https://www.moh.gov.sg/news-highlights/details/eight-more-confirmed-cases-of-covid-19-infection
As of 13 February 2020, 12pm, the Ministry of Health (MOH) has confirmed and verified eight additional cases of COVID-19 infection in Singapore, all of which are linked to previous cases.
Links between previous cases found
1. Further epidemiological investigations and contact tracing have uncovered links between previously announced and new cases. This was made possible with the assistance of the Singapore Police Force.
a. Cases 8 and 9, as well as Cases 31, 33 and 38, are linked to The Life Church and Missions Singapore (146B Paya Lebar Road). This is a possible cluster involving five cases (Cases 8, 9, 31, 33 and 38).
b. Nine of the confirmed cases (Cases 19, 20, 21, 24, 25, 27, 28, 34 and 40) are linked to the cluster associated with Yong Thai Hang (24 Cavan Road).
c. Three of the confirmed cases (Cases 30, 36 and 39) are linked to the private business meeting held at Grand Hyatt Singapore from 20 to 22 January.
d. Four of the confirmed cases (Cases 42, 47, 52 and 56) are linked to the Seletar Aerospace Heights construction site.
e. Seven of the confirmed cases (Cases 48, 49, 51, 53, 54, 57 and 58) are linked to the Grace Assembly of God.
Investigations on these clusters are ongoing.
3. Contact tracing is underway for the other seven locally transmitted cases to establish any links to previous cases or travel history to mainland China. Case 44 was a contact of Cases 13 and 26. Case 55 is linked to Case 50.
About the confirmed cases
Case 51
4. Case 51 is a 48 year-old male Singapore Citizen with no recent travel history to China. He is currently warded in an isolation room at the National Centre for Infectious Diseases (NCID). He is linked to the cluster at Grace Assembly of God.
5. He reported onset of symptoms on 4 February and sought treatment at a general practitioner (GP) clinic on 5 February and 10 February. He went to NCID on 11 February, and subsequent test results confirmed COVID-19 infection on 12 February afternoon.
6. Prior to hospital admission, he went to work at Grace Assembly of God (Tanglin) (355 Tanglin Road) and Grace Assembly of God (Bukit Batok) (1 Bukit Batok West Avenue 4). He stays at Bishan Street 13.
Case 52
7. Case 52 is a 37 year-old male Bangladesh national who is a Singapore Work Pass holder, and has no recent travel history to China. He is currently warded in an isolation room at NCID. He is linked to the cluster at Seletar Aerospace Heights construction site.
8. He reported onset of symptoms on 7 February. As he was identified as a close contact of Cases 42 and 47, he was transported by an ambulance to Tan Tock Seng Hospital on 11 February. Subsequent test results confirmed COVID-19 infection on 12 February afternoon.
9. Prior to hospital admission, he had gone to work at the Seletar Aerospace Heights construction site, the same location where Cases 42 and 47 had worked. He reported that he had mostly stayed at his rental apartment at Campbell Lane since the onset of symptoms.
Case 53
10. Case 53 is a 54 year-old male Singapore Citizen with no recent travel history to China. He is currently warded in an isolation room at NCID. He is linked to the cluster at Grace Assembly of God.
11. He reported onset of symptoms on 10 February, and went to NCID on 12 February where he was immediately isolated. Subsequent test results confirmed COVID-19 infection on 12 February afternoon.
12. Prior to hospital admission, he reported that he had mostly stayed at home at Hillview Avenue. He works at the National University of Singapore, but had not interacted with colleagues and students after onset of symptoms.
Cases 54 to 58
13. Cases 54 (54 year-old female Singapore Citizen), 57 (26 year-old male Singapore Citizen) and 58 (55 year-old male Singapore Citizen) are linked to the cluster at Grace Assembly of God. All three cases did not have recent travel history to China. They were confirmed to have COVID-19 infection on 13 February morning, and are currently warded in separate isolation rooms at NCID.
14. Case 55 is a 30 year-old male Singapore Citizen with no recent travel history to China. He was confirmed to have COVID-19 infection on 13 February morning, and is currently warded in an isolation room at NCID. He is a family member of Case 50.
15. Case 56 is a 30 year-old male Bangladesh national with no recent travel history to China. He was confirmed to have COVID-19 infection on 13 February morning, and is currently warded in an isolation room at NCID. He is linked to the cluster at the Seletar Aerospace Heights construction site.
16. MOH has initiated epidemiological investigations and contact tracing to identify individuals who had close contact with the cases.
Case 50 (Announced on 12 February)
17. Case 50 is a 62 year-old male Singapore Citizen with no recent travel history to China. He is currently warded in an isolation room at NCID.
18. He reported onset of symptoms on 7 February and had sought treatment at two GP clinics on 7 February, 10 February and 11 February. He was admitted to NCID on 11 February and was immediately isolated. Subsequent test results confirmed COVID-19 infection on 12 February morning.
19. Prior to hospital admission, other than going to work at DBS Asia Central at Marina Bay Financial Centre (12 Marina Boulevard), he had stayed at his home at Mei Hwan Drive, except to seek medical treatment.
Update on condition of confirmed cases
20. To date, a total of 15 cases have fully recovered from the infection and have been discharged from hospital. Of the 43 confirmed cases who are still in hospital, most are stable or improving. Seven are in critical condition in the intensive care unit.
Update on suspect cases
21. As of 13 February 2020, 12pm, 711 of the suspect cases have tested negative for COVID-19, and 58 have tested positive. Test results for the remaining 82 cases are pending.
Update on contact tracing for confirmed cases
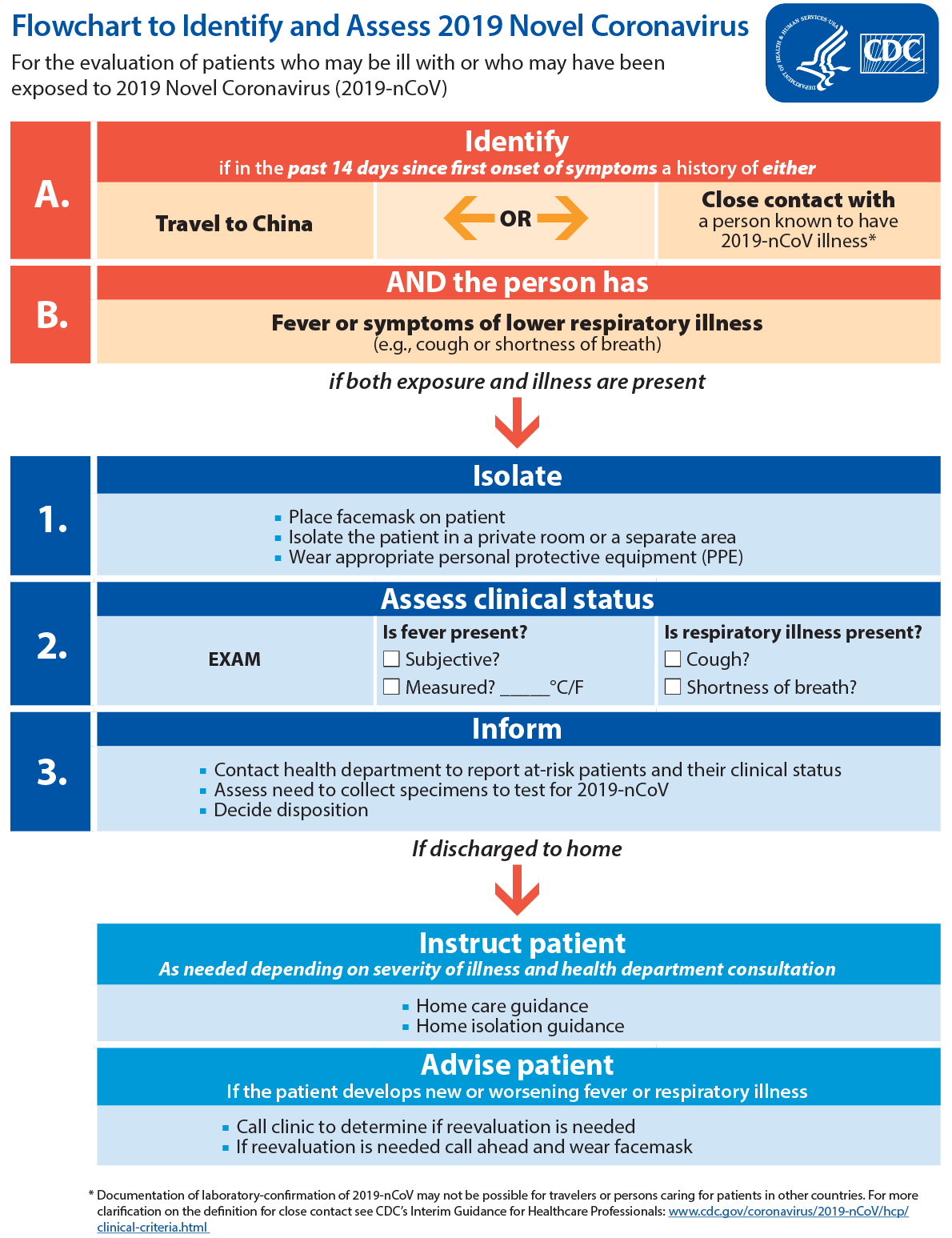
22. Contact tracing for the confirmed cases is ongoing. Once identified, MOH will closely monitor all close contacts. As a precautionary measure, they will be quarantined for 14 days from their last exposure to the patient. In addition, all other identified contacts who have a low risk of being infected will be under active surveillance, and will be contacted daily to monitor their health status.
23. As of 13 February 2020, 12pm, MOH has identified 1,278 close contacts. Of the 1,161 who are still in Singapore, 1,144 have been contacted and are being quarantined or isolated. Efforts are ongoing to contact the remaining 17 close contacts.
Health advisory
24. Singaporeans are advised to defer all travel to Hubei Province and all non-essential travel to Mainland China.
25. All travellers should monitor their health closely for two weeks upon return to Singapore and seek medical attention promptly if they feel unwell. Travellers should inform their doctor of their travel history. If they have a fever or respiratory symptoms (e.g. cough, shortness of breath), they should wear a mask and call the clinic ahead of the visit.
26. Travellers and members of the public should adopt the following precautions at all times:
- Avoid close contact with people who are unwell or showing symptoms of illness;
- Observe good personal hygiene;
- Practise frequent hand washing with soap (e.g. before handling food or eating, after going to toilet, or when hands are dirtied by respiratory secretions after coughing or sneezing);
- Wear a mask if you have respiratory symptoms such as a cough or shortness of breath;
- Cover your mouth with a tissue paper when coughing or sneezing, and dispose the soiled tissue paper in the rubbish bin immediately; and
- Seek medical attention promptly if you are feeling unwell.
- MOH will continue to monitor the situation closely. As medical practitioners are on the lookout for suspect cases, Singapore is likely to see more cases that will need to be investigated.
MINISTRY OF HEALTH
13 FEBRUARY 2020