Archive for June, 2018
CDC Pandemic Flu Fighters
Thursday, June 28th, 2018Influenza poses one of the world’s greatest infectious disease challenges. The 1918 flu pandemic is a stark reminder of the devastation that can result from a global flu pandemic. CDC and its public health partners around the world work diligently to monitor and prepare for the next flu pandemic. Highlighted below are some of CDC’s flu fighters, dedicated public health professionals contributing to pandemic flu prevention and response at home and around the world.
Amra Uzicanin, MD, MPH, Team Lead, CDC’s Community Interventions for Infection Control Unit
As Lead of CDC’s Community Interventions for Infection Control Unit (CI-ICU), Dr. Amra Uzicanin is dedicated to developing the scientific evidence base and policies for use of nonpharmaceutical interventions (NPIs), for infectious disease control in community settings with a focus on pandemic flu. NPIs, also known as community mitigation measures, are the first line of defense to help slow the spread of pandemic influenza (flu). NPIs are readily available everywhere and can be used before a pandemic vaccine is available. CI-ICU works hard to prevent and reduce the spread of infectious diseases in communities by empowering people and communities to take action grounded in evidence-based knowledge of NPIs. Dr. Uzicanin says the 1918 flu pandemic “was a pandemic where ordinary people and communities as well as government authorities, public health officials, and healthcare professionals were striving to find new ways to fight off the flu and prevent its impact worldwide.”
Anita Patel, PharmD, MS, Team Lead, CDC’s Pandemic Medical Care and Countermeasures
Dr. Anita Patel is one of CDC’s key problem solvers working to protect the United States from a future influenza pandemic. Her responsibilities include making sure the nation has strategies in place for medical countermeasures to be able to treat sick patients and protect health care workers. Dr. Patel says the 1918 flu pandemic is a sobering reminder of the dangers of flu. “Learning from history allows us to plan for the possible range of impacts, and move the needle in preparedness.”
Anne Schuchat, MD (RADM, USPHS) CDC Principal Deputy Director
Principal Deputy Director of CDC, Dr. Anne Schuchat, is one of the many veterans of CDC’s fight on flu. Combatting influenza is a hallmark of Dr. Schuchat’s 30 years at CDC. In reflecting on the 1918 influenza pandemic, Dr. Schuchat says studying what happened can help us to better prepare the nation and the world for similar scenarios in the future.
Daniel Jernigan, MD, MPH (CAPT, USPHS), Director, Influenza Division
Dr. Dan Jernigan, a captain in the United States Public Health Service (USPHS), serves as director of the Influenza Division in CDC’s National Center for Immunization and Respiratory Diseases. In this role, Jernigan is always working to prepare for the next influenza pandemic. “We are determined to intervene where we can to stop the spread of disease—that’s public health,” he says. For CDC’s Influenza Division, stopping the spread of disease means, “tracking influenza viruses and human illness with influenza viruses worldwide – be it from seasonal, avian, swine, or other novel flu viruses. We track illness, study the virus, assess the risk posed by the virus, make vaccine viruses that are then used to manufacture flu vaccines and help make policies for influenza prevention and treatment.”
James Stevens, Ph.D., Associate Director, Laboratory Sciences in CDC’s Influenza Division
CDC’s influenza laboratories play a leading role in the ongoing global task of looking for new flu viruses, assessing the risk they pose to people, and supporting efforts to proactively prepare for the emergence of flu viruses considered to have pandemic potential. This includes everything from conducting surveillance on novel influenza viruses, to developing the viruses that are used to mass-produce flu vaccines, which are called “candidate vaccine viruses” or “CVVs”. As Associate Director for Laboratory Sciences in CDC’s Influenza Division, Dr. James Stevens oversees and coordinates CDC’s influenza laboratory operations. He says the 1918 flu pandemic “is the deadliest we’ve seen in modern times. We have to remember it because it is the worst-case scenario situation, and we don’t want it to happen again.”
Lisa Koonin, DrPH, MN, MPH, Deputy Director, Influenza Coordination Unit
Martin Cetron, MD, Director, Division of Global Migration and Quarantine (DGMQ)
Air travel today can easily facilitate the spread of diseases around the world with each flight. CDC’s Division of Global Migration and Quarantine (DGMQ) helps protect the health of our communities in a globally mobile world. As director of DGMQ, Dr. Martin (Marty) Cetron is a leader in global health and migration with a focus on emerging infections, tropical diseases, and vaccine-preventable diseases in mobile populations. He says the 1918 influenza (flu) pandemic was “monumental, and as an unprecedented event in human history, it taught us some really important lessons.
Stephen Redd, MD (RADM, USPHS) Director, Office of Public Health Preparedness and Response
CDC’s Dr. Stephen Redd has deep and diverse experiences in responding to public health emergencies, including the 2009 H1N1 influenza pandemic during which he served as incident commander for the CDC’s response. For the past four years, Dr. Redd has directed CDC’s Office of Public Health Preparedness and Response, the group responsible for ensuring CDC is prepared to respond to a public health emergency.
Terrence Tumpey, Ph.D., Chief, Influenza Immunology and Pathogenesis Branch
Dr. Terrence Tumpey is a microbiologist and chief of the Immunology and Pathogenesis Branch (IPB) in the Centers for Disease Control and Prevention’s Influenza Division. He’s perhaps best known for his groundbreaking work reconstructing the 1918 pandemic influenza virus. In 1918, this virus was responsible for the pandemic that is estimated to have killed at least 50 million people worldwide. In 2004, Dr. Tumpey was the first to physically reconstruct, or “rescue” the 1918 virus, using reverse genetics to build an H1N1 virus with all the same genes as the pandemic virus. After the reconstruction was completed, Dr. Tumpey was the first person to study the live 1918 H1N1 virus in the laboratory.
WHO, the UN Food and Agriculture Organization (FAO), the World Organisation for Animal Health (OIE), and the Global Alliance for Rabies Control (GARC) are joining forces to support countries as they seek to accelerate their actions towards the elimination of dog-mediated rabies by 2030.
Thursday, June 28th, 2018“……The Global Strategic Plan set three objectives for affected countries, development partners, and key stakeholders: (1) to effectively use vaccines, medicines, tools, and technologies that will stop dog rabies transmission and reduce the risk of human rabies deaths; (2) to generate evidence-based guidance and high-quality data to measure impact and inform policy decisions; and (3) to harness multistakeholder engagement to sustain commitment and resources...…”
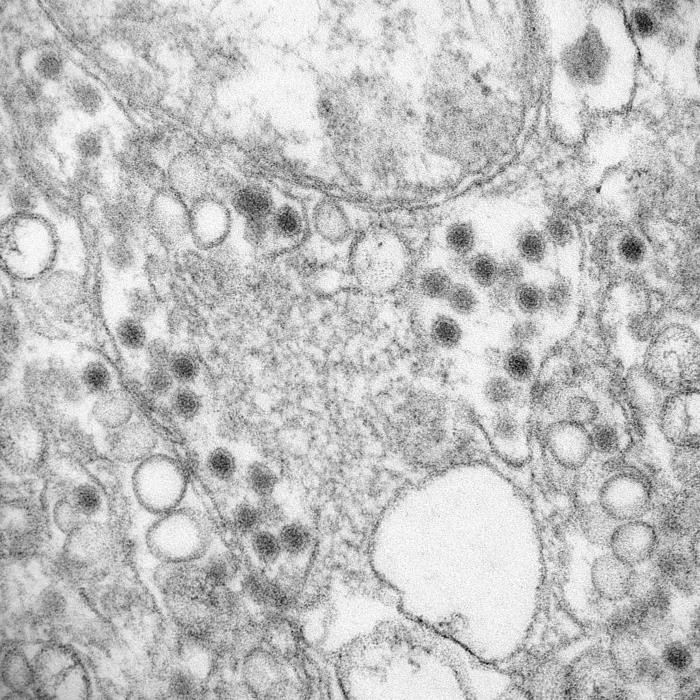
Scientists have captured the clearest and most detailed image yet of Zika that could contribute to the development of more effective vaccines and treatments to combat the virus.
Wednesday, June 27th, 2018
This is a transmission electron microscopic (TEM) image of Zika virus, grown in LLC-MK2 culture cells, which is a member of the family Flaviviridae. Virus particles are 40 nm in diameter, with an outer envelope, and an inner dense core. Also note the smooth membrane vesicles, which are known to be the replication complex for this virus.
Credit: CDC/Goldsmith, Rollin
Myanmar’s “tip of the spear:” hundreds of battle-hardened soldiers from two light infantry divisions – the 33rd and 99th – famed for their brutal counter-insurgency campaigns against this nation’s many ethnic minorities including the Rohingyas
Wednesday, June 27th, 2018“….When Rohingya militants launched attacks across northern Rakhine State in August last year, the 33rd and 99th spearheaded the response. Their ensuing crackdown drove 700,000 Rohingya into neighboring Bangladesh…..”
“….The European Union and Canada on June 25 imposed sanctions on seven senior Myanmar military and police officers, including the commanders of the 33rd and 99th. The seven face asset freezes and are banned from traveling to EU countries. So far, the United States has sanctioned only one Myanmar general for abuses during the Rakhine campaign……”
We Will Destroy Everything : Amnesty International Document
At least 45,000 people have fled the upsurge in fighting in Syria’s southwestern Deraa province, heading toward the border with Jordan.
Tuesday, June 26th, 2018The world’s most dangerous countries for women: a global poll of about 550 experts on women’s issues.
Tuesday, June 26th, 2018- India is the most dangerous country for women in terms of sexual violence and slave labor
- Afghanistan
- Syria
- Somalia
- Saudi Arabia. ……
- Just one Western nation appeared in the top 10: the US, which ranked joint third for a question on the risk of sexual violence, coercion, and harassment.
Plan International: Adolescent Rohingya girls are being kept in stifling conditions in refugee camps in Bangladesh, unable to go out, deprived of education and facing prospects of early marriage whether they want it or not.
Tuesday, June 26th, 2018“……The report, Adolescent Girls in Crisis: Voices of the Rohingya is based on interviews with 300 refugee girls between 10 and 19 years old living in camps outside Cox’s Bazar……..”
Forced Displacement in 2017
Tuesday, June 26th, 2018“…….In its annual Global Trends report, released today, UNHCR, the UN Refugee Agency said 68.5 million people were displaced as of the end of 2017. Among them were 16.2 million people who became displaced during 2017 itself, either for the first time or repeatedly – indicating a huge number of people on the move and equivalent to 44,500 people being displaced each day, or a person becoming displaced every two seconds.
Refugees who have fled their countries to escape conflict and persecution accounted for 25.4 million of the 68.5 million. This is 2.9 million more than in 2016, also the biggest increase UNHCR has seen in a single year. Asylum-seekers, who were still awaiting the outcome of their claims to refugee status as of 31 December 2017, meanwhile rose by around 300,000 to 3.1 million. People displaced inside their own country accounted for 40 million of the total, slightly fewer than the 40.3 million in 2016…….”
A polio case in Papua New Guinea, and the virus is circulating in the community
Tuesday, June 26th, 2018Papua New Guinea confirms poliovirus outbreak, launches response

PORT MORESBY, 25 June 2018 – The National Department of Health of Papua New Guinea and the World Health Organization (WHO) today confirmed that the strain of poliovirus first detected in a child from Morobe Province in April is now circulating in the same community.
The one confirmed case is a 6-year-old boy with lower limb weakness, first detected on 28 April 2018. A vaccine-derived poliovirus type 1 (VDPV1) had been isolated as the cause of the paralysis on 21 May 2018.
On 22 June 2018, the United States Centers for Disease Control and Prevention confirmed that the same virus was also isolated from stool specimens of two healthy children from the same community. This means that the virus is circulating in the community—representing an outbreak of the virus.
“We are deeply concerned about this polio case in Papua New Guinea, and the fact that the virus is circulating,” said Pascoe Kase, Secretary of the National Department of Health (NDOH). “Our immediate priority is to respond and prevent more children from being infected.”
The NDOH has formally informed WHO and has been working with WHO and other partners in launching a response. Some of the immediate steps include conducting large-scale immunization campaigns and strengthening surveillance systems that help detect the virus early. These activities are also being strengthened in neighbouring provinces.
“Since the detection of poliovirus in April, WHO has been working with the Government on the investigation, laboratory confirmation, enhanced surveillance and response activities,” said Dr Luo Dapeng, WHO Representative in Papua New Guinea. “We will continue to support the Government to ensure children are protected.”
Papua New Guinea has not had a case of wild poliovirus since 1996, and the country was certified as polio-free in 2000 along with the rest of the WHO Western Pacific Region.
In Morobe Province, polio vaccine coverage is low, with only 61% of children having received the recommended 3 doses. Water, sanitation and hygiene are also challenges in the area.
Public health response
Outbreak response activities are ongoing in Morobe Province. Experts from the NDOH, Papua New Guinea’s Central Public Health Laboratory, Provincial Health Authorities, UNICEF and WHO have conducted field missions to undertake clinical investigation, house-to-house surveys, sample collection and contact tracing.
The team also collected stool specimens from family members of the patient and from the community. A “mop up” immunization campaign was done in the community targeting children under 15 years old. To date, 845 children from the Lufa Mountain Settlement have been vaccinated.
Circulating vaccine-derived poliovirus
Oral polio vaccine (OPV) contains an attenuated (weakened) vaccine-virus, which activates an immune response in the body. When a child is immunized with OPV, the weakened vaccine-virus replicates in the intestine for a limited period, thereby developing immunity by building up antibodies. During this time, the vaccine-virus is also excreted. In areas of inadequate sanitation, this excreted vaccine-virus can spread in the immediate community (and this can offer protection to other children through ‘passive’ immunization), before eventually dying out.
On rare occasions, if a population is seriously under-immunized, an excreted vaccine-virus can continue to circulate for an extended period of time. The longer it is allowed to survive, the more genetic changes it undergoes. In very rare instances, the vaccine-virus can genetically change into a form that can paralyze—this is what is known as a circulating vaccine-derived poliovirus (cVDPV).
Because of relatively limited travel to and from this area and the planned immunization activities, WHO assesses the risk of international spread of the cVDPV from Papua New Guinea to other countries to be low.
However, it is important that all countries—in particular those with frequent travel and contacts with polio-affected countries and areas—strengthen surveillance for cases of AFP to rapidly detect any virus importation and facilitate a rapid response. Countries, territories and areas should maintain high immunization coverage to minimize the consequences of any new virus introduction.
WHO recommends that all travellers to polio-affected areas be fully vaccinated against polio. Residents (and visitors for more than 4 weeks) from infected areas should receive an additional dose of OPV or inactivated polio vaccine (IPV) within 4 weeks to 12 months of travel.
For further information, please contact:
National Department of Health, AOPI Centre, Waigani, Port Moresby
Email: Jacob_Marcos@health.gov.pg / jcbmarcos@gmail.com
Phone: +675 301-3745 / +675 7206-8115
World Health Organization, 4th Floor AOPI Centre, Waigani, Port Moresby
Email: rezam@who.int / taukarair@who.int
Phone: +675 325-7827 / +675 7197-1499 / +675 7543-7337
Reporting Forced Displacement – Key Definitions
Monday, June 25th, 2018UNHCR does not use the term ‘migrant’ to describe people who are forced to flee.
- Refugee: A person who has fled their country and needs ‘international protection’ because of a risk of violence or persecution were they to return home. This includes people fleeing wars. The term has its roots in international legal instruments, notably the 1951 Refugee Convention and its 1967 Protocol and the 1969 OAU Convention. You can acquire refugee status by applying for it individually, or in cases of large influx by being given it on a “prima facie” basis. Refugees cannot be returned to their home country unless it is on a strictly voluntary basis.
- Asylum Seeker: A person who has applied on an individual basis for refugee status and is awaiting the result. Asylum seekers are given ‘international protection’ while their claims are being assessed, and like refugees may not be returned home unless it is on a voluntary basis.
- Internally displaced person: Internally displaced people, often known by the abbreviation IDPs, are those who are forced to flee their homes to elsewhere in their own country.
- Stateless person: Someone who is without a nationality of any country, and consequently lacks the human rights and access to services of those who have citizenship. It is possible to be stateless and a refugee simultaneously.