Archive for the ‘Zika virus’ Category
Zika virus was discovered in the salivary glands of five mosquito species caught in the wild in Mexico, including three previously unreported
Friday, January 19th, 2018Zika Virus in Salivary Glands of Five Different Species of Wild-Caught Mosquitoes from Mexico
Scientific Reports 8, Article number: 809 (2018)
doi:10.1038/s41598-017-18682-3
“…..The authors conclude, “To the best of our knowledge this is the first report that shows the presence of ZIKV [Zika virus] in the salivary glands of wild-caught female mosquitoes Cx. coronator, Cx. tarsalis, and Ae. vexans, as well as and in Ae. aegypti and Cx. quinquefasciatus, which have already been reported as potential vectors for ZIKV.….”
Zika Toddlers: How are they faring?
Friday, December 15th, 2017“……The study, the first to comprehensively assess some of the oldest Zika babies in Brazil, focused on 15 of the most disabled children born with abnormally small heads, a condition called microcephaly. At about 22 months old, these children had the cognitive and physical development of babies younger than 6 months. They could not sit up or chew, and they had virtually no language…..”
EPA Registers the Wolbachia ZAP Strain in Live Male Asian Tiger Mosquitoes in order to reduce their population thereby reducing the spread numerous diseases of significant human health concern
Thursday, November 9th, 2017
For Release: November 7, 2017
On November 3, 2017, EPA registered a new mosquito biopesticide – ZAP Males® – that can reduce local populations of the type of mosquito (Aedes albopictus, or Asian Tiger Mosquitoes) that can spread numerous diseases of significant human health concern, including the Zika virus.
ZAP Males® are live male mosquitoes that are infected with the ZAP strain, a particular strain of the Wolbachia bacterium. Infected males mate with females, which then produce offspring that do not survive. (Male mosquitoes do not bite people.) With continued releases of the ZAP Males®, local Aedes albopictus populations decrease. Wolbachia are naturally occurring bacteria commonly found in most insect species.
This time-limited registration allows MosquitoMate, Inc. to sell the Wolbachia-infected male mosquitoes for five years in the District of Columbia and the following states: California, Connecticut, Delaware, Illinois, Indiana, Kentucky, Massachusetts, Maine, Maryland, Missouri, New Hampshire, New Jersey, Nevada, New York, Ohio, Pennsylvania, Rhode Island, Tennessee, Vermont, and West Virginia. Before the ZAP Males® can be used in each of those jurisdictions, it must be registered in the state or district.
When the five-year time limit ends, the registration will expire unless the registrant requests further action from EPA.
EPA’s risk assessments, along with the pesticide labeling, EPA’s response to public comments on the Notice of Receipt, and the proposed registration decision, can be found on www.regulations.gov under docket number EPA-HQ-OPP-2016-0205.
CDC recommendations to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas during the period of September 2017 – March 2018.
Wednesday, October 25th, 2017Advice for Providers Treating Patients in or Recently Returned from Hurricane-Affected Areas, Including Puerto Rico and US Virgin Islands
Distributed via the CDC Health Alert Network
October 24, 2017, 1330 ET (1:30 PM ET)
CDCHAN-00408
Summary
The Centers for Disease Control and Prevention (CDC) is working with federal, state, territorial, and local agencies and global health partners in response to recent hurricanes. CDC is aware of media reports and anecdotal accounts of various infectious diseases in hurricane-affected areas, including Puerto Rico and the US Virgin Islands (USVI). Because of compromised drinking water and decreased access to safe water, food, and shelter, the conditions for outbreaks of infectious diseases exist.
The purpose of this HAN advisory is to remind clinicians assessing patients currently in or recently returned from hurricane-affected areas to be vigilant in looking for certain infectious diseases, including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. Additionally, this Advisory provides guidance to state and territorial health departments on enhanced disease reporting.
Background
Hurricanes Irma and Maria made landfall in Puerto Rico and USVI in September 2017, causing widespread flooding and devastation. Natural hazards associated with the storms continue to affect many areas. Infectious disease outbreaks of diarrheal and respiratory illnesses can occur when access to safe water and sewage systems are disrupted and personal hygiene is difficult to maintain. Additionally, vector borne diseases can occur due to increased mosquito breeding in standing water; both Puerto Rico and USVI are at risk for outbreaks of dengue, Zika, and chikungunya.
Health care providers and public health practitioners should be aware that post-hurricane environmental conditions may pose an increased risk for the spread of infectious diseases among patients in or recently returned from hurricane-affected areas; including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. The period of heightened risk may last through March 2018, based on current predictions of full restoration of power and safe water systems in Puerto Rico and USVI.
In addition, providers in health care facilities that have experienced water damage or contaminated water systems should be aware of the potential for increased risk of infections in those facilities due to invasive fungi, nontuberculous Mycobacterium species, Legionella species, and other Gram-negative bacteria associated with water (e.g., Pseudomonas), especially among critically ill or immunocompromised patients.
Cholera has not occurred in Puerto Rico or USVI in many decades and is not expected to occur post-hurricane.
Recommendations
These recommendations apply to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas (e.g., within the past 4 weeks), during the period of September 2017 – March 2018.
- Health care providers and public health practitioners in hurricane-affected areas should look for community and healthcare-associated infectious diseases.
- Health care providers in the continental US are encouraged to ask patients about recent travel (e.g., within the past 4 weeks) to hurricane-affected areas.
- All healthcare providers should consider less common infectious disease etiologies in patients presenting with evidence of acute respiratory illness, gastroenteritis, renal or hepatic failure, wound infection, or other febrile illness. Some particularly important infectious diseases to consider include leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza.
- In the context of limited laboratory resources in hurricane-affected areas, health care providers should contact their territorial or state health department if they need assistance with ordering specific diagnostic tests.
- For certain conditions, such as leptospirosis, empiric therapy should be considered pending results of diagnostic tests— treatment for leptospirosis is most effective when initiated early in the disease process. Providers can contact their territorial or state health department or CDC for consultation.
- Local health care providers are strongly encouraged to report patients for whom there is a high level of suspicion for leptospirosis, dengue, hepatitis A, typhoid, and vibriosis to their local health authorities, while awaiting laboratory confirmation.
- Confirmed cases of leptospirosis, dengue, hepatitis A, typhoid fever, and vibriosis should be immediately reported to the territorial or state health department to facilitate public health investigation and, as appropriate, mitigate the risk of local transmission. While some of these conditions are not listed as reportable conditions in all states, they are conditions of public health importance and should be reported.
For More Information
- General health information about hurricanes and other tropical storms: https://www.cdc.gov/disasters/hurricanes/index.html
- Information about Hurricane Maria: https://www.cdc.gov/disasters/hurricanes/hurricane_maria.html
- Information for Travelers:
- Travel notice for Hurricanes Irma and Maria in the Caribbean: https://wwwnc.cdc.gov/travel/notices/alert/hurricane-irma-in-the-caribbean
- Health advice for travelers to Puerto Rico: https://wwwnc.cdc.gov/travel/destinations/traveler/none/puerto-rico?s_cid=ncezid-dgmq-travel-single-001
- Health advice for travelers to the U.S. Virgin Islands: https://wwwnc.cdc.gov/travel/destinations/traveler/none/usvirgin-islands?s_cid=ncezid-dgmq-travel-leftnav-traveler
- Resources from CDC Health Information for International Travel 2018 (the Yellow Book):
- Post-travel Evaluation: https://wwwnc.cdc.gov/travel/yellowbook/2018/post-travel-evaluation/general-approach-to-the-returned-traveler
- Information about infectious diseases after a disaster: https://www.cdc.gov/disasters/disease/infectious.html
- Dengue: https://www.cdc.gov/dengue/index.html
- Hepatitis A: https://www.cdc.gov/hepatitis/HAV/index.htm
- Leptospirosis: https://www.cdc.gov/leptospirosis/
- Typhoid fever: https://www.cdc.gov/typhoid-fever/index.html
- Vibriosis: https://www.cdc.gov/vibrio/index.html
- Information about other infectious diseases of concern:
- Conjunctivitis: https://www.cdc.gov/conjunctivitis/
- Influenza: https://www.cdc.gov/flu/index.htm
- Scabies: https://www.cdc.gov/parasites/scabies/index.html
- Tetanus and wound management: https://www.cdc.gov/disasters/emergwoundhcp.html
- Tetanus in Areas Affected by a Hurricane: Guidelines for Clinicians https://emergency.cdc.gov/coca/cocanow/2017/2017sept12.asp
Disease-carrying mosquitoes may be moving into new ecological niches with greater frequency.
Friday, September 8th, 2017“…..The website, ProMED mail, has carried more than a dozen such reports since June, all involving mosquito species known to transmit human diseases.
Most reports have concerned the United States, where, for example, Aedes aegypti — the yellow fever mosquito, which also spreads Zika, dengue and chikungunya — has been turning up in counties in California and Nevada where it had never, or only rarely, been seen.
Other reports have noted mosquito species found for the first time on certain South Pacific islands, or in parts of Europe where harsh winters previously kept them at bay…..”
An adult Aedes aegypti mosquito, the species responsible for the majority of human Zika virus cases, has been found in Canada for the first time.
Friday, August 25th, 2017Neurological complications associated with Zika virus in adults in Brazil
Monday, August 21st, 2017“…..A new article published by JAMA Neurology reports on a study of hospitalized adult patients with new-onset neurologic syndromes who were evaluated for Zika virus infection.
The single-center study of 40 patients, include 29 with Guillain-Barré syndrome (GBS), seven with encephalitis, three with transverse myelitis and one with newly diagnosed chronic inflammatory demyelinating polyneuropathy.
Of those 40 patients, 35 (88 percent) had evidence of recent Zika virus infection in the serum (blood) or cerebrospinal fluid, according to the results. Of the patients who were positive for Zika virus infection, 27 had GBS, five had encephalitis, two had transverse myelitis and one had chronic inflammatory demyelinating polyneuropathy, according to the results…..”
A new antibody-based assay distinguishes Zika from similar viral infections
Wednesday, July 19th, 2017“A new test is the best-to-date in differentiating Zika virus infections from infections caused by similar viruses. The antibody-based assay, developed by researchers at UC Berkeley and Humabs BioMed, a private biotechnology company, is a simple, cost-effective way to determine if a person’s infection is from the Zika virus or another virus of the same family, such as dengue and West Nile viruses….”
“…..This study demonstrates that the antibody-based assay we developed and implemented in five countries has high specificity and sensitivity in the detection of recent and past ZIKV infections. The ZIKV nonstructural protein 1 (NS1) blockade-of-binding ELISA assay is a simple, robust, and low-cost solution for Zika surveillance programs, seroprevalence studies, and intervention trials in flavivirus-endemic areas….”
Outcomes for Completed Pregnancies in the US States, the District of Columbia, and the US Territories
Saturday, July 8th, 2017
As of June 27, 2017
Completed pregnancies with or without birth defects: 1,687
Includes aggregated data reported to the US Zika Pregnancy Registry(https://www.cdc.gov/zika/reporting/registry.html)
Liveborn infants with birth defects: 88
Includes aggregated data reported to the US Zika Pregnancy Registry(https://www.cdc.gov/zika/reporting/registry.html)
Pregnancy losses with birth defects: 8
Includes aggregated data reported to the US Zika Pregnancy Registry(https://www.cdc.gov/zika/reporting/registry.html)
Completed pregnancies with or without birth defects: 2,830
Includes aggregated data reported to the Zika pregnancy and infant registries(https://www.cdc.gov/zika/reporting/index.html)
Liveborn infants with birth defects: 122
Includes aggregated data reported to the Zika pregnancy and infant registries(https://www.cdc.gov/zika/reporting/index.html)
Pregnancy losses with birth defects: 6
Includes aggregated data reported to the Zika pregnancy and infant registries(https://www.cdc.gov/zika/reporting/index.html)
About these numbers
What these numbers show
- The number of completed pregnancies with or without birth defects include those that ended in a live birth, miscarriage, stillbirth, or termination.
- The number of liveborn infants and pregnancy losses with birth defects include those among completed pregnancies with laboratory evidence of possible Zika virus infection.
- The numbers are aggregated into two categories 1) the 50 US states and the District of Columbia, and 2) the US territories and freely associated states. At this time, CDC is not reporting individual state, tribal, territorial or jurisdictional data to protect the privacy of the women and children affected by Zika. CDC is using the standard CDC surveillance case definition for the Zika Pregnancy and Infant registries to monitor brain abnormalities, microcephaly, and other serious birth defects that have been linked to Zika virus infection during pregnancy across the United States and territories.
- The numbers may increase or decrease as new cases are added or information on existing cases is clarified.
- Birth defects reported include those that have been linked to Zika virus infection during pregnancy, including microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from damage to brain that affects nerves, muscles and bones, such as clubfoot or inflexible joints, and confirmed hearing loss.
What these new numbers do not show
- These numbers reflect the outcomes of pregnancies with any laboratory evidence of possible Zika virus infection reported to the Zika pregnancy and infant registries as of the date specified. There may be delays in reporting of pregnancy outcomes from the jurisdictions.
- Although these birth defects occurred from pregnancies of women with laboratory evidence of possible Zika virus infection, we cannot determine whether individual defects were caused by Zika virus infection or other factors.
Where do these numbers come from?
- These data reflect pregnancies reported to the Zika pregnancy and infant registries(https://www.cdc.gov/zika/reporting/index.html). Together, these registries cover the full United States including territories and freely associated states.
- These systems were established in collaboration with state, local, tribal and territorial health departments for comprehensive monitoring of pregnancy and infant outcomes of pregnancies with any laboratory evidence of possible Zika virus infection.
- The data collected through the Zika pregnancy and infant registries will be used to update recommendations for clinical care, to plan for services and support for pregnant women and families affected by Zika virus, and to improve prevention of Zika virus infection during pregnancy.
- The Zika Pregnancy and Infant Registries) are protected by an Assurance of Confidentiality(https://www.cdc.gov/od/science/integrity/confidentiality/index.htm). Under the Assurance, CDC cannot report jurisdiction-specific information without permission from the jurisdiction.
Detailed case inclusion criteria for healthcare providers
The following details the inclusion criteria for brain abnormalities and other adverse outcomes potentially related to Zika virus infection during pregnancy. All pregnancy outcomes are monitored, but reporting of adverse outcomes is limited to those meeting the criteria below.
Brain abnormalities with and without microcephaly
- Confirmed or possible congenital microcephaly#
- Intracranial calcifications
- Cerebral atrophy
- Abnormal cortical formation (e.g., polymicrogyria, lissencephaly, pachygyria, schizencephaly, gray matter heterotopia)
- Corpus callosum abnormalities
- Cerebellar abnormalities
- Porencephaly
- Hydranencephaly
- Ventriculomegaly / hydrocephaly (excluding “mild” ventriculomegaly without other brain abnormalities)
- Fetal brain disruption sequence (collapsed skull, overlapping sutures, prominent occipital bone, scalp rugae)
- Other major brain abnormalities, including intraventricular hemorrhage in utero (excluding post-natal IVH)
Neural tube defects and other early brain malformations
- Neural tube defects (NTD)
- Anencephaly / Acrania
- Encephalocele
- Spina bifida
- Holoprosencephaly / Arhinencephaly
Structural eye abnormalities
- Microphthalmia / Anophthalmia
- Coloboma
- Cataract
- Intraocular calcifications
- Chorioretinal anomalies involving the macula (e.g., chorioretinal atrophy and scarring, macular pallor, gross pigmentary mottling and retinal hemorrhage); excluding retinopathy of prematurity
- Optic nerve atrophy, pallor, and other optic nerve abnormalities
Consequences of central nervous system (CNS) dysfunction
- Congenital contractures (e.g., arthrogryposis, club foot, congenital hip dysplasia) with associated brain abnormalities
- Congenital deafness documented by postnatal testing
#Live births: measured head circumference (HC) adjusted for gestational age and sex <3rd percentile at birth, or if not measured at birth, within first 2 weeks of life; pregnancy loss: prenatal HC more than 3 standard deviations below the mean based on ultrasound or postnatal HC <3rd percentile. Birth measurements based on intergrowth21 standards which are based on measurements within 24 hours of birth, and therefore measurements within 24 hours of birth are appropriate for this assessment.
Dysphagia resulting from congenital Zika virus syndrome microcephaly can develop in infants >3 months of age and is severe.
Wednesday, June 14th, 2017Leal MC, van der Linden V, Bezerra TP, de Valois L, Borges ACG, Antunes MMC, et al. Characteristics of dysphagia in infants with microcephaly caused by congenital Zika virus infection, Brazil, 2015. Emerg Infect Dis. 2017 Aug [date cited]. https://doi.org/10.3201/eid2308.170354
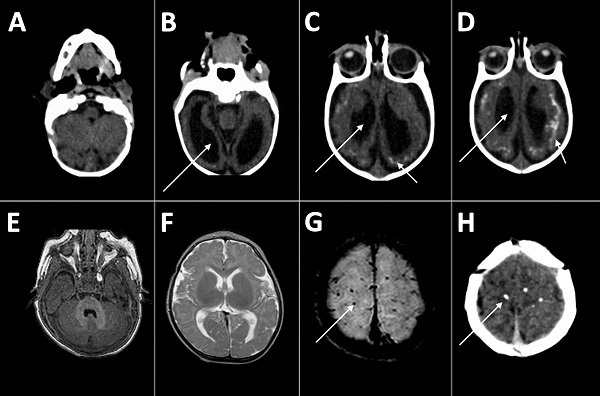
Computed tomography radiographs of the brains of 2 infants with dysphagia and microcephaly caused by congenital Zika virus infection, Brazil, 2015. A–D) Images for patient 4 show malformation of cortical development, ventriculomegaly (long arrows), and calcifications in cortical and subcortical white matter in transition between cortex and white matter (short arrows). E–H) Images for patient 6 show no malformation of cortical development or ventriculomegaly, but calcifications are visible in the cortical area (arrows).




