George Washington Bridge Live Stream
February 27th, 2022CDC Video: Preparing and Administrating Heptavalent Antitoxin for the Treatment of Botulism
May 21st, 2021
Rao AK, Sobel J, Chatham-Stephens K, Luquez C. Clinical Guidelines for Diagnosis and Treatment of Botulism, 2021. MMWR Recomm Rep 2021;70(No. RR-2):1–30. DOI: http://dx.doi.org/10.15585/mmwr.rr7002a1external icon
https://www.cdc.gov/mmwr/volumes/70/rr/rr7002a1.htm?ACSTrackingID=USCDC_1052-DM57269&ACSTrackingLabel=CDC%20Publishes%20First%20Comprehensive%20Clinical%20Guidelines%20for%20Diagnosis%20and%20Treatment%20of%20Botulism&deliveryName=USCDC_1052-DM57269
Infant Botulism: Information for Clinicians
Call ⇒
Infant Botulism Treatment and Prevention Program at the California Department of Public Health
Available 24/7
If you suspect your patient has botulism, call immediately. Do not wait for laboratory confirmation.
The on-call physician will provide a no-cost clinical consultation and release BabyBIGexternal icon treatment if the patient’s clinical findings indicate infant botulism.
Call your state health departmentexternal icon to report the suspected case.
Treat ⇒
Prepareexternal icon and administerexternal icon BabyBIG as soon as it is received. Do not wait for laboratory confirmation.
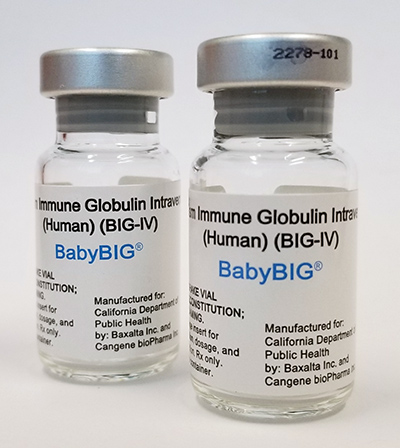
BabyBIG®, human antitoxin for the treatment of infant botulism.
Photo courtesy of the California Department of Public Health.
Test ⇒
Submit specimens for diagnostic testing through your state health department’s laboratory or CDC. All patients receiving BabyBIG must be tested.
Some laboratories, including CDC, do not routinely accept specimens unless BabyBIG has been released.
Questions about testing and reporting should be directed to your state health department.
Receive
The laboratory will report results and notify the state health department of positive results.
Testing can take several days. If you do not hear back within 5 days, contact your state health department.
Ohio History Connection: History + Public Health, Reflecting on One Year of COVID-19
March 13th, 2021
991 subscribers