subsistence activities. Climate change has already had observable impacts on biodiversity, ecosystems, and the benefits they provide to society. These impacts include the migration of native species to new areas and the spread of invasive species. Such changes are projected to continue, and without substantial and sustained reductions in global greenhouse gas emissions, extinctions and transformative impacts on some ecosystems cannot be avoided in the long term. Valued aspects of regional heritage and quality of life tied to ecosystems, wildlife, and outdoor recreation will change with the climate, and as a result, future generations can expect to experience and interact with the natural environment in ways that are different from today. Adaptation strategies, including prescribed burning to reduce fuel for wildfire, creation of safe havens for important species, and control of invasive species, are being implemented to address emerging impacts of climate change. While some targeted response actions are underway, many impacts, including losses of unique coral reef and sea ice ecosystems, can only be avoided by significantly reducing global emissions of carbon dioxide and other greenhouse gases.
9. Agriculture
Rising temperatures, extreme heat, drought, wildfire on rangelands, and heavy downpours are expected to increasingly disrupt agricultural productivity in the United States. Expected increases in challenges to livestock health, declines in crop yields and quality, and changes in extreme events in the United States and abroad threaten rural livelihoods, sustainable food security, and price stability.
Climate change presents numerous challenges to sustaining and enhancing crop productivity, livestock health, and the economic vitality of rural communities. While some regions (such as the Northern Great Plains) may see conditions conducive to expanded or alternative crop productivity over the next few decades, overall, yields from major U.S. crops are expected to decline as a consequence of increases in temperatures and possibly changes in water availability, soil erosion, and disease and pest outbreaks. Increases in temperatures during the growing season in the Midwest are projected to be the largest contributing factor to declines in the productivity of U.S. agriculture. Projected increases in extreme heat conditions are expected to lead to further heat stress for livestock, which can result in large economic losses for producers. Climate change is also expected to lead to large-scale shifts in the availability and prices of many agricultural products across the world, with corresponding impacts on U.S. agricultural producers and the U.S. economy. These changes threaten future gains in commodity crop production and put rural livelihoods at risk. Numerous adaptation strategies are available to cope with adverse impacts of climate variability and change on agricultural production. These include altering what is produced, modifying the inputs used for production, adopting new technologies, and adjusting management strategies. However, these strategies have limits under severe climate change impacts and would require sufficient long- and short-term investment in changing practices.
10. Infrastructure
Our Nation’s aging and deteriorating infrastructure is further stressed by increases in heavy precipitation events, coastal flooding, heat, wildfires, and other extreme events, as well as changes to average precipitation and temperature. Without adaptation, climate change will continue to degrade infrastructure performance over the rest of the century, with the potential for cascading impacts that threaten our economy, national security, essential services, and health and well-being.
Climate change and extreme weather events are expected to increasingly disrupt our Nation’s energy and transportation systems, threatening more frequent and longer-lasting power outages, fuel shortages, and service disruptions, with cascading impacts on other critical sectors. Infrastructure currently designed for historical climate conditions is more vulnerable to future weather extremes and climate change. The continued increase in the frequency and extent of high-tide flooding due to sea level rise threatens America’s trillion-dollar coastal property market and public infrastructure, with cascading impacts to the larger economy. In Alaska, rising temperatures and erosion are causing damage to buildings and coastal infrastructure that will be costly to repair or replace, particularly in rural areas; these impacts are expected to grow without adaptation. Expected increases in the severity and frequency of heavy precipitation events will affect inland infrastructure in every region, including access to roads, the viability of bridges, and the safety of pipelines. Flooding from heavy rainfall, storm surge, and rising high tides is expected to compound existing issues with aging infrastructure in the Northeast. Increased drought risk will threaten oil and gas drilling and refining, as well as electricity generation from power plants that rely on surface water for cooling. Forward-looking infrastructure design, planning, and operational measures and standards can reduce exposure and vulnerability to the impacts of climate change and reduce energy use while providing additional near-term benefits, including reductions in greenhouse gas emissions.
11. Oceans & Coasts
Coastal communities and the ecosystems that support them are increasingly threatened by the impacts of climate change. Without significant reductions in global greenhouse gas emissions and regional adaptation measures, many coastal regions will be transformed by the latter part of this century, with impacts affecting other regions and sectors. Even in a future with lower greenhouse gas emissions, many communities are expected to suffer financial impacts as chronic high-tide flooding leads to higher costs and lower property values.
Rising water temperatures, ocean acidification, retreating arctic sea ice, sea level rise, high-tide flooding, coastal erosion, higher storm surge, and heavier precipitation events threaten our oceans and coasts. These effects are projected to continue, putting ocean and marine species at risk, decreasing the productivity of certain fisheries, and threatening communities that rely on marine ecosystems for livelihoods and recreation, with particular impacts on fishing communities in Hawai‘i and the U.S.-Affiliated Pacific Islands, the U.S. Caribbean, and the Gulf of Mexico. Lasting damage to coastal property and infrastructure driven by sea level rise and storm surge is expected to lead to financial losses for individuals, businesses, and communities, with the Atlantic and Gulf Coasts facing above-average risks. Impacts on coastal energy and transportation infrastructure driven by sea level rise and storm surge have the potential for cascading costs and disruptions across the country. Even if significant emissions reductions occur, many of the effects from sea level rise over this centuryand particularly through mid-centuryare already locked in due to historical emissions, and many communities are already dealing with the consequences. Actions to plan for and adapt to more frequent, widespread, and severe coastal flooding, such as shoreline protection and conservation of coastal ecosystems, would decrease direct losses and cascading impacts on other sectors and parts of the country. More than half of the damages to coastal property are estimated to be avoidable through well-timed adaptation measures. Substantial and sustained reductions in global greenhouse gas emissions would also significantly reduce projected risks to fisheries and communities that rely on them.
12. Tourism and Recreation
Outdoor recreation, tourist economies, and quality of life are reliant on benefits provided by our natural environment that will be degraded by the impacts of climate change in many ways.
Climate change poses risks to seasonal and outdoor economies in communities across the United States, including impacts on economies centered around coral reef-based recreation, winter recreation, and inland water-based recreation. In turn, this affects the well-being of the people who make their living supporting these economies, including rural, coastal, and Indigenous communities. Projected increases in wildfire smoke events are expected to impair outdoor recreational activities and visibility in wilderness areas. Declines in snow and ice cover caused by warmer winter temperatures are expected to negatively impact the winter recreation industry in the Northwest, Northern Great Plains, and the Northeast. Some fish, birds, and mammals are expected to shift where they live as a result of climate change, with implications for hunting, fishing, and other wildlife-related activities. These and other climate-related impacts are expected to result in decreased tourism revenue in some places and, for some communities, loss of identity. While some new opportunities may emerge from these ecosystem changes, cultural identities and economic and recreational opportunities based around historical use of and interaction with species or natural resources in many areas are at risk. Proactive management strategies, such as the use of projected stream temperatures to set priorities for fish conservation, can help reduce disruptions to tourist economies and recreation.
M 6.3 Earthquake: 20km SSW of Sarpol-e Zahab, Iran with at least 200 injured so far
Sunday, November 25th, 2018Tectonic Summary
Seismotectonics of the Middle East and Vicinity
No fewer than four major tectonic plates (Arabia, Eurasia, India, and Africa) and one smaller tectonic block (Anatolia) are responsible for seismicity and tectonics in the Middle East and surrounding region. Geologic development of the region is a consequence of a number of first-order plate tectonic processes that include subduction, large-scale transform faulting, compressional mountain building and crustal extension.

Mountain building in northern Pakistan and Afghanistan is the result of compressional tectonics associated with collision of the India plate moving northwards at a rate of 40 mm/yr with respect to the Eurasia plate. Continental thickening of the northern and western edge of the India subcontinent has produced the highest mountains in the world, including the Himalayan, Karakoram, Pamir and Hindu Kush ranges. Earthquake activity and faulting found in this region, as well as adjacent parts of Afghanistan and India, are due to collisional plate tectonics.
Beneath the Pamir-Hindu Kush Mountains of northern Afghanistan, earthquakes occur to depths as great as 200 km as a result of remnant lithospheric subduction. Shallower crustal earthquakes in the Pamir-Hindu Mountains occur primarily along the Main Pamir Thrust and other active Quaternary faults, which accommodate much of the region’s crustal shortening. The western and eastern margins of the Main Pamir Thrust display a combination of thrust and strike-slip mechanisms.
Along the western margin of the Tibetan Plateau, in the vicinity of southeastern Afghanistan and western Pakistan, the India plate translates obliquely relative to the Eurasia plate, resulting in a complex fold-and-thrust belt known as the Sulaiman Range. Faulting in this region includes strike-slip, reverse-slip and oblique-slip motion and often results in shallow, destructive earthquakes. The relatively fast moving left-lateral, strike-slip Chaman Fault system in southeastern Afghanistan accommodates translational motion between the India and Eurasia plates. In 1505, a segment of the Chaman Fault system near Kabul, Afghanistan ruptured causing widespread destruction of Kabul and surrounding villages. In the same region, the more recent 30 May 1935, M7.6 Quetta, Pakistan earthquake, occurred within the Sulaiman Range, killing between 30,000 and 60,000 people.
Off the south coast of Pakistan and southeast coast of Iran, the Makran trench is the present-day surface expression of active subduction of the Arabia plate beneath the continental Eurasia plate, which converge at a rate of approximately 20 mm/yr. Although the Makran subduction zone has a relatively slow convergence rate, it has produced large devastating earthquakes and tsunamis. For example, the November 27, 1945 M8.0 mega-thrust earthquake produced a tsunami within the Gulf of Oman and Arabia Sea, killing over 4,000 people. Northwest of this active subduction zone, collision of the Arabia and Eurasia plates forms the approximately 1,500-km-long fold and thrust belt of the Zagros Mountains, which crosses the whole of western Iran and extends into northeastern Iraq. Collision of the Arabia and Eurasia plates also causes crustal shortening in the Alborz Mountains and Kopet Dag in northern Iran. Eastern Iran experiences destructive earthquakes that originate on both strike-slip and reverse faults. For example, the 16 September 1978 M7.8 earthquake, along the southwest edge of the Dasht-e-Lut Basin killed at least 15,000 people.
Along the eastern margin of the Mediterranean region there is complex interaction between the Africa, Arabia and Eurasia plates. The Red Sea Rift is a spreading center between the Africa and Arabia plates, with a spreading rate of approximately 10mm/yr near its northern end, and 16mm/yr near its southern end (Chu, D. and Gordon, R. G., 1998). Seismicity rate and size of earthquakes has been relatively small along the spreading center, but the rifting process has produced a series of volcanic systems across western Saudi Arabia.
Further north, the Red Sea Rift terminates at the southern boundary of the Dead Sea Transform Fault. The Dead Sea Transform is a strike-slip fault that accommodates differential motion between the Africa and Arabia plates. Though both the Africa plate, to the west, and the Arabia plate, to the east, are moving in a NNE direction, the Arabia plate is moving slightly faster, resulting in the left-lateral, strike-slip motion along this segment of the plate boundary. Historically, earthquake activity along the Dead Sea Transform has been a significant hazard in the densely populated Levant region (eastern Mediterranean). For example, the November 1759 Near East earthquake is thought to have killed somewhere between 2,000-20,000 people. The northern termination of the Dead Sea Transform occurs within a complex tectonic region of southeast Turkey, where interaction of the Africa and Arabia plates and the Anatolia block occurs. This involves translational motion of the Anatolia Block westwards, with a speed of approximately 25mm/yr with respect to Eurasia, in order to accommodate closure of the Mediterranean basin.
The right-lateral, strike-slip North Anatolia Fault, in northern Turkey, accommodates much of the westwards motion between the Anatolia Block and Eurasia Plate. Between 1939 and 1999, a series of devastating M7.0+ strike-slip earthquakes propagated westwards along the North Anatolia Fault system. The westernmost of these earthquakes was the 17th August 1999, M7.6 Izmit earthquake, near the Sea of Marmara, killed approximately 17,000 people.
At the southern edge of the Anatolia Block lies the east-west trending Cyprian Arc with associated levels of moderate seismicity. The Cyprian Arc represents the convergent boundary between the Anatolia Block to the north and the Africa Plate to the south. The boundary is thought to join the East Anatolia Fault zone in eastern Turkey; however no certain geometry or sense of relative motion along the entire boundary is widely accepted.
Uganda: At least 35 people died as overcrowded boat capsizes on Lake Victoria
Sunday, November 25th, 2018WHO: Putting stalled malaria control efforts back on track
Sunday, November 25th, 2018Reductions in malaria cases have stalled after several years of decline globally, according to the new World malaria report 2018. To get the reduction in malaria deaths and disease back on track, WHO and partners are joining a new country-led response, launched today, to scale up prevention and treatment, and increased investment, to protect vulnerable people from the deadly disease.
For the second consecutive year, the annual report produced by WHO reveals a plateauing in numbers of people affected by malaria: in 2017, there were an estimated 219 million cases of malaria, compared to 217 million the year before. But in the years prior, the number of people contracting malaria globally had been steadily falling, from 239 million in 2010 to 214 million in 2015.
“Nobody should die from malaria. But the world faces a new reality: as progress stagnates, we are at risk of squandering years of toil, investment and success in reducing the number of people suffering from the disease,” says Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “We recognise we have to do something different – now. So today we are launching a country-focused and -led plan to take comprehensive action against malaria by making our work more effective where it counts most – at local level.”
Where malaria is hitting hardest
In 2017, approximately 70% of all malaria cases (151 million) and deaths (274 000) were concentrated in 11 countries: 10 in Africa (Burkina Faso, Cameroon, Democratic Republic of the Congo, Ghana, Mali, Mozambique, Niger, Nigeria, Uganda and United Republic of Tanzania) and India. There were 3.5 million more malaria cases reported in these 10 African countries in 2017 compared to the previous year, while India, however, showed progress in reducing its disease burden.
Despite marginal increases in recent years in the distribution and use of insecticide-treated bed nets in sub-Saharan Africa – the primary tool for preventing malaria – the report highlights major coverage gaps. In 2017, an estimated half of at-risk people in Africa did not sleep under a treated net. Also, fewer homes are being protected by indoor residual spraying than before, and access to preventive therapies that protect pregnant women and children from malaria remains too low.
High impact response needed
In line with WHO’s strategic vision to scale up activities to protect people’s health, the new country-driven “High burden to high impact” response plan has been launched to support nations with most malaria cases and deaths. The response follows a call made by Dr Tedros at the World Health Assembly in May 2018 for an aggressive new approach to jump-start progress against malaria. It is based on four pillars:
- Galvanizing national and global political attention to reduce malaria deaths;
- Driving impact through the strategic use of information;
- Establishing best global guidance, policies and strategies suitable for all malaria endemic countries; and
- Implementing a coordinated country response.
Catalyzed by WHO and the RBM Partnership to End Malaria, “High burden to high impact” builds on the principle that no one should die from a disease that can be easily prevented and diagnosed, and that is entirely curable with available treatments.
“There is no standing still with malaria. The latest World malaria report shows that further progress is not inevitable and that business as usual is no longer an option,” said Dr Kesete Admasu, CEO of the RBM Partnership. “The new country-led response will jumpstart aggressive new malaria control efforts in the highest burden countries and will be crucial to get back on track with fighting one of the most pressing health challenges we face.”
Targets set by the WHO Global technical strategy for malaria 2016–2030 to reduce malaria case incidence and death rates by at least 40% by 2020 are not on track to being met.
Pockets of progress
The report highlights some positive progress. The number of countries nearing elimination continues to grow (46 in 2017 compared to 37 in 2010). Meanwhile in China and El Salvador, where malaria had long been endemic, no local transmission of malaria was reported in 2017, proof that intensive, country-led control efforts can succeed in reducing the risk people face from the disease.
In 2018, WHO certified Paraguay as malaria free, the first country in the Americas to receive this status in 45 years. Three other countries – Algeria, Argentina and Uzbekistan – have requested official malaria-free certification from WHO.
India – a country that represents 4% of the global malaria burden – recorded a 24% reduction in cases in 2017 compared to 2016. Also in Rwanda, 436 000 fewer cases were recorded in 2017 compared to 2016. Ethiopia and Pakistan both reported marked decreases of more than
240 000 in the same period.
“When countries prioritize action on malaria, we see the results in lives saved and cases reduced,” says Dr Matshidiso Moeti, WHO Regional Director for Africa. “WHO and global malaria control partners will continue striving to help governments, especially those with the highest burden, scale up the response to malaria.”
Domestic financing is key
As reductions in malaria cases and deaths slow, funding for the global response has also shown a levelling off, with US$ 3.1 billion made available for control and elimination programmes in 2017 including US$ 900 million (28%) from governments of malaria endemic countries. The United States of America remains the largest single international donor, contributing US$ 1.2 billion (39%) in 2017.
To meet the 2030 targets of the global malaria strategy, malaria investments should reach at least US$6.6 billion annually by 2020 – more than double the amount available today.
Editors note
Download the WHO World malaria report 2018 app for an interactive experience with the report’s country data: App Store (iOS devices) | Google Play (Android devices).
WHO: 2018’s World Malaria Report at a Glance
Wednesday, November 21st, 2018This year’s World malaria report at a glance
The WHO’s 11th World malaria report summarizes global progress in the fight against malaria up to the end of 2017. The 2017 report showed that progress against malaria has stalled in many countries, and that the world was unlikely to achieve the WHO Global technical strategy for malaria 2016–2030 (GTS) morbidity and mortality targets for 2020. One year on, the 2018 report describes progress since then, including efforts to intensify the response in the highest burden countries.
Overview
Global and regional malaria burden, in numbers
Malaria cases
In 2017, an estimated 219 million cases of malaria occurred worldwide (95% confidence interval [CI]: 203–262 million), compared with 239 million cases in 2010 (95% CI: 219–285 million) and 217 million cases in 2016 (95% CI: 200–259 million).
Although there were an estimated 20 million fewer malaria cases in 2017 than in 2010, data for the period 2015–2017 highlight that no significant progress in reducing global malaria cases was made in this timeframe.
Most malaria cases in 2017 were in the WHO African Region (200 million or 92%), followed by the WHO South-East Asia Region with 5% of the cases and the WHO Eastern Mediterranean Region with 2%.
Fifteen countries in sub-Saharan Africa and India carried almost 80% of the global malaria burden. Five countries accounted for nearly half of all malaria cases worldwide: Nigeria (25%), Democratic Republic of the Congo (11%), Mozambique (5%), India (4%) and Uganda (4%).
The 10 highest burden countries in Africa reported increases in cases of malaria in 2017 compared with 2016. Of these, Nigeria, Madagascar and the Democratic Republic of the Congo had the highest estimated increases, all greater than half a million cases. In contrast, India reported 3 million fewer cases in the same period, a 24% decrease compared with 2016.
The incidence rate of malaria declined globally between 2010 and 2017, from 72 to 59 cases per 1000 population at risk. Although this represents an 18% reduction over the period, the number of cases per 1000 population at risk has stood at 59 for the past 3 years.
The WHO South-East Asia Region continued to see its incidence rate fall – from 17 cases of the disease per 1000 population at risk in 2010 to 7 in 2017 (a 59% decrease). All other WHO regions recorded either little progress or an increase in incidence rate. The WHO Region of the Americas recorded a rise, largely due to increases in malaria transmission in Brazil, Nicaragua and Venezuela (Bolivarian Republic of). In the WHO African Region, the malaria incidence rate remained at 219 cases per 1000 population at risk for the second year in a row.
Plasmodium falciparum is the most prevalent malaria parasite in the WHO African Region, accounting for 99.7% of estimated malaria cases in 2017, as well as in the WHO regions of South-East Asia (62.8%), the Eastern Mediterranean (69%) and the Western Pacific (71.9%). P. vivax is the predominant parasite in the WHO Region of the Americas, representing 74.1% of malaria cases.
Malaria deaths
In 2017, there were an estimated 435 000 deaths from malaria globally, compared with 451 000 estimated deaths in 2016, and 607 000 in 2010.
Children aged under 5 years are the most vulnerable group affected by malaria. In 2017, they accounted for 61% (266 000) of all malaria deaths worldwide.
The WHO African Region accounted for 93% of all malaria deaths in 2017. Although the WHO African Region was home to the highest number of malaria deaths in 2017, it also accounted for 88% of the 172 000 fewer global malaria deaths reported in 2017 compared with 2010.
Nearly 80% of global malaria deaths in 2017 were concentrated in 17 countries in the WHO African Region and India; 7 of these countries accounted for 53% of all global malaria deaths: Nigeria (19%), Democratic Republic of the Congo (11%), Burkina Faso (6%), United Republic of Tanzania (5%), Sierra Leone (4%), Niger (4%) and India (4%).
All WHO regions except the WHO Region of the Americas recorded reductions in mortality in 2017 compared with 2010. The largest declines occurred in the WHO regions of South- East Asia (54%), Africa (40%) and the Eastern Mediterranean (10%). Despite these gains, the malaria mortality reduction rate has also slowed since 2015, reflecting the estimated trends in malaria case incidence.
Malaria-related anaemia
This year’s report includes a section on malaria-related anaemia, a condition that, left untreated, can result in death, especially among vulnerable populations such as pregnant women and children aged under 5 years.
Anaemia was once a key indicator of progress in malaria control, and its prevalence was used to evaluate the efficacy of interventions. Recent years have seen a decline in awareness of the burden of malaria-associated anaemia
Despite its importance as a direct and indirect consequence of malaria, the prevalence of anaemia among populations vulnerable to the disease has not been reported consistently as a metric of malaria transmission and burden.
Data from household surveys conducted in 16 high-burden African countries between 2015 and 2017 show that, among children aged under 5 years, the prevalence of any anaemia was 61%, mild anaemia 25%, moderate anaemia 33% and severe anaemia 3%. Of children who tested positive for malaria, the prevalence of any anaemia was 79%, mild anaemia 21%, moderate anaemia 50% and severe anaemia 8%.
Investments in malaria programmes and research
Malaria control and elimination investments
In 2017, an estimated US$ 3.1 billion was invested in malaria control and elimination efforts globally by governments of malaria endemic countries and international partners – an amount slighter higher than the figure reported for 2016.
Nearly three quarters (US$ 2.2 billion) of investments in 2017 were spent in the WHO African Region, followed by the WHO regions of South-East Asia (US$ 300 million), the Americas (US$ 200 million), and the Eastern Mediterranean and the Western Pacific (US$ 100 million each).
In 2017, US$ 1.4 billion was invested in low-income countries, US$ 1.2 billion in lower-middle income countries and US$ 300 million in upper-middle-income countries. International funding represented the major source of funding in low-income and lower-middle-income countries, at 87% and 70%, respectively.
Governments of endemic countries contributed 28% of total funding (US$ 900 million) in 2017, a figure unchanged from 2016. Two thirds of domestically sourced funds were invested in malaria control activities carried out by national malaria programmes (NMPs), with the remaining share estimated as the cost of patient care.
As in previous years, the United States of America (USA) was the largest international source of malaria financing, providing US$ 1.2 billion (39%) in 2017. Country members of the Development Assistance Committee together accounted for US$ 700 million (21%). The United Kingdom of Great Britain and Northern Ireland contributed around US$ 300 million (9%) while the Bill & Melinda Gates Foundation provided US$ 100 million (2%).
Of the US$ 3.1 billion invested in 2017, US$ 1.3 billion was channelled through the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Investment outlook
Although funding for malaria has remained relatively stable since 2010, the level of investment in 2017 is far from what is required to reach the first 2 milestones of the GTS; that is, a reduction of at least 40% in malaria case incidence and mortality rates globally by 2020, compared with 2015 levels.
To reach the GTS 2030 targets, it is estimated that annual malaria funding will need to increase to at least US$ 6.6 billion per year by 2020.
Stepping up investments in malaria research and development is key to achieving the GTS targets. In 2016, US$ 588 million was spent in this area, representing 85% of the estimated annual need for research and development.
Although research and development funding for malaria vaccines and drugs declined in 2016 compared with 2015, investments in vector control products almost doubled, from US$ 33 million to US$ 61 million.
Deliveries of malaria commodities
Insecticide-treated mosquito nets
Between 2015 and 2017, a total of 624 million insecticide-treated mosquito nets (ITNs), mainly long-lasting insecticidal nets (LLINs), were reported by manufacturers as having been delivered globally. This represents a substantial increase over the previous period 2012–2014, when 465 million ITNs were delivered globally.
An estimated 552 million ITNs were distributed by NMPs globally, with most (459 million or 83%) being delivered in sub-Saharan Africa over the period 2015–2017.
Globally, 85% of ITNs were distributed through free mass distribution campaigns, 8% in antenatal care facilities and 4% as part of immunization programmes.
Rapid diagnostic tests
An estimated 276 million rapid diagnostic tests (RDTs) were sold globally in 2017.
In 2017, 245 million RDTs were distributed by NMPs. Most RDTs (66%) were tests that detected P. falciparum only and were supplied to sub-Saharan Africa.
In sub-Saharan Africa, RDTs are becoming increasingly the most used method to test for malaria diagnosis among suspected malaria patients in public health facilities. In 2017, an estimated 75% of malaria tests were conducted using RDTs, up from 40% in 2010.
Artemisinin-based combination therapy
An estimated 2.74 billion treatment courses of artemisinin-based combination therapy (ACT) were procured by countries over the period 2010–2017. An estimated 62% of these procurements were reported to have been made for the public sector.
During the period 2010–2017, 1.45 billion ACT treatment courses were delivered by NMPs, of which 1.42 billion (98%) were in the WHO African Region.
With increases in diagnostic testing in recent years, ACT treatment courses are becoming more targeted towards patients who tested positive for malaria. This is demonstrated by a substantially reduced ratio of ACTs to tests (0.8 in 2017 compared with 2.5 in 2010). Nevertheless, this implies that an estimated 30% of patients who received ACTs were not tested for malaria.
Preventing malaria
Vector control
Half of people at risk of malaria in Africa are sleeping under an ITN: in 2017, 50% of the population was protected by this intervention, an increase from 29% in 2010. Furthermore, the percentage of the population with access to an ITN increased from 33% in 2010 to 56% in 2017. However, coverage has improved only marginally since 2015 and has been at a standstill since 2016.
Households with at least 1 ITN for every 2 people doubled to 40% between 2010 and 2017. However, this figure represents only a modest increase over the past 3 years, and remains far from the target of universal coverage.
Fewer people at risk of malaria are being protected by indoor residual spraying (IRS), a prevention method that involves spraying the inside walls of dwellings with insecticides. Globally, IRS protection declined from a peak of 5% in 2010 to 3% in 2017, with decreases seen across all WHO regions.
In the WHO African Region, IRS coverage dropped from 80 million people at risk in 2010, to a low point of 51 million in 2016 before rising to 64 million in 2017. In other WHO regions, the number of people protected with IRS in 2017 was 1.5 million in the Americas, 7.5 million in the Eastern Mediterranean, 41 million in South-East Asia, and 1.5 million in the Western Pacific.
The declines in IRS coverage are occurring as countries change or rotate insecticides (changing to more expensive chemicals), and as operational strategies change (e.g. decreasing at-risk populations in malaria elimination countries).
Preventive therapies
To protect women in areas of moderate and high malaria transmission in Africa, WHO recommends “intermittent preventive treatment in pregnancy” (IPTp) with the antimalarial drug sulfadoxine-pyrimethamine. Among 33 African countries that reported on IPTp coverage levels in 2017, an estimated 22% of eligible pregnant women received the recommended 3 or more doses of IPTp, compared with 17% in 2015 and 0% in 2010.
In 2017, 15.7 million children in 12 countries in Africa’s Sahel subregion were protected through seasonal malaria chemoprevention (SMC) programmes. However, about 13.6 million children who could have benefited from this intervention were not covered, mainly due to a lack of funding.
Diagnostic testing and treatment
Accessing care
Prompt diagnosis and treatment is the most effective way to prevent a mild case of malaria from developing into severe disease and death. Based on national household surveys completed in 19 countries in sub-Saharan Africa between 2015 and 2017, a median of 52% (interquartile range [IQR]: 44–62%) of children with a fever (febrile) were taken to a trained medical provider for care. This includes public sector hospitals and clinics, formal private sector health facilities and community health workers.
Although more febrile children were brought for care in the public health sector (median: 36%, IQR: 30–46%) than in the formal medical private sector (median: 8%, IQR: 5–10%), a high proportion of febrile children did not receive any medical attention (median: 40%, IQR: 28–45%). Poor access to health care providers or lack of awareness of malaria symptoms among caregivers are among the contributing factors.
The national surveys reveal disparities in access to health care based on household income and location: the percentage of febrile children brought for care was higher in wealthier households (median: 72%, IQR: 62–75%) compared with poorer households (median: 58%, IQR: 47–67%), and was higher among those living in urban areas (median: 69%, IQR: 59–76%) compared with rural areas (median: 60%, IQR: 51–71%).
Diagnosing malaria
According to 58 surveys conducted in 30 sub-Saharan African countries between 2010 and 2017, the percentage of children with a fever that received a diagnostic test in the public health sector has increased, hitting a median of 59% (IQR: 34–75%) over the period 2015– 2017, up from a median of 33% (IQR:18–44%) for 2010–2012.
Data collected from 56 surveys carried out in sub-Saharan Africa reveal that the percentage of febrile children attending public health facilities who received a malaria diagnostic test before antimalarial treatment has gone up from a median of 35% (IQR: 27–56%) in 2010–2012 to 74% (IQR: 51–81%) in 2015–2017. A similar increase has been recorded in the formal private health sector, from 41% (IQR: 17–67%) in 2010–2012 to 63% (IQR: 41–83%) in 2015–2017.
Treating malaria
Based on 19 household surveys conducted in sub-Saharan Africa between 2015 and 2017, the percentage of children aged under 5 years with a fever who received any antimalarial drug was 29% (IQR: 15–48%).
Children are more likely to be given ACTs – the most effective antimalarial drugs – if medical care is sought in the public sector compared with the private sector. Data from 18 national surveys conducted in sub-Saharan Africa show that for the period 2015–2017, an estimated 88% (IQR: 73–92%) of febrile children brought for treatment for malaria in the public health sector received ACTs, compared with 74% (IQR: 47–88%) in the formal medical private sector.
To bridge the treatment gap among children, WHO recommends the uptake of integrated community case management (iCCM). This approach promotes integrated management of common life-threatening conditions in children – malaria, pneumonia and diarrhoea – at health facility and community levels. In 2017, of 21 African countries with high malaria burden, 20 had iCCM policies in place, of which 12 had started implementing those policies.
Malaria surveillance systems
Effective surveillance of malaria cases and deaths is essential for identifying the areas or population groups that are most affected by malaria, and for targeting resources for maximum impact. A strong surveillance system requires high levels of access to care and case detection, and complete reporting of health information by all sectors, whether public or private.
In 2017, among 52 moderate to high-burden countries, reporting rates of malaria were 60% or more. In the WHO African Region, 36 out of 46 countries indicated that at least 80% of public health facilities had reported data on malaria through their national health information system.
Malaria elimination
Globally, the elimination net is widening, with more countries moving towards zero indigenous cases: in 2017, 46 countries reported fewer than 10 000 such cases, up from 44 countries in 2016 and 37 countries in 2010. The number of countries with less than 100 indigenous cases – a strong indicator that elimination is within reach – increased from 15 countries in 2010 to 24 countries in 2016 and 26 countries in 2017.
Paraguay was certified by WHO as malaria free in 2018, while Algeria, Argentina and Uzbekistan have made formal requests to WHO for certification. In 2017, China and El Salvador reported zero indigenous cases.
One of the key GTS milestones for 2020 is elimination of malaria in at least 10 countries that were malaria endemic in 2015. At the current rate of progress, it is likely that this milestone will be reached.
In 2016, WHO identified 21 countries with the potential to eliminate malaria by the year 2020. WHO is working with the governments in these countries – known as “E-2020 countries” – to support their elimination acceleration goals.
Although 11 E-2020 countries remain on track to achieve their elimination goals, 10 have reported increases in indigenous malaria cases in 2017 compared with 2016.
Challenges in getting the malaria response back on track
The challenges facing the global malaria response are many, and as highlighted in this year’s report, immediate barriers to achieving the fast-approaching GTS milestones for 2020 and 2025 are malaria’s continued rise in countries with the highest burden of the disease and inadequate international and domestic funding. At the same time, the continued emergence of parasite resistance to antimalarial medicines and mosquito resistance to insecticides pose threats to progress.
High-burden countries
In 2017, 11 countries accounted for approximately 70% of estimated malaria cases and deaths globally: 10 in sub-Saharan Africa and India. Among these countries, only India reported progress in reducing its malaria cases in 2017 compared to 2016.
To get the global malaria response back on track, a new country-driven approach – “High burden to high impact” – will be launched in Mozambique on 19 November 2018, alongside the release of the World malaria report 2018.
Catalyzed by WHO and the RBM Partnership to End Malaria, the approach is founded upon 4 pillars: galvanize national and global political attention to reduce malaria deaths; drive impact in country through the strategic use of information; establish best global guidance, policies and strategies suitable for all malaria endemic countries; and implement a coordinated country response.
Funding
In 24 out of 41 high-burden countries, which rely mainly on external funding for malaria programmes, the average level of funding available per person at risk declined in 2015–2017 compared to 2012–2014. This ranged from a 95% reduction in the Congo (highest) to a 1% decrease in Uganda (lowest) over the time points compared.
In the countries that experienced a 20% or more decrease in total funding per person at risk, international financing declined, at times combined with lower domestic investments.
Among the 41 high-burden countries, overall, funding per person at risk of malaria stood at US$ 2.32.
Drug resistance
ACTs have been integral to the recent success of global malaria control, and protecting their efficacy for the treatment of malaria is a global health priority.
Most studies conducted between 2010 and 2017 show that ACTs remain effective, with overall efficacy rates greater than 95% outside the Greater Mekong subregion (GMS). In Africa, artemisinin (partial) resistance has not been reported to date.
Although multidrug resistance, including artemisinin (partial) resistance and partner drug resistance, has been reported in 4 GMS countries, there has been a massive reduction in malaria cases and deaths in this subregion. Monitoring the efficacy of antimalarial drugs has resulted in prompt updating of malaria treatment policies in most GMS countries.
Insecticide resistance
The recently released WHO Global report on insecticide resistance in malaria vectors: 2010– 2016 showed that resistance to the four commonly used insecticide classes – pyrethroids, organochlorines, carbamates and organophosphates – is widespread in all major malaria vectors across the WHO regions of Africa, the Americas, South-East Asia, the Eastern Mediterranean and the Western Pacific.
Of the 80 malaria endemic countries that provided data for 2010–2017, resistance to at least 1 of the 4 insecticide classes in 1 malaria vector from 1 collection site was detected in 68 countries, an increase over 2016 due to improved reporting and 3 new countries reporting on resistance for the first time. In 57 countries, resistance to 2 or more insecticide classes was reported.
Resistance to pyrethroids – the only insecticide class currently used in ITNs – is widespread and was detected in at least 1 malaria vector in more than two thirds of the sites tested and was highest in the WHO regions of Africa and the Eastern Mediterranean.
Resistance to organochlorines was detected for at least 1 malaria vector in almost two thirds of the sites and was highest in the WHO South-East Asia Region. Resistance to carbamates and organophosphates was less prevalent and was detected in 33% and 27% of the tested sites, respectively. Prevalence was highest for carbamates in the WHO South-East Asia Region and for organophosphates in the WHO Western Pacific Region.
In view of the current situation, resistance monitoring and management plans are essential, in line with the WHO Global plan for insecticide resistance management in malaria vectors. To date, 40 countries have completed these plans.
ITNs continue to be an effective tool for malaria prevention, even in areas where mosquitoes have developed resistance to pyrethroids. This was evidenced in a large multicountry evaluation coordinated by WHO between 2011 and 2016 across study locations in 5 countries.