Archive for May, 2019
Peru and Ecuador have recorded cases of Mayaro virus (MAYV) in 2019.
Saturday, May 4th, 2019Pan American Health Organization / World Health Organization. Epidemiological Alert:
Mayaro fever. 1 May 2019, Washington, D.C.: PAHO/WHO; 2019
Mayaro fever is a zoonosis caused by an arbovirus of the Alphavirus genus, Togavirus family. Transmission by Haemagogus mosquitoes has been documented. Human cases are associated with recent exposures to humid forest environments inhabited by these vectors.
In the first days, the disease presents as a nonspecific clinical picture similar to other arboviruses: fever, headache, myalgia, retro-ocular pain, chills, severe arthralgia, dizziness, nausea, photophobia, anorexia, often incapacitating joint edema, rash (mainly on the chest, legs, back, arms and less frequently in the face), abdominal pain, leukopenia and thrombocytopenia, and in some cases mild hemorrhagic disease symptoms have been described.
The incubation period is relatively short, ranging between 1 to 12 days. The disease is self-limiting, with a duration from 3 to 5 days, with persistence of arthralgia that can remain for weeks or months; a fatal case with encephalopathy has been documented.
Symptomatic management with nonsteroidal anti-inflammatory drugs (NSAIDS), rest,
hydration, and supportive treatment of possible complications is recommended, following
the exclusion of more severe diseases such as malaria, dengue, or bacterial infections.
There is no specific antiviral treatment for Mayaro virus infection.
In 2019, 2 cases were confirmed in Peru in the provinces of Quispicanchis (Cusco Region)
and La Mar (Ayacucho Region) (16).
Additionally, on 26 April 2019, Ecuador reported that of 34 samples that were negative for
dengue, chikungunya, Zika, and leptospirosis, 5 were positive for Mayaro.

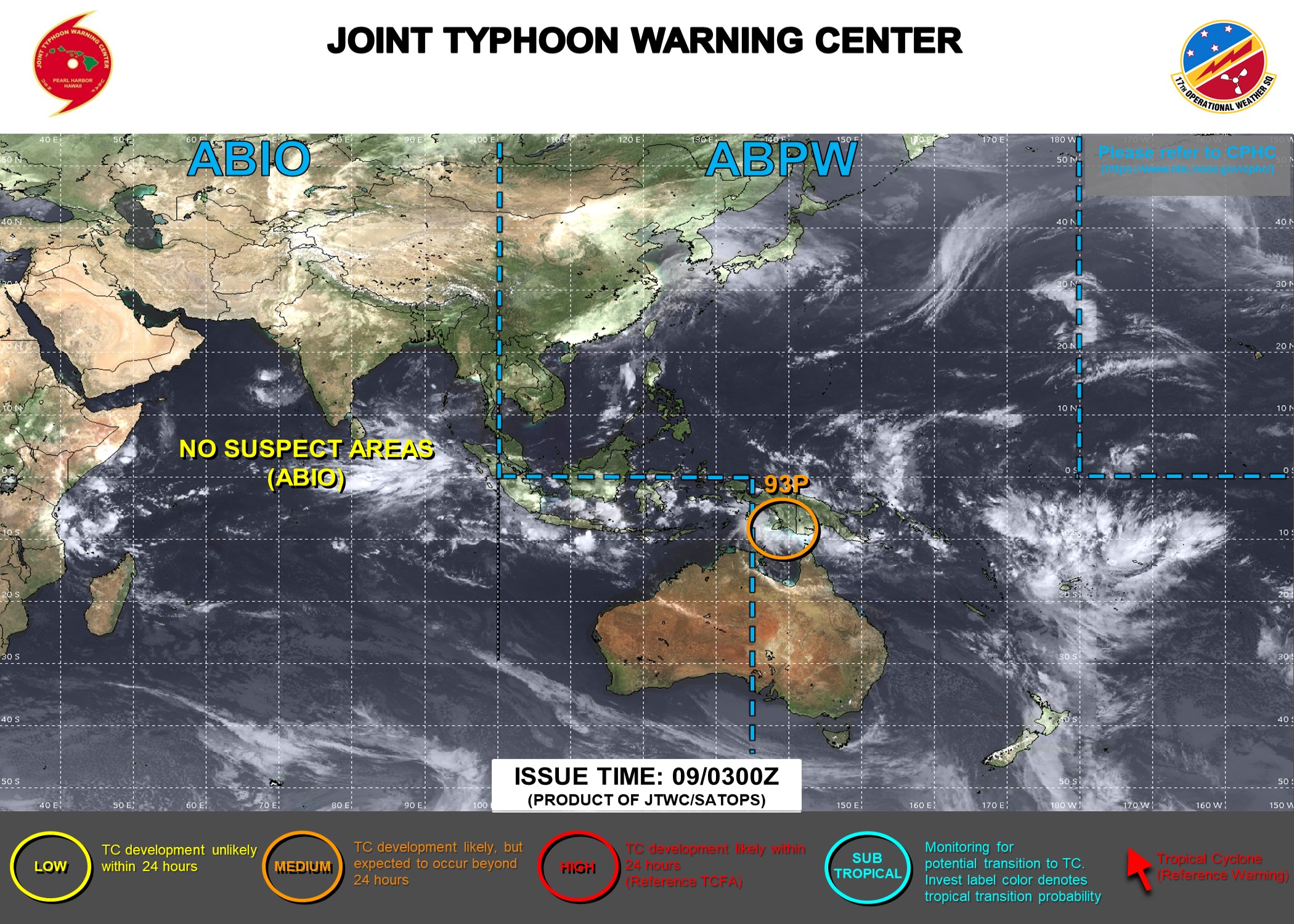
Fani (the strongest to hit the area in 20 years) slams into India and at least 2 dead so far and millions heading inland.
Friday, May 3rd, 2019“…….On Thursday, Tropical Cyclone Fani had strengthened significantly in the Bay of Bengal, with maximum sustained winds of 250 kilometers per hour (155 mph) and gusts of up to 305 kilometers per hour (190 mph)…….
5/3/1962: Two commuter trains and a freight train collide near Tokyo, Japan, killing more than 160 people and injuring over 300
Friday, May 3rd, 2019First FDA-approved vaccine for the prevention of dengue disease in endemic regions
Friday, May 3rd, 2019- May 01, 2019
The U.S. Food and Drug Administration announced today the approval of Dengvaxia, the first vaccine approved for the prevention of dengue disease caused by all dengue virus serotypes (1, 2, 3 and 4) in people ages 9 through 16 who have laboratory-confirmed previous dengue infection and who live in endemic areas. Dengue is endemic in the U.S. territories of American Samoa, Guam, Puerto Rico and the U.S. Virgin Islands.
“Dengue disease is the most common mosquito-borne viral disease in the world and global incidence has increased in recent decades,” said Anna Abram, FDA deputy commissioner for policy, legislation, and international affairs. “The FDA is committed to working proactively with our partners at the U.S. Centers for Disease Control and Prevention, as well as international partners, including the World Health Organization, to combat public health threats, including through facilitating the development and availability of medical products to address emerging infectious diseases. While there is no cure for dengue disease, today’s approval is an important step toward helping to reduce the impact of this virus in endemic regions of the United States.”
The CDC estimates more than one-third of the world’s population is living in areas at risk for infection by dengue virus which causes dengue fever, a leading cause of illness among people living in the tropics and subtropics. The first infection with dengue virus typically results in either no symptoms or a mild illness that can be mistaken for the flu or another viral infection. A subsequent infection can lead to severe dengue, including dengue hemorrhagic fever (DHF), a more severe form of the disease that can be fatal. Symptoms may include stomach pain, persistent vomiting, bleeding, confusion and difficulty breathing. Approximately 95 percent of all severe/hospitalized cases of dengue are associated with second dengue virus infection. Because there are no specific drugs approved for the treatment of dengue disease, care is limited to the management of symptoms.
Each year, an estimated 400 million dengue virus infections occur globally according to the CDC. Of these, approximately 500,000 cases develop into DHF, which contributes to about 20,000 deaths, primarily among children. Although dengue cases are rare in the continental U.S., the disease is regularly found in American Samoa, Puerto Rico, Guam, the U.S. Virgin Islands, as well as Latin America, Southeast Asia and the Pacific islands.
“Infection by one type of dengue virus usually provides immunity against that specific serotype, but a subsequent infection by any of the other three serotypes of the virus increases the risk of developing severe dengue disease, which may lead to hospitalization or even death,” said Peter Marks, M.D., director of the FDA’s Center for Biologics Evaluation and Research. “As the second infection with dengue is often much more severe than the first, the FDA’s approval of this vaccine will help protect people previously infected with dengue virus from subsequent development of dengue disease.”
The safety and effectiveness of the vaccine was determined in three randomized, placebo-controlled studies involving approximately 35,000 individuals in dengue-endemic areas, including Puerto Rico, Latin America and the Asia Pacific region. The vaccine was determined to be approximately 76 percent effective in preventing symptomatic, laboratory-confirmed dengue disease in individuals 9 through 16 years of age who previously had laboratory-confirmed dengue disease. Dengvaxia has already been approved in 19 countries and the European Union.
The most commonly reported side effects by those who received Dengvaxia were headache, muscle pain, joint pain, fatigue, injection site pain and low-grade fever. The frequency of side effects was similar across Dengvaxia and placebo recipients and tended to decrease after each subsequent dose of the vaccine.
Dengvaxia is not approved for use in individuals not previously infected by any dengue virus serotype or for whom this information is unknown. This is because in people who have not been infected with dengue virus, Dengvaxia appears to act like a first dengue infection – without actually infecting the person with wild-type dengue virus – such that a subsequent infection can result in severe dengue disease.Therefore, health care professionals should evaluate individuals for prior dengue infection to avoid vaccinating individuals who have not been previously infected by dengue virus. This can be assessed through a medical record of a previous laboratory-confirmed dengue infection or through serological testing (tests using blood samples from the patient) prior to vaccination.
Dengvaxia is a live, attenuated vaccine that is administered as three separate injections, with the initial dose followed by two additional shots given six and twelve months later.
The FDA granted this application Priority Review and a Tropical Disease Priority Review Voucher under a program intended to encourage development of new drugs and biologics for the prevention and treatment of certain tropical diseases. The approval was granted to Sanofi Pasteur.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
###
Flooding in Iowa and the waters in Davenport continue to rise
Friday, May 3rd, 2019https://www.youtube.com/watch?v=uVD3JgZfGqc
Hundreds of thousands of people evacuated parts of India’s eastern coast Thursday as Fani moves in.
Thursday, May 2nd, 2019DRC: April was the deadliest month of the 9-month long Ebola outbreak
Thursday, May 2nd, 2019“…..April total: 406 cases, 308 deaths
Today’s cases raise the outbreak total to 1,495, of which 1,429 are confirmed and 66 are probable. There have been 984 deaths, and 306 suspected cases are still under investigation…..”
There have now been 31,056 measles cases, including 415 deaths (case-fatality rate, 1.34%) reported in the Philippines since Jan 1
Thursday, May 2nd, 2019Overview
Current measles outbreak started late 2017 in Mindanao. In 2018, 20,827 cases were reported with 199 deaths. Outbreak and supplementary immunization activities in 2018 were ineffective in addressing the outbreak as the immunization activity was met with increased vaccine hesitancy due to the Dengue vaccine controversy. Weak routine immunization leading to a decrease in overall immunization coverage over the last decade resulted in large immunity gaps among younger children against vaccine preventable diseases including measles.
The Philippines Department of Health (DoH) declared measles outbreaks in 5 Regions (Region NCR, III, IVA, VI, VII) on 7 February 2019, whereas cases are being reported from all 17 Regions. DoH issued guidelines for nation-wide measles vaccination accompanied by Oral Polio Vaccine (OPV) and Vitamin A distribution until end March 2019, prioritizing unvaccinated children between 6 and 59 months; schoolchildren from kindergarten to grade 6; and adults who voluntarily wish to be vaccinated against measles.
Current Situation
Between 1 January and 13 April 2019, 31,056 measles cases including 415 deaths were officially reported through the routine surveillance system from the DoH, with a Case Fatality Rate (CFR) of 1,34% (see Table 1).
The number of cases is 368% higher in 2019 than during the same time period in 2018.
With a median age of 3 years old, 52% of measles cases are under 5 years of age. 53% of measles cases are male.
With a median age of 1 year old, 83% of all deaths are children under the age of 5, 59% of measles deaths are male. Most deaths are reported from Region III, IV-A, VIII and NCR.