Archive for July, 2016
Suicide bombers detonated 2 vehicles laden with explosives near the perimeter of the airport enclave killing at least 12.
Wednesday, July 27th, 2016The Special Representative of the UN Secretary-General (SRSG) for Somalia Michael Keating condemned in the strongest possible terms today’s terrorist attack in the vicinity of Mogadishu International Airport that killed at least a dozen people.
Suicide bombers detonated two vehicles laden with explosives near the perimeter of the airport enclave this morning. No United Nations personnel are among the confirmed dead.
“Al-Shabaab have once again carried out a ruthless attack that has claimed the lives of at least a dozen Somalis,” said SRSG Keating. “The overwhelming majority of Somalis have rejected such terrorist tactics and the use of violence to achieve political objectives. This horrific incident is a fresh example of the extremists’ desperate attempts to disrupt political progress. Neither the Somali authorities nor the United Nations will be deterred from moving forward.” Limited franchise elections are due to be held later this year.
“On behalf of the entire UN community in Somalia, I extend our heartfelt condolences to the families and friends of the deceased and wish a speedy recovery to the injured,” said SRSG Keating.
Zika virus disease in the United States, 2015–2016
Wednesday, July 27th, 2016Zika virus disease in the United States, 2015–2016
As of July 20, 2016 (5 am EST)
- Zika virus disease and Zika virus congenital infection are nationally notifiable conditions.
- This update from the CDC Arboviral Disease Branch includes provisional data reported to ArboNET for January 01, 2015 – July 20, 2016.
US States
- Locally acquired mosquito-borne cases reported: 0
- Travel-associated cases reported: 1,403
- Laboratory acquired cases reported: 1
- Total: 1,404
- Sexually transmitted: 15
- Guillain-Barré syndrome: 5
US Territories
- Locally acquired cases reported: 3,815
- Travel-associated cases reported: 12
- Total: 3,827*
- Guillain-Barré syndrome: 14
*Sexually transmitted cases are not reported for areas with local mosquito-borne transmission of Zika virus because it is not possible to determine whether infection occurred due to mosquito-borne or sexual transmission.
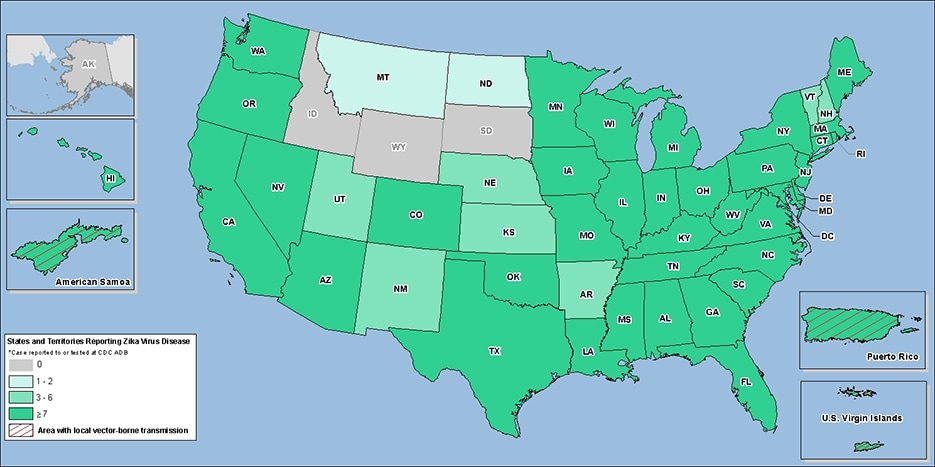
Laboratory-confirmed Zika virus disease cases reported to ArboNET by state or territory — United States, 2015–2016 (as of July 20, 2016)
Over the past few years, there’s been a sharp increase in the number of aid workers being targeted for kidnap and ransom.
Tuesday, July 26th, 2016Aid Worker Security Database: The Aid Worker Security Database (AWSD) records major incidents of violence against aid workers, with incident reports from 1997 through the present.
Aid Worker Security Report (2015)
In 2014, 329 aid workers were victims of major attacks. 121 killed. 88 wounded. 120 kidnapped.
“…Kidnappings have again surpassed shootings as the most common means of violence affecting aid workers. As in past years, most kidnap victims were national staff of aid projects in Afghanistan, and were released following intervention by community elders. The estimated number of humanitarian aid workers in 2013 was 450,000, yielding a global attack rate of 10.5 victims per 10,000 in the field. Although the estimated number of aid workers has not yet been calculated for 2014, it is not expected to drop significantly (given humanitarian funding trends, it is more likely to increase). This means that attack rates will have reduced in 2014 along with absolute numbers.
In 2014, the five contexts with the greatest number of attacks on aid workers were Afghanistan, Syria, South Sudan, Central African Republic and Pakistan…..”

CDC Issues Updated Zika Recommendations: To all men and women who have traveled to or reside in areas with active Zika virus transmission* and their sex partners.
Tuesday, July 26th, 2016Zika virus has been identified as a cause of congenital microcephaly and other serious brain defects (1). CDC issued interim guidance for the prevention of sexual transmission of Zika virus on February 5, 2016, with an initial update on April 1, 2016 (2). The following recommendations apply to all men and women who have traveled to or reside in areas with active Zika virus transmission* and their sex partners. The recommendations in this report replace those previously issued and are now updated to reduce the risk for sexual transmission of Zika virus from both men and women to their sex partners. This guidance defines potential sexual exposure to Zika virus as having had sex with a person who has traveled to or lives in an area with active Zika virus transmission when the sexual contact did not include a barrier to protect against infection. Such barriers include male or female condoms for vaginal or anal sex and other barriers for oral sex.† Sexual exposure includes vaginal sex, anal sex, oral sex, or other activities that might expose a sex partner to genital secretions.§ This guidance will be updated as more information becomes available.
As of July 20, 2016, 15 cases of Zika virus infection transmitted by sexual contact had been reported in the United States.¶ Sexually transmitted Zika virus infection has also been reported in other countries (3). In published reports, the longest interval after symptom onset that sexual transmission from a man might have occurred was 32–41 days (4). Using real-time reverse transcription–polymerase chain reaction (rRT-PCR), which detects viral RNA but is not necessarily a measure of infectivity, Zika virus RNA has been detected in semen up to 93 days after symptom onset (5). In addition, one report describes an asymptomatically infected man with Zika virus RNA detected by rRT-PCR in his semen 39 days following departure from a Zika virus-affected area and who might have sexually transmitted Zika virus to his partner (6). In most cases, serial semen specimens were not collected until Zika virus RNA was no longer detectable so that the precise duration and pattern of infectious Zika virus in semen remain unknown. Zika virus also has been transmitted from a symptomatically infected woman to a male sex partner (7), and Zika virus RNA has been detected in vaginal fluids 3 days after symptom onset and in cervical mucus up to 11 days after symptom onset (8). For sex partners of infected women, Zika virus might be transmitted through exposure to vaginal secretions or menstrual blood. Sexual transmission of infections, including those caused by other viruses, is reduced by consistent and correct use of barriers to protect against infection.
With this update, CDC is expanding its existing recommendations to cover all pregnant couples, which includes pregnant women with female sex partners. This guidance also describes what other couples (those who are not pregnant or planning to become pregnant) can do to reduce the risk for Zika virus transmission. CDC’s recommendations for couples planning to become pregnant have been published separately (9).
Updated Recommendations
Recommendations for pregnant couples. Zika virus infection is of particular concern during pregnancy. Pregnant women with sex partners (male or female) who live in or who have traveled to an area with active Zika virus transmission should consistently and correctly use barriers against infection during sex or abstain from sex for the duration of the pregnancy. These recommendations reduce the risk for sexual transmission of Zika virus during pregnancy, which could have adverse fetal effects. Pregnant women should discuss with their health care provider their own and their sex partner’s history of having been in areas with active Zika virus transmission and history of illness consistent with Zika virus disease**; providers can consult CDC’s guidance for evaluation and testing of pregnant women (10).
Recommendations for couples who are not pregnant and are not planning to become pregnant. Several factors could influence a couple’s level of concern about sexual transmission of Zika virus. The risk for acquiring mosquito-borne Zika virus infection in areas with active transmission depends on the duration and extent of exposure to infected mosquitoes and the steps taken to prevent mosquito bites.†† According to currently available information, most Zika virus infections appear to be asymptomatic, and when illness does occur, it is usually mild, with symptoms lasting from several days to a week; severe disease requiring hospitalization is uncommon (11).
Men and women who want to reduce the risk for sexual transmission of Zika virus should use barrier methods against infection consistently and correctly during sex or abstain from sex when one sex partner has traveled to or lives in an area with active Zika virus transmission. Based on expert opinion and on limited but evolving information about the sexual transmission of Zika virus, the recommended duration of consistent use of a barrier method against infection or abstinence from sex depends on whether the sex partner has confirmed infection or clinical illness consistent with Zika virus disease and whether the sex partner is male or female (Box). The rationale for these time frames has been published previously (9).
Couples who do not desire pregnancy should use available strategies to prevent unintended pregnancy and might consider multiple options, including (in addition to condoms, the only method that protects against both pregnancy and sexual transmission of Zika virus) use of the most effective contraceptive methods that can be used correctly and consistently (9,12). In addition, couples should be advised that correct and consistent use of barrier methods against infection, such as condoms, reduces the risk for other sexually transmitted infections.
Zika Virus Testing and Sexual Transmission
At present, Zika virus testing for the assessment of risk for sexual transmission is of uncertain value, because current understanding of the duration and pattern of shedding of Zika virus in the male and female genitourinary tract is limited. Therefore, testing of specimens to assess risk for sexual transmission is currently not recommended.
Zika virus testing is recommended for persons who have had possible sexual exposure to Zika virus and who develop signs or symptoms consistent with Zika virus disease.§§ All pregnant women should be tested if they have had possible exposure to Zika virus, including sexual exposure (9,10). CDC urges health care providers to report to local and state health departments all cases of Zika virus disease, including those suspected to have occurred by sexual transmission.
Corresponding author: John T. Brooks, zud4@cdc.gov, 404-639-3894.
References
- Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects—reviewing the evidence for causality. N Engl J Med 2016;374:1981–7. CrossRef PubMed
- Oster AM, Russell K, Stryker JE, et al. Update: interim guidance for prevention of sexual transmission of Zika virus—United States, 2016. MMWR Morb Mortal Wkly Rep 2016;65:323–5.CrossRef PubMed
- World Health Organization. Prevention of sexual transmission of Zika virus: interim guidance update. June 7, 2016. Geneva, Switzerland: World Health Organization; 2016.http://apps.who.int/iris/bitstream/10665/204421/1/WHO_ZIKV_MOC_16.1_eng.pdf?ua=1
- Turmel JM, Abgueguen P, Hubert B, et al. Late sexual transmission of Zika virus related to persistence in the semen. Lancet 2016;387:2501. CrossRef PubMed
- Mansuy J, Pasquier C, Daudin M, et al. Zika virus in semen of a patient returning from a non-epidemic area. Lancet Infect Dis 2016;16:894–5. CrossRef
- Fréour T, Mirallié S, Hubert B, et al. Sexual transmission of Zika virus in an entirely asymptomatic couple returning from a Zika epidemic area, France, April 2016. Euro Surveill 2016;21(23).PubMed
- Davidson A, Slavinski S, Komoto K, Rakeman J, Weiss D. Suspected female-to-male sexual transmission of Zika virus—New York City, 2016. MMWR Morb Mortal Wkly Rep 2016;65:716–7.CrossRef PubMed
- Prisant N, Bujan L, Benichou H, et al. Zika virus in the female genital tract. Lancet Infect Dis 2016. Epub July 11, 2016. CrossRef
- Petersen EE, Polen KN, Meaney-Delman D, et al. Update: interim guidance for health care providers caring for women of reproductive age with possible Zika virus exposure—United States, 2016. MMWR Morb Mortal Wkly Rep 2016;65:315–22. PubMed
- Oduyebo T, Igbinosa I, Petersen EE, et al. Update: interim guidance for health care providers caring for pregnant women with possible Zika virus exposure—United States, July 2016. MMWR Morb Mortal Wkly Rep 2016. Epub July 25, 2016.
- Duffy MR, Chen TH, Hancock WT, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med 2009;360:2536–43. CrossRef PubMed
- CDC. Reproductive health: contraception. Atlanta GA: US Department of Health and Human Services, CDC; 2016.http://www.cdc.gov/reproductivehealth/unintendedpregnancy/contraception.htm
* http://www.cdc.gov/zika/geo/index.html.
† Barrier methods to protect against infection include male or female condoms for vaginal or anal sex, male condoms for oral sex (mouth-to-penis), and male condoms cut to create a flat barrier or dental dams for oral sex (mouth-to-vagina).
§ For the purpose of these guidelines, sex is specifically defined as vaginal sex (penis-to vagina sex), anal sex (penis-to-anus sex), oral sex (mouth-to-penis sex or mouth-to-vagina sex), and the sharing of sex toys.
¶ http://www.cdc.gov/zika/geo/united-states.html.
** Clinical illness consistent with Zika virus disease includes one or more of the following signs or symptoms: acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis.
 BOX. Recommendations for prevention of sexual transmission of Zika virus for couples in which one or both partners have traveled to or reside in an area with active Zika virus transmission
BOX. Recommendations for prevention of sexual transmission of Zika virus for couples in which one or both partners have traveled to or reside in an area with active Zika virus transmission
Couples in which a woman is pregnant
- Couples in which a woman is pregnant should use barrier methods against infection consistently and correctly or abstain from sex for the duration of the pregnancy.
Couples who are not pregnant and are not planning to become pregnant*
- Couples in which a partner had confirmed Zika virus infection or clinical illness consistent with Zika virus disease should consider using barrier methods against infection consistently and correctly or abstain from sex as follows:
― Men with Zika virus infection for at least 6 months after onset of illness;
― Women with Zika virus infection for at least 8 weeks after onset of illness. - Couples in areas without active Zika transmission in which one partner traveled to or resides in an area with active Zika virus transmission but did not develop symptoms of Zika virus disease should consider using barrier methods against infection or abstaining from sex for at least 8 weeks after that partner departed the Zika-affected area.
- Couples who reside in an area with active Zika virus transmission might consider using barrier methods against infection or abstaining from sex while active transmission persists.
* Couples who do not desire pregnancy should use the most effective contraceptive methods that can be used correctly and consistently in addition to barrier methods to protect against infections, such as condoms, which reduce the risk for both sexual transmission of Zika and other sexually transmitted infections. Couples planning conception might have multiple factors to consider, which are discussed in more detail in the following: Petersen EE, Polen KN, Meaney-Delman D, et al. Update: interim guidance for health care providers caring for women of reproductive age with possible Zika virus exposure—United States, 2016. MMWR Morb Mortal Wkly Rep 2016;65:315–22.
PAHO/WHO updates the characterization of Zika Congenital Syndrome
Tuesday, July 26th, 2016Washington, 22 July 2016 (PAHO/WHO) — The Pan American Health Organization/World Health Organization (PAHO/WHO) has updated its preliminary characterization of Zika Congenital Syndrome, after an international meeting in Pernambuco.
The event gathered scientists from Brazil, Colombia, Argentina, the United States, PAHO and WHO to investigate the details of Zika virus infection and its effects on the child. The update aims to contribute to improvement of the care provided in health services in the affected regions.
PAHO/WHO is leading a process to gather and review more evidence to clearly define these effects and will update its description as further evidence is produced.
In addition to previously known signs, such as microcephaly and some brain abnormalities described earlier, other aspects characterizing the Zika Congenital Syndrome have been identified.
They include clinical conditions and neuroimaging findings mainly related to the central nervous system such as epilepsy, hearing and visual impairment, and psychomotor development as well as effects on the bones and joints, or the osteoarticular system. These conditions have been characterized and analyzed in terms of frequency and severity in the time periods including antenatal, neonatal (0 to 28 days) and the child’s first year.
The scientists looked at systematic reviews of data on Zika, and shared country experiences from Brazil and Colombia. They heard an overview of the epidemiological situation, presented by PAHO’s Incident Manager for Zika, Dr. Sylvain Aldighieri, and visited health care facilities in Recife that care for infants who have microcephaly and other conditions associated with Zika virus infection.
The experts noted, “The range of abnormalities seen and the likely causal relationship with Zika virus infection suggest the presence of a new congenital syndrome. WHO has set in place a process for defining the spectrum of this syndrome. The process focuses on mapping and analyzing the clinical manifestations encompassing the neurological, hearing, visual and other abnormalities, and neuroimaging findings.”
Information on the complications resulting from Zika virus infection is still limited, and the scientists shared data on diagnosis, description, consequences, physical processes and analysis of evidence from clinicians and researchers on their main findings so far.
“Our aim is to assist the countries in strengthening surveillance of Zika and Zika Congenital Syndrome, in addition to enhancing readiness for dealing with Guillain-Barré cases in health services. The spatial and temporal association of Zika and Guillain-Barré syndrome is evident in various countries,” noted PAHO/WHO’s Aldighieri.
“We had the opportunity to go to IMIP (Instituto de Medicina Integral Professor Fernando Figueira), in Pernambuco, and see the excellent, incredible, work that they are doing in following up and taking care of about 200 children with microcephaly. It’s important that we get this kind of work to other parts of Brazil and the world for children affected with microcephaly,” said PAHO/WHO’s Director of Family, Gender and Life Course, Dr. Andres de Francisco. “We also should remember that Zika is not the only cause of microcephaly and microcephaly is not the only possible sign of Zika,” he added.
Dr. Luis Codina, PAHO/WHO’s deputy representative in Brazil, said, “After almost a year of very strong work done by various groups of researchers, today there is a certain consensus in associating Zika not only with microcephaly, but also with other aspects of a congenital syndrome. PAHO wants to facilitate this process of investigation and generation of knowledge.”
Japan: At least 19 people were killed and 26 injured in a stabbing attack at a facility for disabled people west of Tokyo,
Tuesday, July 26th, 2016Breaking News: Two dead and at least 14 others injured after a shooting at a Fort Myers, Florida, nightclub, according to police
Monday, July 25th, 2016July 25, 1956: The Italian liner Andrea Doria collided with the Swedish ship Stockholm off the New England coast, claiming the lives of 51 people.
Monday, July 25th, 2016Ansbach, Bavaria: A bomb-carrying Syrian dies outside German music festival; 12 wounded
Monday, July 25th, 2016A team from Brazil’s Fiocruz Institute reported that Culex quinquefasciatus mosquitoes are a potential Zika virus vector.
Monday, July 25th, 2016
Culex quinquefasciatus
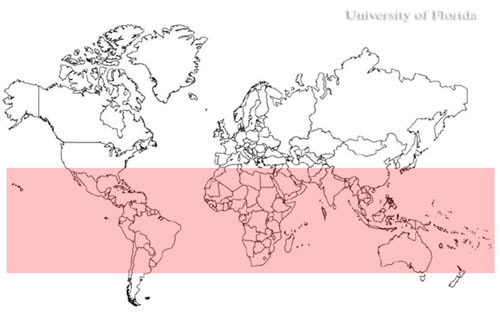
World distribution of the southern house mosquito, Culex quinquefasciatus


