Archive for November, 2017
Everyone Needs Somewhere to Go: World Toilet Day (11/19/17)
Sunday, November 19th, 2017We use toilets every day – at home, school, and work – yet 40% of the world’s population does not have this luxury. Clean and safe toilets are more than just a place to use the restroom. They are essential for health, human dignity, and improved education. Sadly, 2.3 billion people lack even a basic sanitation service, which in many ways represents an ongoing public health crisis that puts much of the world’s population at risk for diseases such as cholera, dysentery, hepatitis, and typhoid fever. Almost 1 billion face the indignity every day of defecating outside without privacy. The 2015 Sustainable Development Goals include a target to ensure universal access to adequate and equitable sanitation and use of safely managed sanitation services by 2030, making sanitation a global development priority. To raise awareness of this issue, the United Nations General Assembly designated November 19 as World Toilet Day.
The Center for Global Health’s Emergency Response and Recovery Branch (ERRB), with support from the National Center for Emerging and Zoonotic Infectious Diseases’ Waterborne Disease Prevention Branch (WDPB), joined the United Nations and other development partners to reach the Sustainable Development Goal by evaluating the safety and acceptability of urine-diverting dry toilets (UDDTs). These types of toilets collect feces (poop) and urine separately for treatment, and because they are installed above ground, they are appropriate for areas where traditional options (e.g., dug pit latrines) are not feasible. This increases the potential for access to clean and safe toilets in difficult environments, such as flood-prone or dry areas.
In 2014, CDC was awarded a grant from Research for Health in Humanitarian Crises (R2HC), an organization working to improve health outcomes by strengthening the evidence for health interventions in humanitarian crises. This grant funds a study of UDDTs in a refugee camp setting to provide guidance on their potential use in humanitarian crises.

WDPB is also involved in efforts to improve sanitation by partnering with a start-up company, Sanivation, to provide in-home container-based urine-diverting toilets to households and to collect and turn the feces into fuel. In 2013, Sanivation received a CDC Innovation Fund Award to begin this waste-to-fuel conversion project in Kenya. Sanivation uses concentrated solar heat to treat the waste and make it safe; then the mix the treated waste with charcoal dust from agricultural waste and transform it into briquettes that widely used for cooking. This method of waste treatment has worked in refugee camp settings and provides a cost-effective and environmentally friendly way to reuse human waste. The project has been so successful, that in 2017, Sanivation received a special CDC Innovation Fund Award to scale-up their waste collection and treatment activities beyond its household subscribers. This new award will enable Sanivation to collect and treat waste from overflowing latrines, leaking septic tanks and other unsafely managed sanitation systems throughout the community, and to expand from one ton of waste collected and treated per month to over four tons. Ultimately, Sanivation plans to expand to other regions of East Africa with the goal of serving over 1 million people by 2020.
Through these efforts, CDC is working to increase the evidence base needed to provide clean and safe toilets and safely managed sanitation services in developing countries with limited resources. CDC’s efforts to improve sanitation are part of a worldwide initiative to break the silence surrounding the sanitation crisis.
To learn more about CDC efforts and other current sanitation initiatives visit:
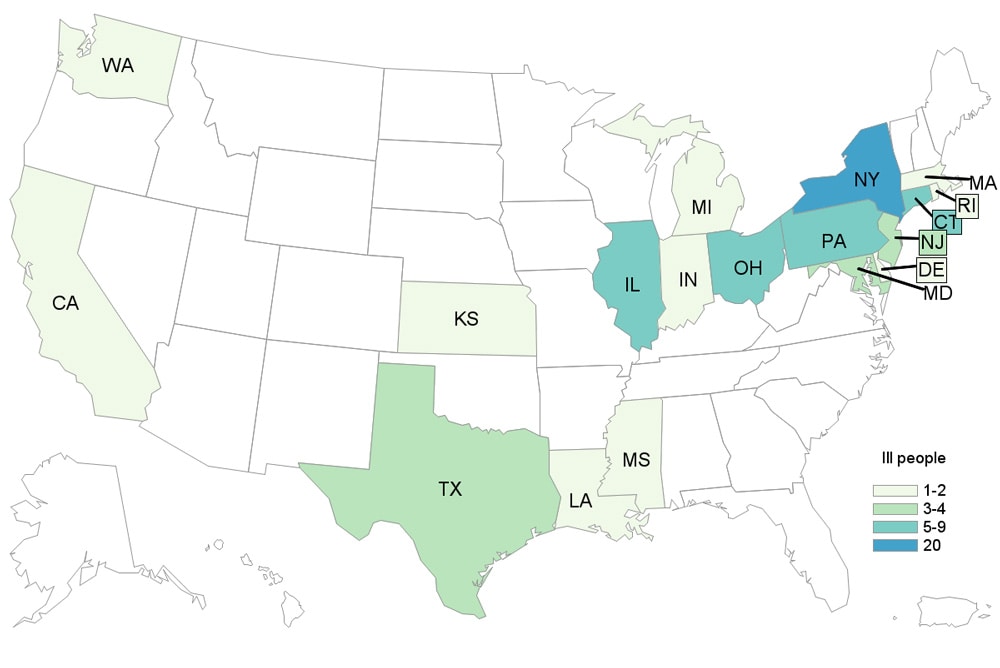
Multistate Outbreak of Salmonella Agbeni Infections Linked to Pet Turtles, 2017
Saturday, November 18th, 2017More than 168,000 people have flown or sailed out of Puerto Rico to Florida since the hurricane.
Saturday, November 18th, 2017About 5,000 barrels of oil, or about 210,000 gallons, gushed out of the Keystone Pipeline on Thursday in South Dakota
Friday, November 17th, 2017Multistate Outbreak of Multidrug-Resistant Salmonella Heidelberg Infections Linked to Contact with Dairy Calves
Friday, November 17th, 2017Since the last update on August 2, 2017, eight more ill people have been reported from six states.
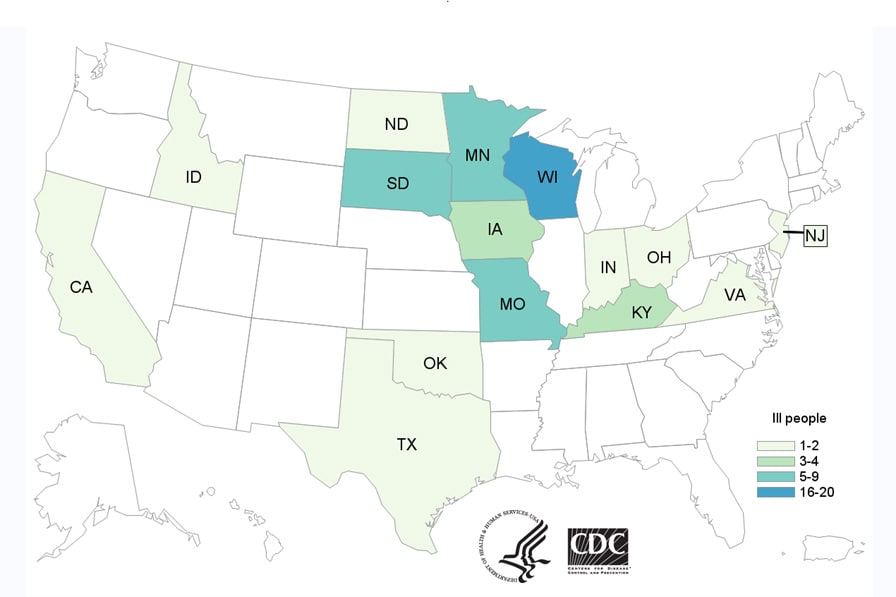
- CDC, several states, and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) are investigating a multistate outbreak of multidrug-resistant Salmonella Heidelberg infections.
- A total of 54 people infected with the outbreak strains of Salmonella Heidelberg have been reported from 15 states.
- Seventeen (35%) people have been hospitalized. No deaths have been reported.
- Illnesses started on dates ranging from January 27, 2015 to October 15, 2017.
- Eighteen (33%) people in this outbreak are children under the age of 5.
- Epidemiologic and laboratory investigations linked ill people in this outbreak to contact with calves, including dairy calves.
- In interviews, ill people answered questions about contact with animals and foods eaten in the week before becoming ill. Of the 54 people interviewed, 34 (63%) reported contact with dairy calves or other cattle. Some of the ill people interviewed reported that they became sick after their dairy calves became sick or died.
- Ongoing surveillance in veterinary diagnostic laboratories showed that calves in several states continue to get sick with the outbreak strains of multidrug resistant Salmonella Heidelberg.
- Information collected earlier in the outbreak indicated that most of the calves came from Wisconsin. Regulatory officials in several states are now tracing the origin of the calves that are linked to the newer illnesses.
- Antibiotic resistance testing(https://www.cdc.gov/narms/resources/glossary.html) conducted by CDC on clinical isolates from ill people shows that the isolates were resistant to multiple types of antibiotics.
- Antibiotic resistance may be associated with increased risk of hospitalization, development of a bloodstream infection, or treatment failure in patients.
- Whole genome sequencing has identified multiple antimicrobial resistance genes in outbreak-associated isolates from 43 ill people, 87 isolates from cattle, and 11 isolates from animal environments.
- These findings match results from standard antibiotic resistance testing(https://www.cdc.gov/narms/resources/glossary.html) methods used by CDC’s National Antimicrobial Resistance Monitoring System (NARMS)(https://www.cdc.gov/narms/index.html) laboratory on clinical isolates from eight ill people in this outbreak.
- All eight isolates from ill people were resistant to amoxicillin-clavulanic acid, ampicillin, cefoxitin, ceftriaxone, streptomycin, sulfisoxazole, and tetracycline, and had reduced susceptibility to ciprofloxacin. Seven isolates were also resistant to trimethoprim-sulfamethoxazole. Five were also resistant to nalidixic acid. Three were also resistant to chloramphenicol. All eight isolates tested were susceptible to azithromycin and meropenem.
- Follow these steps to prevent illness when working with any livestock:
- Always wash your hands thoroughly with soap and water right after touching livestock, equipment, or anything in the area where animals live and roam. Use dedicated clothes, shoes, and work gloves when working with livestock. Keep and store these items outside of your home.
- It is especially important to follow these steps if there are children under age 5 in your household. Young children are more likely to get a Salmonella infection because their immune systems are still developing.
- Work with your veterinarian to keep your animals healthy and prevent diseases.
- This investigation is ongoing and we will provide updates as more information becomes available. Livestock owners should continue to watch for increased sicknesses in dairy calves and consult their veterinarian if needed.
New Zealand: An outbreak of mumps.
Friday, November 17th, 2017What is the current situation?
Public health officials in New Zealand have reported an outbreak of mumps.
Mumps is a contagious disease that is spread when infected people cough, sneeze, or talk. Sharing items, like cups or drink cans, with infected people can also spread the virus. The virus can also live for several hours on items and surfaces touched by an infected person. Symptoms of mumps include fever, headache, muscle aches, tiredness, loss of appetite, and swollen and tender salivary glands (under the ears or jaw) on one or both sides of the face. Some people who get mumps have very mild or no symptoms, and often they do not know they have the disease.
CDC recommends that travelers to New Zealand protect themselves by making sure they are vaccinated against mumps. The only mumps vaccines available in the United States are the measles-mumps-rubella (MMR) and the measles-mumps-rubella-varicella (MMRV) vaccines. Children should get two doses of MMR vaccine, starting with the first dose at 12 through 15 months of age, and the second dose at 4 through 6 years of age. Teens and adults also should be up to date on their MMR vaccinations (two doses at least 28 days apart).
What can travelers do to protect themselves?
- Before you travel, make sure you have already been vaccinated. If you are not, get the MMR vaccine.
- While traveling, wash your hands often. If soap and water aren’t available, use hand sanitizer (containing at least 60% alcohol) to clean hands.
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hand) when coughing or sneezing.
- Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups, with people who are sick.
Learn more about preventing mumps and what to do if you think you have it on the mumps page for travelers.
Traveler Information
- CDC Mumps Homepage
- Information for Travelers on Mumps
- Mumps Vaccination Information
- Mumps Vaccine Information Statement
Clinician Information
- Mumps(https://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/mumps.htm) in CDC Health Information for International Travel (“Yellow Book”)
- CDC Mumps Homepage
- Mumps Clinical Information
- Mumps in Epidemiology and Prevention of Vaccine-Preventable Diseases (“Pink Book”)
After the earthquake in Iran: The new wing of the Imam Khomeini hospital partly crumpled like “an empty soft-drink can in the hands of a child” while the original hospital building, 40 years old, stood beside the wreckage, barely damaged.
Thursday, November 16th, 2017-
The magnitude 7.3 earthquake killed more than 500 people in Iran and eight in neighboring Iraq.
-
More than 40,000 properties became uninhabitable including many newly built state hospitals, schools, apartment complexes and even army barracks.
-
The earthquake has laid bare what many Iranians have been saying for a long time: Corruption inside state organizations has led to shoddy construction work and undermined Iran’s infrastructure.
WHO: Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities
Thursday, November 16th, 2017Focus on AMR – evidence, guidelines and publications
Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities
The eight recommendations are:
- Adopt multipart strategies to prevent and control CRE, CRAB, or CRPsA infection or colonization that includes at least hand hygiene, surveillance (especially for CRE), contact precautions, patient isolation (single room or cohorting), and environmental cleaning
- Implement hand hygiene best practices spelled out in earlier WHO guidance
- Conduct surveillance for CRE-CRAB-CRPsA infection and colonization, especially targeting those with previous CRE colonization, contacts of CRE patients, or those with a history of recent hospitalization in CRE-endemic settings
- Implement contact precautions when caring for infected or colonized patients
- Isolate infected or colonized patients, either in a single room or with others who have the same pathogen
- Comply with environmental cleaning protocols in the “patient zone” of infected or colonized patients, though the optimal cleaning agent was not identified
- Take surveillance cultures of the environment to detect contamination
- Monitor the impact of the interventions
Carbapenem-resistant gram-negative bacteria, namely, carbapenem-resistant Enterobacteriaceae (CRE), Acinetobacter baumannii (CRAB) and Pseudomonas aeruginosa (CRPsA), are an emerging cause of health-care acquired infection that pose a significant threat to public health. The first ever global guidelines for the prevention and control of CRE-CRAB-CRPsA in health care facilities were published on 14 November 2017. They include 8 recommendations distilled by the world’s leading experts from a review of the latest evidence. They are designed to provide evidence-based recommendations on the early recognition and specific required infection prevention and control practices (IPC) and procedures to effectively prevent the occurrence and control the spread of CRE-CRAB-CRPsA colonization and/or infection in acute health care facilities. They provide an evidence-based framework to help inform the development and/or strengthening of national and facility IPC policies and programmes to control the transmission of CRE-CRAB-CRPsA in a variety of health care settings. The recommendations included in these guidelines build upon the overarching standards set by the WHO publication Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level.
These guidelines are intended to support IPC improvement at the facility level, targeting infection prevention leads, senior managers, other health care professionals and patients alike. They are also relevant to policy makers, regulatory and professional bodies at the national level, among others. We encourage you all to use and promote these guidelines.
Teleclass: Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities
Tehama, CA: This incident, as tragic and as bad as it is, could have been so much worse.
Wednesday, November 15th, 2017“…..a much bigger death toll was averted when the killer was unable to break into an elementary school. The staff at tiny Rancho Tehama Elementary School west of Corning moved quickly when they heard gunfire nearby just before classes were set to begin…”