Archive for the ‘Zika virus’ Category
The mosquito, Aedes albopictus, that is responsible for transmitting Zika virus and yellow fever is closing in on Portugal
Friday, October 5th, 2018WHO: Prioritizing Emerging Infectious Diseases in Need of Research and Development
Sunday, August 19th, 2018The World Health Organization R&D Blueprint aims to accelerate the availability of medical technologies during epidemics by focusing on a list of prioritized emerging diseases for which medical countermeasures are insufficient or nonexistent. The prioritization process has 3 components: a Delphi process to narrow down a list of potential priority diseases, a multicriteria decision analysis to rank the short list of diseases, and a final Delphi round to arrive at a final list of 10 diseases.
A group of international experts applied this process in January 2017, resulting in a list of 10 priority diseases. The robustness of the list was tested by performing a sensitivity analysis. The new process corrected major shortcomings in the pre–R&D Blueprint approach to disease prioritization and increased confidence in the results.
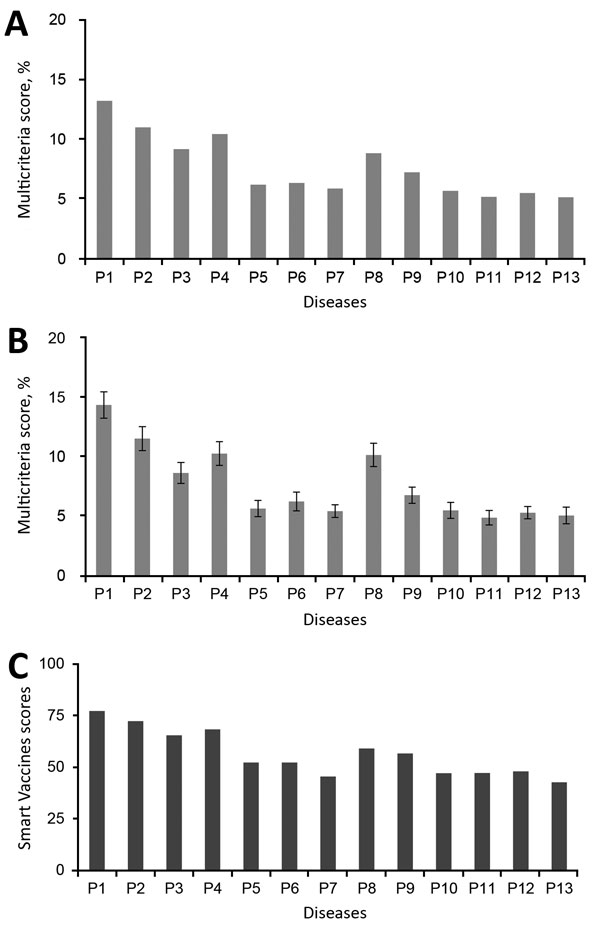
Multicriteria scores of diseases considered in the 2017 prioritization exercise for the development of the World Health Organization R&D Blueprint to prioritize emerging infectious diseases in need of research and development. A) Disease final ranking using the geometric average of the comparison matrices. B) Disease final ranking using the arithmetic average of the raw data. Error bars correspond to SD, indicating disagreement among experts. C) Disease final ranking using the SMART Vaccines prioritization tool (56). P1, Ebola virus infection; P2, Marburg virus infection; P3, Middle East Respiratory Syndrome coronavirus infection; P4, severe acute respiratory syndrome; P5, Lassa virus infection; P6, Nipah virus infection; P7, Rift Valley fever; P8, Zika virus infection; P9, Crimean-Congo hemorrhagic fever; P10, severe fever with thrombocytopenia syndrome; P11, South American hemorrhagic fever; P12, plague; P13, hantavirus infection.
Si Mehand M, Millett P, Al-Shorbaji F, Roth C, Kieny MP, Murgue B. World Health Organization methodology to prioritize emerging infectious diseases in need of research and development. Emerg Infect Dis. 2018 Sep [date cited]. https://doi.org/10.3201/eid2409.171427
Sterile Insect Technique on Aedes aegypti mosquitoes
Monday, July 16th, 2018In an international partnership between CSIRO, Verily and James Cook University, scientists used specialised technology to release millions of sterilised male Aedes aegypti mosquitoes across the Cassowary Coast in Queensland in a bid to combat the global pest.
CSIRO Director of Health and Biosecurity Dr Rob Grenfell said the results were a major win in the fight against diseases-spreading mosquitoes.
“The invasive Aedes aegypti mosquito is one of the world’s most dangerous pests, capable of spreading devastating diseases like dengue, Zika and chikungunya and responsible for infecting millions of people with disease around the world each year,” Dr Grenfell said.
“Increased urbanisation and warming temperatures mean that more people are at risk, as these mosquitoes which were once relegated to areas near the equator forge past previous climatic boundaries.
“Although the majority of mosquitoes don’t spread diseases, the three mostly deadly types the Aedes, Anopheles and Culex are found almost all over the world and are responsible for around 17 per cent of infectious disease transmissions globally.”
From November 2017 to June this year, non-biting male Aedes aegypti mosquitoes sterilised with the natural bacteria Wolbachia were released in trial zones along the Cassowary Coast in North Queensland.
They mated with local female mosquitoes, resulting in eggs that did not hatch and a significant reduction of their population.
“Our heartfelt thanks goes out to the Innisfail community who literally opened their doors to our team, letting us install mosquito traps around their homes and businesses – we couldn’t have done this without your support,” Dr Grenfell said.
The process, known as the Sterile Insect Technique, has been successfully used since the 1950s but the challenge in making it work for mosquitoes like the Aedes aegypti has been rearing enough mosquitoes, removing biting females, identifying the males and then releasing the huge numbers needed to suppress a population.
To address this challenge, Verily, an affiliate of Alphabet Inc, developed a mosquito rearing and sex sorting and release technology as part of its global Debug project.
“We’re very pleased to see strong suppression of these dangerous biting female Aedes aegypti mosquitoes,” Verily’s Nigel Snoad said.
“We are particularly thankful to the people of Innisfail for their strong support, which has been incredible.
“We came to Innisfail with CSIRO and JCU to see how this approach worked in a tropical environment where these mosquitoes thrive, and to learn what it was like to operate our technology with research collaborators as we work together to find new ways to tackle these dangerous mosquitoes.”
Scientists compared the number of Aedes aegypti mosquitoes trapped in release sites and control zones to monitor and track populations.
The millions of mosquitoes needed for the trial were reared at James Cook University in Cairns.
To produce the three million male mosquitoes needed for the trial, researchers at James Cook University (JCU) in Cairns set out to raise almost 20 million Aedes aegypti.
“We allowed for the possibility of deaths during the process, as well as the need to sift out the female half of the population,” Dr Kyran Staunton from James Cook University said.
“Verily’s technology enabled us to do the sex sorting faster and with much higher accuracy.
“We learnt a lot from collaborating on this first tropical trial and we’re excited to see how this approach might be applied in other regions where Aedes aegypti poses a threat to life and health.”
“The health of our nation is paramount as we help Australia achieve its vision to become one of the healthiest nations on earth,” CSIRO Chief Executive Dr Larry Marshall said.
“By enabling industry partners like Verily to leverage the world-leading health capability we have built in CSIRO we can deliver this moonshot and tackle some of the world’s most wicked challenges with science.”
Clinical differences between Dengue and Zika
Thursday, June 28th, 2018Yan G, Pang L, Cook AR, Ho HJ, Win MS, Khoo AL, et al. Distinguishing Zika and dengue viruses through simple clinical assessment, Singapore. Emerg Infect Dis. 2018 Aug [date cited]. https://doi.org/10.3201/eid2408.171883
“…Conjunctivitis strongly indicated Zika virus infection (odds ratio [OR] 30.1, 95% CI 9.57–94.44; p < 0.001). In contrast, fever (OR 0.05, 95% CI 0.01–0.47; p = 0.008), myalgia (OR 0.20, 95% CI 0.08–0.48; p<0.001), and headache (OR 0.12, 95% CI 0.05–0.30; p<0.001) were more prominent in patients with DENV infection.
Further, DENV patients tended to have thrombocytopenia (median platelet count 132 × 109/µL, range 15–386 × 109/µL) and monocytosis (median monocyte count 0.50 × 109/µL, range 0.11–1.70 × 109/µL), whereas Zika patients tended to have normal platelet (median 225 × 109/µL, range 128–326 × 109/µL; p<0.001) and monocyte (median 0.35 × 109/µL, range 0.13–1.00 × 109/µL; p = 0.021) counts……”
WHO: List of Blueprint priority diseases (i.e. diseases and pathogens to prioritize for research and development in public health emergency contexts)
Tuesday, May 22nd, 20182018 annual review of the Blueprint list of priority diseases
For the purposes of the R&D Blueprint, WHO has developed a special tool for determining which diseases and pathogens to prioritize for research and development in public health emergency contexts. This tool seeks to identify those diseases that pose a public health risk because of their epidemic potential and for which there are no, or insufficient, countermeasures. The diseases identified through this process are the focus of the work of R& D Blueprint. This is not an exhaustive list, nor does it indicate the most likely causes of the next epidemic.
The first list of prioritized diseases was released in December 2015.
Using a published prioritization methodology, the list was first reviewed in January 2017.
February 2018 – Second annual review
The second annual review occurred 6-7 February, 2018. Experts consider that given their potential to cause a public health emergency and the absence of efficacious drugs and/or vaccines, there is an urgent need for accelerated research and development for*:
- Crimean-Congo haemorrhagic fever (CCHF)
- Ebola virus disease and Marburg virus disease
- Lassa fever
- Middle East respiratory syndrome coronavirus (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS)
- Nipah and henipaviral diseases
- Rift Valley fever (RVF)
- Zika
- Disease X
Disease X represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease, and so the R&D Blueprint explicitly seeks to enable cross-cutting R&D preparedness that is also relevant for an unknown “Disease X” as far as possible.
A number of additional diseases were discussed and considered for inclusion in the priority list, including: Arenaviral hemorrhagic fevers other than Lassa Fever; Chikungunya; highly pathogenic coronaviral diseases other than MERS and SARS; emergent non-polio enteroviruses (including EV71, D68); and Severe Fever with Thrombocytopenia Syndrome (SFTS).
These diseases pose major public health risks and further research and development is needed, including surveillance and diagnostics. They should be watched carefully and considered again at the next annual review. Efforts in the interim to understand and mitigate them are encouraged.
Although not included on the list of diseases to be considered at the meeting, monkeypox and leptospirosis were discussed and experts stressed the risks they pose to public health. There was agreement on the need for: rapid evaluation of available potential countermeasures; the establishment of more comprehensive surveillance and diagnostics; and accelerated research and development and public health action.
Several diseases were determined to be outside of the current scope of the Blueprint: dengue, yellow fever, HIV/AIDs, tuberculosis, malaria, influenza causing severe human disease, smallpox, cholera, leishmaniasis, West Nile Virus and plague. These diseases continue to pose major public health problems and further research and development is needed through existing major disease control initiatives, extensive R&D pipelines, existing funding streams, or established regulatory pathways for improved interventions. In particular, experts recognized the need for improved diagnostics and vaccines for pneumonic plague and additional support for more effective therapeutics against leishmaniasis.
The experts also noted that:
- For many of the diseases discussed, as well as many other diseases with the potential to cause a public health emergency, there is a need for better diagnostics.
- Existing drugs and vaccines need further improvement for several of the diseases considered but not included in the priority list.
- Any type of pathogen could be prioritised under the Blueprint, not only viruses.
- Necessary research includes basic/fundamental and characterization research as well as epidemiological, entomological or multidisciplinary studies, or further elucidation of transmission routes, as well as social science research.
- There is a need to assess the value, where possible, of developing countermeasures for multiple diseases or for families of pathogens.
The impact of environmental issues on diseases with the potential to cause public health emergencies was discussed. This may need to be considered as part of future reviews.
The importance of the diseases discussed was considered for special populations, such as refugees, internally displaced populations, and victims of disasters.
The value of a One Health approach was stressed, including a parallel prioritization processes for animal health. Such an effort would support research and development to prevent and control animal diseases minimising spill-over and enhancing food security. The possible utility of animal vaccines for preventing public health emergencies was also noted.
Also there are concerted efforts to address anti-microbial resistance through specific international initiatives. The possibility was not excluded that, in the future, a resistant pathogen might emerge and appropriately be prioritized.
*The order of diseases on this list does not denote any ranking of priority.
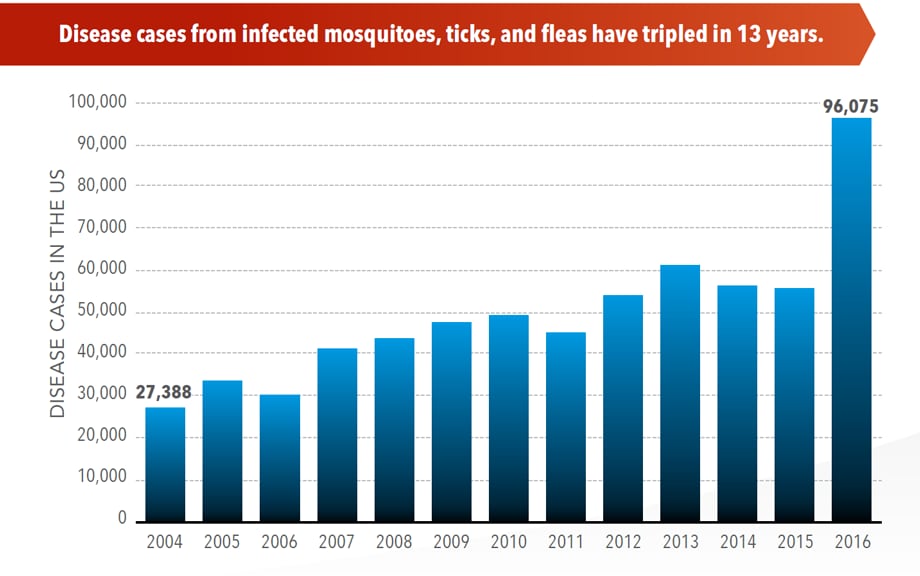
U.S. trends in occurrence of nationally reportable vectorborne diseases during 2004–2016.
Wednesday, May 2nd, 2018Rosenberg R, Lindsey NP, Fischer M, et al. Vital Signs: Trends in Reported Vectorborne Disease Cases — United States and Territories, 2004–2016. MMWR Morb Mortal Wkly Rep. ePub: 1 May 2018. DOI: http://dx.doi.org/10.15585/mmwr.mm6717e1.
Key Points
•A total of 642,602 cases of 16 diseases caused by bacteria, viruses, or parasites transmitted through the bites of mosquitoes, ticks, or fleas were reported to CDC during 2004–2016. Indications are that cases were substantially underreported.
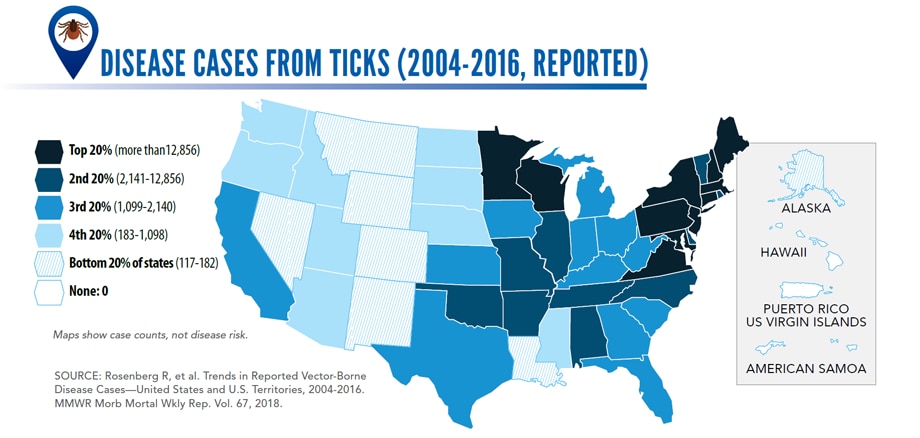
•Tickborne diseases more than doubled in 13 years and were 77% of all vectorborne disease reports. Lyme disease accounted for 82% of all tickborne cases, but spotted fever rickettsioses, babesiosis, and anaplasmosis/ehrlichiosis cases also increased.
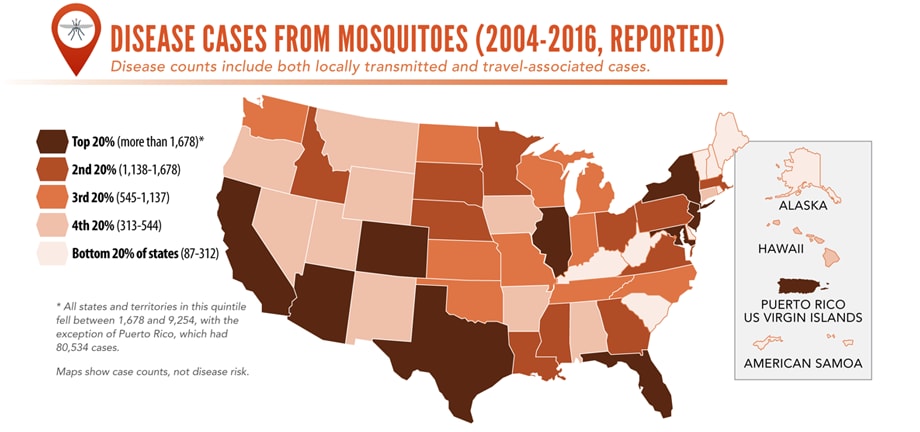
•Tickborne disease cases predominated in the eastern continental United States and areas along the Pacific coast. Mosquitoborne dengue, chikungunya, and Zika viruses were almost exclusively transmitted in Puerto Rico, American Samoa, and the U.S. Virgin Islands, where they were periodically epidemic. West Nile virus, also occasionally epidemic, was widely distributed in the continental United States, where it is the major mosquitoborne disease.
•During 2004–2016, nine vectorborne human diseases were reported for the first time from the United States and U.S. territories. The discovery or introduction of novel vectorborne agents will be a continuing threat.
•Vectorborne diseases have been difficult to prevent and control. A Food and Drug Administration–-approved vaccine is available only for yellow fever virus. Many of the vectorborne diseases, including Lyme disease and West Nile virus, have animal reservoirs. Insecticide resistance is widespread and increasing.
•Preventing and responding to vectorborne disease outbreaks are high priorities for CDC and will require additional capacity at state and local levels for tracking, diagnosing, and reporting cases; controlling vectors; and preventing transmission.
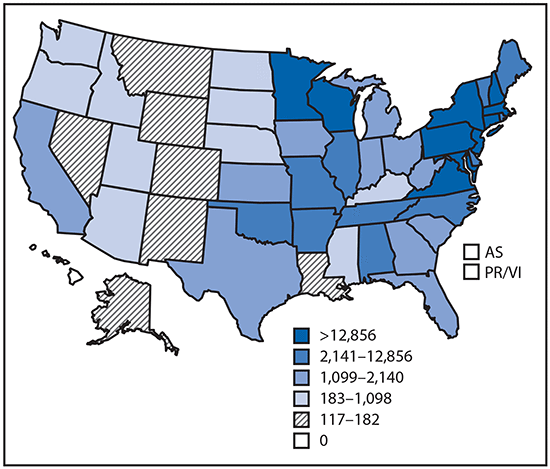
Reported cases* of tickborne disease — U.S. states and territories, 2004–2016
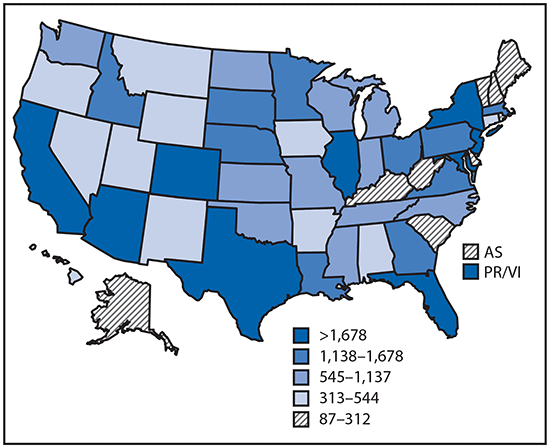
Reported cases* of mosquitoborne disease — U.S. states and territories, 2004–2016
Reported nationally notifiable mosquitoborne,* tickborne, and fleaborne† disease cases — U.S. states and territories, 2004–2016
The number of reported cases of disease from mosquito, tick, and flea bites has more than tripled in the USA (2004-2016)
Wednesday, May 2nd, 2018More cases in the US (2004-2016)
- The number of reported cases of disease from mosquito, tick, and flea bites has more than tripled.
- More than 640,000 cases of these diseases were reported from 2004 to 2016.
- Disease cases from ticks have doubled.
- Mosquito-borne disease epidemics happen more frequently.
More germs (2004-2016)
- Chikungunya and Zika viruses caused outbreaks in the US for the first time.
- Seven new tickborne germs can infect people in the US.
More people at risk
- Commerce moves mosquitoes, ticks, and fleas around the world.
- Infected travelers can introduce and spread germs across the world.
- Mosquitoes and ticks move germs into new areas of the US, causing more people to be at risk.
The US is not fully prepared
- Local and state health departments and vector control organizations face increasing demands to respond to these threats.
- More than 80% of vector control organizations report needing improvement in 1 or more of 5 core competencies, such as testing for pesticide resistance.
- More proven and publicly accepted mosquito and tick control methods are needed to prevent and control these diseases.
Vector-Borne Diseases Reported by States to CDC

Mosquito-borne diseases
- California serogroup viruses
- Chikungunya virus
- Dengue viruses
- Eastern equine encephalitis virus
- Malaria plasmodium
- St. Louis encephalitis virus
- West Nile virus
- Yellow fever virus
- Zika virus

Tickborne diseases
- Anaplasmosis/ehrlichiosis
- Babesiosis
- Lyme disease
- Powassan virus
- Spotted fever rickettsiosis
- Tularemia

Fleaborne disease
- Plague
For more information: https://wwwn.cdc.gov/nndss/
The 2016 Earthquake in Ecuador and the Zika Outbreak
Friday, April 27th, 2018| The 2016 Earthquake in Ecuador: Zika Outbreak After a Natural Disaster | ||
| Diana Pacheco Barzallo, Andrea Pacheco Barzallo, and Eulalia Narvaez | ||
|
Health Security, Vol. 16, No. 2, April 2018: 127-134.] “……Our results suggest that the earthquake increased the reported cases of Zika by 0.509 per epidemiologic week (data per 10,000 population), and we argue that the destroyed built environment along with other factors created a disease focus, where the virus spread easily. Because of its potential complications and devastating long-term effects, Zika represents a national threat……”
|
||
Disease X: A pathogen with the potential to spread and kill millions but for which there are currently no, or insufficient, countermeasures available.
Sunday, March 11th, 2018“……It was the third time the committee, consisting of leading virologists, bacteriologists and infectious disease experts, had met to consider diseases with epidemic or pandemic potential. But when the 2018 list was released two weeks ago it included an entry not seen in previous years.
- Crimean-Congo haemorrhagic fever (CCHF)
- Ebola virus disease and Marburg virus disease
- Lassa fever
- Middle East respiratory syndrome coronavirus (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS)
- Nipah and henipaviral diseases
- Rift Valley fever (RVF)
- Zika
- Disease X
*Diseases posing significant risk of an international public health emergency for which there is no, or insufficient, countermeasures. Source: World Health Organization (WHO), 2018


