Archive for January, 2019
Rift Valley Fever: It’s even more dangerous to fetuses than Zika.
Friday, January 11th, 2019“…….Testing on human placental tissue revealed that, unlike the Zika virus, Rift Valley fever virus has a unique ability to infect a specialized layer of cells that supports the region of the placenta where nutrients flow in.
Zika must take the “side roads” into the placenta to infect a fetus, while the Rift Valley fever virus can take the “expressway,” Dr. Hartman said.
“The fetus is protected from hundreds of thousands of dangers that could affect it,” she added. “Only a few microbes can get past, and this is one of them.”…….”
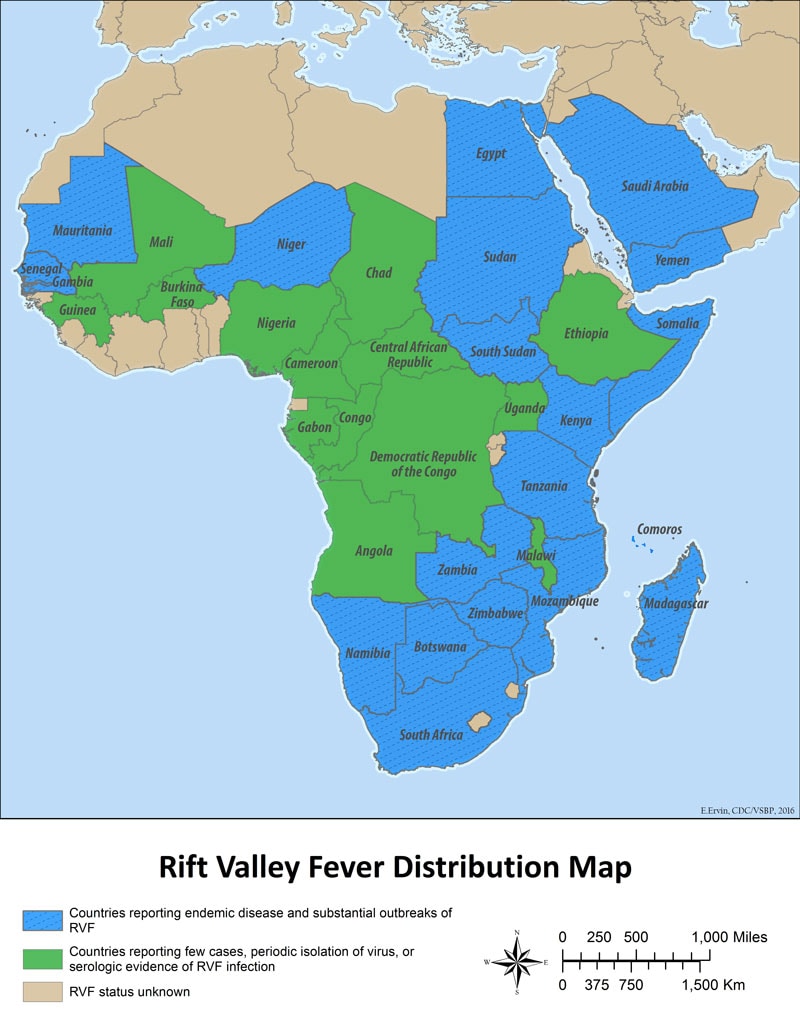
Rift Valley Fever: Document
1/10/1962: An avalanche on the slopes of Mt. Huascaran destroys villages and towns killing more than 4,000 people in Peru
Thursday, January 10th, 2019Pharmacy Needs After a Natural Disaster — Puerto Rico, September–October 2017.
Thursday, January 10th, 2019Lavery AM, Patel A, Boehmer TK, et al. Notes from the Field: Pharmacy Needs After a Natural Disaster — Puerto Rico, September–October 2017. MMWR Morb Mortal Wkly Rep 2018;67:402–403. DOI: http://dx.doi.org/10.15585/mmwr.mm6713a4.
- After Hurricane Ivan made landfall near Mobile, Alabama, in 2004, an assessment of its impact on pharmacies in the affected areas found that 53% had depleted supplies and at least 26% had to prioritize distribution to patients because of limited supplies
- A 2005 study of Hurricane Katrina evacuees in San Antonio, Texas, found that disaster medical assistance teams were more prepared to provide for acute than chronic illnesses although more than two thirds (68%) of patients requested drugs to treat chronic conditions
- On September 20, 2017, Hurricane Maria made landfall in Puerto Rico as a Category 4 hurricane. Five days later, only approximately 29% of pharmacies reporting to Healthcare Ready, an organization that provides information on access to pharmacies during an emergency, were open.
- During June–August 2017, the top categories of drugs prescribed were for
- cardiovascular (average = 21% of prescriptions filled),
- psychiatric (12%), and
- analgesic (10%) drugs.
- Among the cardiovascular drugs prescribed, a majority were angiotensin II receptor antagonists (29%), beta blockers (20%), and angiotensin-converting enzyme (ACE) inhibitors (18%).
- The most frequently dispensed individual drugs were thyroid replacement hormones (230,324 prescriptions dispensed, 5% of total dispensed), gabapentin (144,114 prescriptions dispensed, 3% of total), and metformin (141,734 prescriptions dispensed, 3% of total).
- Ninety percent of prescribed drugs were for oral administration.
- The IQVIA database used in this analysis is limited to retail facilities and does not include hospitals or other institutions such as nursing homes.
- Furthermore, some critical drugs might not be represented in this data set, including insulin, which can also be purchased over the counter; hence, some of the prescribed quantities in this data set could be an underestimate of medication needs. Although insulin was not a most frequently purchased or prescribed drug, it is a daily need for persons with insulin-dependent diabetes and should be prioritized.
- To have a more complete picture of important drugs that might be needed after a disaster, multiple data sources, including drug sales data to hospitals, clinics, and nursing homes, as well as information provided by third-party claims adjudication data, could be analyzed to inform public health activities and guide collaborations with drug suppliers to respond to and recover from large-scale disasters.
Statement of the Nineteenth IHR Emergency Committee Regarding the International Spread of Poliovirus
Thursday, January 10th, 2019The nineteenth meeting of the Emergency Committee under the International Health Regulations (2005) (IHR) regarding the international spread of poliovirus was convened by the Director General on 27 November 2018 at WHO headquarters with members, advisers and invited Member States attending via teleconference.
The Emergency Committee reviewed the data on wild poliovirus (WPV1) and circulating vaccine derived polioviruses (cVDPV). The Secretariat presented a report of progress for affected IHR States Parties subject to Temporary Recommendations. The following IHR States Parties provided an update on the current situation and the implementation of the WHO Temporary Recommendations since the Committee last met on 15 August 2018: Afghanistan, Democratic Republic of the Congo (DR Congo), Nigeria, Niger, Papua New Guinea (PNG), and Somalia.
Wild polio
The Committee commended the continued high level commitment seen in Afghanistan and Pakistan, and the significant degree of cooperation and coordination, particularly in reaching high risk mobile populations that frequently cross the international border. The committee noted that it is four years since there has been international spread outside of these two epidemiologically linked countries.
However, the Committee was very concerned by the increase in WPV1 cases globally in 2018, especially regarding the increased number of WPV cases in Afghanistan. Furthermore, after a 10-month period of no international spread of wild poliovirus between the two neighbors, Pakistan and Afghanistan, cross border spread in both directions has occurred in the last three months.
In Pakistan the situation in 2018 has stagnated, with the number of cases so far at the same level in 2018 as for the whole of 2017. Furthermore, positive environmental isolates in 2018 continue to be widely spread geographically indicating multiple areas of transmission and missed susceptible population groups. Nevertheless, the performance of the eradication program has shown some improvement in areas such as SIA quality.
In Afghanistan, the number of polio cases has almost doubled in 2018, with 19 cases reported so far, compared to 10 at the same time last year, due to worsened security and greater inaccessibility, and persistent pockets of refusals and missed children. Environmental surveillance is also finding an increased proportion of positive samples. The security situation and access would need to significantly improve for eradication efforts to progress, as currently 1 million children under 5 years old are inaccessible in recent polio immunization campaigns.
It is now more than two years since the last WPV1 was detected in an accessible area of Nigeria, and four years since there has been any international spread of WPV1 from the country. The Committee commended the strong efforts to reach inaccessible and trapped children in Borno, Nigeria, even in the face of increased insecurity, and noted that the inaccessible target population was now down to around 70,000 children, scattered across Borno in smaller pockets.
Vaccine derived poliovirus
The outbreaks of cVDPV2 in Somalia, Kenya, DR Congo, Niger and cVDPV1 in PNG and cVDPV3 in Somalia continue to be of major concern, particularly the apparent international spread between Somalia and Kenya and the recent spread from Nigeria into Niger of cVDPV2, given that traditionally cVDPV viruses have rarely spread across borders. Conflict and population movement within and outside DR Congo indicate a degree of risk of spread.
Large inaccessible areas of Somalia are a significant constraint on achieving interruption of transmission of the cVDPV2 and cVDPV3 in the area, exacerbated by large population movements into and out of these areas.
Nevertheless because of the limited supply of IPV, in cVDPV type 2 outbreaks the implementation of the Temporary Recommendations for border immunization of departing travelers can be difficult. The committee noted the progress made with cross border cooperation between PNG and Indonesia, but was concerned that new cases of cVDPV1 in new provinces of PNG had been detected in the last three months, and that surveillance indicators in Indonesian provinces neighboring PNG were sub-optimal. Similarly, countries neighboring Somalia, such as South Sudan, Ethiopia and Djibouti, have areas of weak surveillance which poses the risk that international spread may go undetected. The outbreak of cVDPV2 in Syria has been successfully controlled with no international spread, and Syria is no longer considered infected but remains vulnerable.
The committee noted that in all infected countries, routine immunization was weak. The outbreaks of cVDPV2 in Jigawa, and for the second time in Sokoto, Nigeria, again underlines the vulnerability of northern Nigeria to poliovirus transmission. Routine immunization coverage remains very poor in many areas of the country, although the political leadership and national emergency programme to strengthen routine immunisation is beginning to make an impact in some areas.
Conclusion
The Committee unanimously agreed that the risk of international spread of poliovirus remains a Public Health Emergency of International Concern (PHEIC), and recommended the extension of Temporary Recommendations for a further three months. The Committee considered the following factors in reaching this conclusion:
- Although the declaration of the PHEIC and issuance of Temporary Recommendations has reduced the risk of international spread of WPV, progress is fragile, and should international spread now occur, the impact on WPV eradication would be even more grave in terms of delaying certification and prolonging requirements for dedicated human and financial resources in support of the eradication effort. The reversal in progress in Afghanistan and the stagnation in Pakistan with exportation of WPV continuing between the two countries, heighten concerns.
- There is a risk of global complacency as the numbers of WPV cases remains low and eradication becomes a tangible reality, and a concern that removal of the PHEIC now could contribute to greater complacency.
- Many countries remain vulnerable to WPV importation. Gaps in population immunity in several key high-risk areas is evidenced by the current number of cVDPV outbreaks of all serotypes, which only emerge and circulate when polio population immunity is low as a result of deficient routine immunization programmes.
- The international outbreak of cVDPV2 affecting Somalia and Kenya, with a highly diverged cVDPV2 that appears to have circulated undetected for up to four years, highlights that there are still high-risk populations in South and Central zones of Somalia where population immunity and surveillance are compromised by conflict.
- Similarly the new spread of cVDPV2 between Nigeria and Niger highlights the significant risk of persisting type 2 outbreaks two years after OPV2 withdrawal, and the inability so far to prevent further spread within and outside Nigeria through application of consistently high quality mOPV2 SIAs is a concern.
- The difficulty in controlling spread of cVDPV2 in DR Congo heightens these concerns and demonstrates significant gaps in population immunity at a critical time in the polio endgame;the low coverage with routine IPV vaccination in several countries neighboring DR Congo heightens the risk of international spread, as population immunity is rapidly waning.
- Inaccessibility continues to be a major risk, particularly in several countries currently infected with WPV or cVDPV, i.e. Afghanistan, Nigeria and Somalia, which all have sizable populations that have been unreached with polio vaccine for prolonged periods.
- The increasing number of countries in which immunization systems have been weakened or disrupted by conflict and complex emergencies pose another risk. Populations in these fragile states are vulnerable to outbreaks of polio.
- The risk is amplified by population movement, whether for family, social, economic or cultural reasons, or in the context of populations displaced by insecurity and returning refugees. There is a need for international coordination to address these risks.A regional approach and strong crossborder cooperation is required to respond to these risks, as much international spread of polio occurs over land borders.
Risk categories
The Committee provided the Director-General with the following advice aimed at reducing the risk of international spread of WPV1 and cVDPVs, based on the risk stratification as follows:
- States infected with WPV1, cVDPV1 or cVDPV3, with potential risk of international spread.
- States infected with cVDPV2, with potential risk of international spread.
- States no longer infected by WPV1 or cVDPV, but which remain vulnerable to re-infection by WPV or cVDPV.
Criteria to assess States as no longer infected by WPV1 or cVDPV:
- Poliovirus Case: 12 months after the onset date of the most recent case PLUS one month to account for case detection, investigation, laboratory testing and reporting period OR when all reported AFP cases with onset within 12 months of last case have been tested for polio and excluded for WPV1 or cVDPV, and environmental or other samples collected within 12 months of the last case have also tested negative, whichever is the longer.
- Environmental or other isolation of WPV1 or cVDPV (no poliovirus case): 12 months after collection of the most recent positive environmental or other sample (such as from a healthy child) PLUS one month to account for the laboratory testing and reporting period
- These criteria may be varied for the endemic countries, where more rigorous assessment is needed in reference to surveillance gaps (e.g. Borno)
Once a country meets these criteria as no longer infected, the country will be considered vulnerable for a further 12 months. After this period, the country will no longer be subject to Temporary Recommendations, unless the Committee has concerns based on the final report.
TEMPORARY RECOMMENDATIONS
States infected with WPV1, cVDPV1 or cVDPV3 with potential risk of international spread
WPV1
Afghanistan (most recent detection 25 Oct 2018)
Pakistan (most recent detection 25 Oct 2018)
Nigeria (most recent detection 27 Sept 2016)
cVDPV1
Papua New Guinea (most recent detection 1 Oct 2018)
cVDPV3
Somalia (most recent detection 7 Sept 2018)
These countries should:
- Officially declare, if not already done, at the level of head of state or government, that the interruption of poliovirus transmission is a national public health emergency and implement all required measures to support polio eradication; where such declaration has already been made, this emergency status should be maintained as long as the response is required.
- Ensure that all residents and longterm visitors (i.e. > four weeks) of all ages, receive a dose of bivalent oral poliovirus vaccine (bOPV) or inactivated poliovirus vaccine (IPV) between four weeks and 12 months prior to international travel.
- Ensure that those undertaking urgent travel (i.e. within four weeks), who have not received a dose of bOPV or IPV in the previous four weeks to 12 months, receive a dose of polio vaccine at least by the time of departure as this will still provide benefit, particularly for frequent travelers.
- Ensure that such travelers are provided with an International Certificate of Vaccination or Prophylaxis in the form specified in Annex 6 of the IHR to record their polio vaccination and serve as proof of vaccination.
- Restrict at the point of departure the international travel of any resident lacking documentation of appropriate polio vaccination. These recommendations apply to international travelers from all points of departure, irrespective of the means of conveyance (e.g. road, air, sea).
- Further intensify crossborder efforts by significantly improving coordination at the national, regional and local levels to substantially increase vaccination coverage of travelers crossing the border and of high risk crossborder populations. Improved coordination of crossborder efforts should include closer supervision and monitoring of the quality of vaccination at border transit points, as well as tracking of the proportion of travelers that are identified as unvaccinated after they have crossed the border.
- Further intensify efforts to increase routine immunization coverage, including sharing coverage data, as high routine immunization coverage is an essential element of the polio eradication strategy, particularly as the world moves closer to eradication.
- Maintain these measures until the following criteria have been met: (i) at least six months have passed without new infections and (ii) there is documentation of full application of high quality eradication activities in all infected and high risk areas; in the absence of such documentation these measures should be maintained until the state meets the above assessment criteria for being no longer infected.
- Provide to the Director-General a regular report on the implementation of the Temporary Recommendations on international travel.
States infected with cVDPV2s, with potential risk of international spread
- DR Congo(most recent detection 25 Sept 2018)
- Kenya(most recent detection 21 March 2018)
- Nigeria(most recent detection 17 Oct 2018)
- Niger(most recent detection 9 Sept 2018)
- Somalia(most recent detection 4 Oct 2018)
These countries should:
- Officially declare, if not already done, at the level of head of state or government, that the interruption of poliovirus transmission is a national public health emergency and implement all required measures to support polio eradication; where such declaration has already been made, this emergency status should be maintained.
- Noting the existence of a separate mechanism for responding to type 2 poliovirus infections, consider requesting vaccines from the global mOPV2 stockpile based on the recommendations of the Advisory Group on mOPV2.
- Encourage residents and longterm visitors to receive a dose of IPV (if available in country) four weeks to 12 months prior to international travel; those undertaking urgent travel (i.e. within four weeks) should be encouraged to receive a dose at least by the time of departure.
- Ensure that travelers who receive such vaccination have access to an appropriate document to record their polio vaccination status.
- Intensify regional cooperation and crossborder coordination to enhance surveillance for prompt detection of poliovirus, and vaccinate refugees, travelers and crossborder populations, according to the advice of the Advisory Group.
- Further intensify efforts to increase routine immunization coverage, including sharing coverage data, as high routine immunization coverage is an essential element of the polio eradication strategy, particularly as the world moves closer to eradication.
- Maintain these measures until the following criteria have been met: (i) at least six months have passed without the detection of circulation of VDPV2 in the country from any source, and (ii) there is documentation of full application of high quality eradication activities in all infected and high risk areas; in the absence of such documentation these measures should be maintained until the state meets the criteria of a ‘state no longer infected’.
- At the end of 12 months without evidence of transmission, provide a report to the Director-General on measures taken to implement the Temporary Recommendations.
States no longer infected by WPV1 or cVDPV, but which remain vulnerable to re-infection by WPV or cVDPV
WPV1
- Cameroon (last case 9 Jul 2014)
- Central African Republic (last case 8 Dec 2011)
- Chad (last case 14 Jun 2012)
CVDPV
- Syria (last case 21 Sept 2017)
These countries should:
- Urgently strengthen routine immunization to boost population immunity.
- Enhance surveillance quality, including considering introducing supplementary methods such as environmental surveillance, to reduce the risk of undetected WPV1 and cVDPV transmission, particularly among high risk mobile and vulnerable populations.
- Intensify efforts to ensure vaccination of mobile and crossborder populations, Internally Displaced Persons, refugees and other vulnerable groups.
- Enhance regional cooperation and cross border coordination to ensure prompt detection of WPV1 and cVDPV, and vaccination of high risk population groups.
- Maintain these measures with documentation of full application of high quality surveillance and vaccination activities.
- At the end of 12 months* without evidence of reintroduction of WPV1 or new emergence and circulation of cVDPV, provide a report to the Director-General on measures taken to implement the Temporary Recommendations.
*For the Lake Chad countries, this will be linked to when Nigeria is considered no longer infected by WPV1 or cVDPV2.
Additional considerations
In areas where specific geographies are inaccessible, an intensive effort should be made to immunize communities on the periphery of inaccessible areas including providing immunisation posts at key transit points of high population movement.
The outbreak in Papua New Guinea is an example of the ongoing vulnerability of some parts of the world to polioviruses. The committee urged countries in close proximity to the current outbreaks, such as Ethiopia, South Sudan, Djibouti, Indonesia, Central African Republic and Lake Chad basin countries to urgently strengthen polio surveillance and routine immunization including with bOPV and IPV. There needs to be a renewed urgency to addressing these gaps wherever they exist. The world is at a critical point in polio eradication, and failure to boost population immunity through strengthening routine immunization, and where outbreaks have occurred through implementation of high quality SIAs, in areas of known high risk could jeopardize or severely delay polio eradication. The current situation calls for unabated efforts and use of every tool available, to achieve the goal in these most challenging countries.
The Committee noted that the extension of the PHEIC for over four years in the context of the end game of the global eradication effort, was an exceptional use of the IHR. The committee noted that there is a legitimate debate about whether this continued declaration of a PHEIC may weaken its impact as a tool to address global health emergencies, and specifically whether it continues to have utility noting that the risk of international spread appears to have substantially diminished since 2014. It noted that it was not originally envisaged that a PHEIC would continue for such a long period, but the committee feels that the circumstances of an eradication program such as polio are unique. In an eradication program, it is the mere existence of the virus in a country that necessitates strenuous emergency measures, in addition to the number of cases. The committee was concerned that the removal of the PHEIC in the current situation where exportation of WPV and cVDPV continues and progress has may even have reversed, might send out the wrong message to the global community and might weaken the gains made in reducing the risk of international spread in some areas. There is sound evidence that the Temporary Recommendations have been an important factor in reducing the risk of international spread since 2014 [1],[2].
Based on the current situation regarding WPV1 and cVDPV, and the reports provided by Afghanistan, DR Congo, Nigeria, Niger, Papua New Guinea and Somalia, the Director-General accepted the Committee’s assessment and on 27 November 2018 determined that the situation relating to poliovirus continues to constitute a PHEIC, with respect to WPV1 and cVDPV. The Director-General endorsed the Committee’s recommendations for countries meeting the definition for ‘States infected with WPV1, cVDPV1 or cVDPV3 with potential risk for international spread’, ‘States infected with cVDPV2 with potential risk for international spread’ and for ‘States no longer infected by WPV1 or cVDPV, but which remain vulnerable to re-infection by WPV or cVDPV’ and extended the Temporary Recommendations under the IHR to reduce the risk of the international spread of poliovirus, effective 27 November 2018.
[1] Wilder-Smith A, Leong WY, Lopez LF, et al. Potential for international spread of wild poliovirus via travelers. BMC Med 2015; 13: 133.
[2] Duintjer Tebbens RJ, Thompson KM. Modeling the costs and benefits of temporary recommendations for poliovirus exporting countries to vaccinate international travelers. Vaccine 2017; 35(31): 3823-33
Hantavirus disease – Republic of Panama
Thursday, January 10th, 2019Hantavirus disease – Republic of Panama
The Panama Ministry of Health has reported an increase in cases of hantavirus infection in Los Santos Province, Republic of Panama, to the Pan American Health Organization / World Health Organization (PAHO/WHO). Between 1 January and 22 December 2018, a total of 103 confirmed cases of hantavirus have been reported at the national level, 99 of which were reported in Los Santos Province. In Los Santos Province, 51 cases were classified as hantavirus fever1 (HF) without pulmonary syndrome and 48 cases were classified as hantavirus pulmonary syndrome2 (HPS), including four deaths.
- Of the 51 HF cases, 41% were female, 55% aged between 20-59 years, with 76% occurring between June 2018 and November 2018.
- Of the 48 HPS cases, 56% were female, 67% aged between 20-59 years, with more than half of the cases occurring in February 2018 (17%) and between June 2018 and September 2018 (42%).
- Four deaths were reported among HPS cases (two female, two male, all aged over 60 years).
Cases were confirmed by serology and polymerase chain reaction (PCR)3. Sequencing determined that the type of virus associated with this outbreak is Choclo virus. It was first isolated in 1999 in the western Republic of Panama.
Hantavirus cases have been reported in the Republic of Panama since 1999 (Figure 1). In the last five years, transmission has been documented in Los Santos, Herrera, Veraguas, and Cocle provinces. During 2018, cases have been reported in Los Santos (99 cases, Figure 2), Herrera (two cases), Cocle (one case) and Veraguas (one case) provinces (Figure 3). Since the reservoir for hantavirus is sylvatic rodents and transmission can occur when people come in contact with rodent habitats, the current increase in hantavirus cases in the Republic of Panama could be related to changes in the abundance and distribution of rodent species, as well as strengthened surveillance and laboratory capacity at the provincial level. Environmental and ecological factors affecting rodent populations can have a seasonal impact on disease trends.
Figure 1. Distribution of HF and HPS cases by year, Republic of Panama, 1999-2018 (as of November).

Figure 2. Distribution of confirmed hantavirus cases by epidemiological week, Los Santos Province, Republic of Panama, January–December 2018.
Source: Provided by the Panama Ministry of Health and reproduced by PAHO/WHO
Figure 3. Geographical distribution of confirmed hantavirus cases, Republic of Panama, January–November 2018.
Source: Provided by the Panama Ministry of Health and reproduced by PAHO/WHO
Public health response
The public health responses currently being implemented include:
- Investigation and monitoring of cases, including case management.
- Enhanced surveillance and active case finding.
- Rodent control and mitigation measures.
- Increasing awareness and health promotion in the affected areas.
References:
- Pan American Health Organization / World Health Organization (PAHO/WHO). Epidemiological Alert Hantavirus Pulmonary Syndrome (HPS). 17 October 2013.
- Hantavirus in the Americas: Guidelines for diagnosis, treatment, prevention and control.
- Hantavirus information: Centers for Disease Control and Prevention (CDC)
In the city of Magnitogorsk: The explosion that collapsed a high-rise building wasn’t terrorism, but a crumbling infrastructure
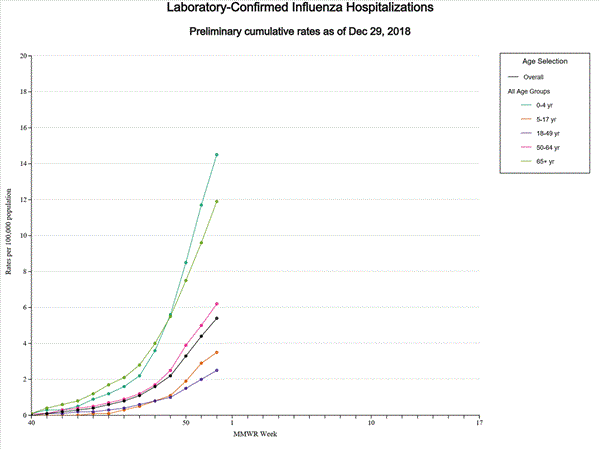
Sunday, January 6th, 20192018-2019 Influenza Season Week 52 ending December 29, 2018
Saturday, January 5th, 2019Influenza activity in the United States is increasing. Influenza A(H1N1)pdm09, influenza A(H3N2), and influenza B viruses continue to co-circulate. Below is a summary of the key influenza indicators for the week ending December 29, 2018:
- Viral Surveillance: The percentage of respiratory specimens testing positive for influenza viruses in clinical laboratories is increasing. Influenza A viruses have predominated in the United States since the beginning of October. Influenza A(H1N1)pdm09 viruses have predominated in most areas of the country, however influenza A(H3) viruses have predominated in the southeastern United States (HHS Region 4).
- Virus Characterization: The majority of influenza viruses characterized antigenically and genetically are similar to the cell-grown reference viruses representing the 2018–2019 Northern Hemisphere influenza vaccine viruses.
- Antiviral Resistance: All viruses tested show susceptibility to the neuraminidase inhibitors (oseltamivir, zanamivir, and peramivir).
- Influenza-like Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) increased to 4.1%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above their region-specific baseline level. The increase in the percentage of patient visits for ILI may be influenced in part by a reduction in routine healthcare visits during the winter holidays, as has occurred during previous seasons.
- ILI State Activity Indictor Map: New York City and 19 states experienced high ILI activity; nine states experienced moderate ILI activity; the District of Columbia and 10 states experienced low ILI activity; and Puerto Rico and 12 states experienced minimal ILI activity.
- Geographic Spread of Influenza: The geographic spread of influenza in 24 states was reported as widespread; Puerto Rico and 18 states reported regional activity; six states reported local activity; the District of Columbia, the U.S. Virgin Islands and two states reported sporadic activity; and Guam did not report.
- Influenza-associated Hospitalizations A cumulative rate of 5.4 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported. The highest hospitalization rate is among children younger than 5 years (14.5 hospitalizations per 100,000 population).
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Two influenza-associated pediatric deaths were reported to CDC during week 52.
WHO: Psychological first aid: Guide for field workers
Saturday, January 5th, 2019Overview
This guide (2011) covers psychological first aid which involves humane, supportive and practical help to fellow human beings suffering serious crisis events. It is written for people in a position to help others who have experienced an extremely distressing event. It gives a framework for supporting people in ways that respect their dignity, culture and abilities.
Endorsed by many international agencies, the guide reflects the emerging science and international consensus on how to support people in the immediate aftermath of extremely stressful events.
Humanitarian Intervention Guide (mhGAP-HIG): Clinical management of mental, neurological and substance use conditions in humanitarian emergencies.
Saturday, January 5th, 2019World Health Organization and United Nations High Commissioner for Refugees. mhGAP Humanitarian Intervention Guide (mhGAP-HIG): Clinical management of mental, neurological and substance use conditions in humanitarian emergencies. Geneva: WHO, 2015.
The target group for WHO work on mental health and psychosocial support in emergencies is any population exposed to extreme stressors, such as refugees, internally displaced persons, disaster survivors and terrorism-, war- or genocide-exposed populations.
The WHO Department of Mental Health and Substance Abuse emphasizes that the number of persons exposed to extreme stressors is large and that exposure to extreme stressors is a risk factor for mental health and social problems. The Department’s work on mental health in emergencies focuses mostly on resource-poor countries, where most populations exposed to natural disasters and war live.
Management of physical health conditions in adults with severe mental disorders
Preventable physical health conditions lead to premature mortality in people with severe mental disorders, reducing their life span by 10-20 years. The majority of these premature deaths are due to physical health conditions.
The physical health of people with severe mental disorders is commonly overlooked, not only by themselves and people around them, but also by health systems, resulting in crucial physical health disparities and limited access to health services. Many lives can be saved by ensuring that people with severe mental disorders receive treatment.
WHO’s “Guidelines on management of physical health conditions in adults with severe mental disorders” provide evidence-based, up-to-date recommendations to practitioners on how to recognize and manage comorbid physical and mental health conditions.
WHO: Mental Health of Refugees and Migrants
Saturday, January 5th, 2019Being a refugee or a migrant does not, in itself, make individuals significantly more vulnerable to mental disorders, but refugees and migrants can be exposed to various stress factors that influence their mental well-being.
Refugees and migrants have often faced war, persecution and hardship in their country of origin. Many will have experienced displacement and difficulties in transit countries and embarked on dangerous travels. Lack of information, uncertainty about immigration status, potential hostility, changing policies, and undignified and protracted detention all contribute to additional stress.
Furthermore, forced migration requires multiple adaptations in short periods of time, making them more vulnerable to abuse and neglect. Pre-existing social and mental health problems can thus be exacerbated.
Clinical Management of Mental, Neurological and Substance Use Conditions in Humanitarian Emergencies