Archive for the ‘Acute flaccid myelitis (AFM)’ Category
CDC: Acute Flaccid Myelitis — United States, 2018
Friday, July 12th, 2019Lopez A, Lee A, Guo A, et al. Vital Signs: Surveillance for Acute Flaccid Myelitis — United States, 2018. MMWR Morb Mortal Wkly Rep. ePub: 9 July 2019. DOI: http://dx.doi.org/10.15585/mmwr.mm6827e1external icon
“…….Among all patients with confirmed, probable, and non-AFM, 227 (98%), 26 (100%), and 113 (98%), respectively, were hospitalized, including 127 (60%), 12 (57%), and 54 (50%), respectively, admitted to an intensive care unit; 27% (62) of those with confirmed AFM required respiratory support, 87% of whom (53/61) required mechanical ventilation. No deaths were reported during the acute illness of patients with confirmed AFM who had limb weakness onset in 2018; however, there were two reports of patients confirmed with AFM in 2018 who had died months after limb weakness onset.…..”

AFM: So far in 2019, there have been 11 reports of PUIs (patients under investigation), one of which has been confirmed (from North Carolina). In 2018, there are 215 confirmed cases of AFM in 40 states.
Tuesday, February 19th, 2019
An increase in reports of acute flaccid paralysis (AFP) in the United Kingdom, 1 January 2018–21 January 2019.
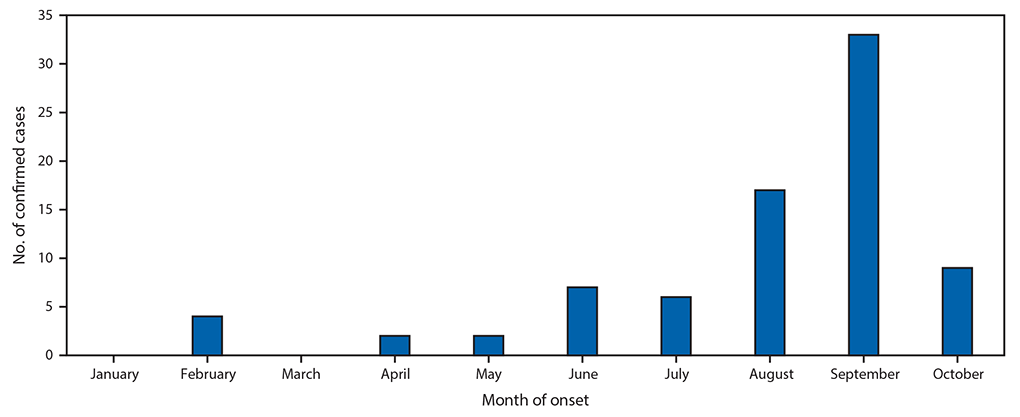
Friday, February 8th, 2019“…..As at 21 January 2019, 40 cases had been identified with a peak in October 2018. The increase was temporally associated with an upsurge in enterovirus (EV) D68 activity. Enterovirus was detected in 15 cases, mainly from respiratory tract samples; nine were typed as EV-D68……”
The U.S. AFM (Acute Flaccid Myelitis) outbreak grows to 165 cases in 36 states
Tuesday, December 18th, 2018
CDC reports 18 more cases of the mysterious AFM in the week ending on Nov 30, bringing this year’s total to 134 cases confirmed in 33 states, among 299 cases reported, and the agency says the outbreak “appears to have peaked.”
Tuesday, December 4th, 2018
Increase in Acute Flaccid Myelitis — United States, 2018
Wednesday, November 14th, 2018McKay SL, Lee AD, Lopez AS, et al. Increase in Acute Flaccid Myelitis — United States, 2018. MMWR Morb Mortal Wkly Rep. ePub: 13 November 2018. DOI: http://dx.doi.org/10.15585/mmwr.mm6745e1.
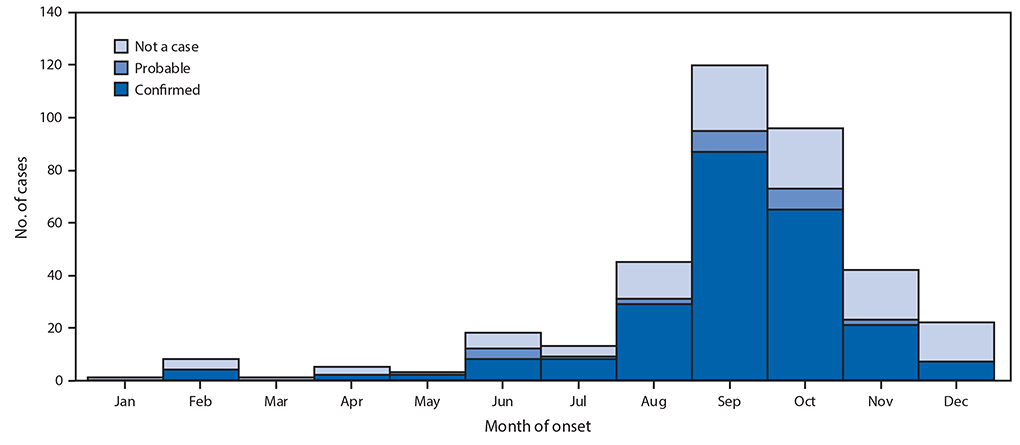
n August 2018, CDC noted an increased number of reports of patients having symptoms clinically compatible with acute flaccid myelitis (AFM), a rare condition characterized by rapid onset of flaccid weakness in one or more limbs and spinal cord gray matter lesions, compared with August 2017. Since 2014, CDC has conducted surveillance for AFM using a standardized case definition (1,2). An Epi-X* notice was issued on August 23, 2018, to increase clinician awareness and provide guidance for case reporting.
Patients who meet the clinical case criteria for AFM, defined as acute flaccid limb weakness, are classified using the Council of State and Territorial Epidemiologists case definitions of “confirmed” (magnetic resonance imaging [MRI] with spinal cord lesion largely restricted to gray matter and spanning ≥1 spinal segments), “probable” (cerebrospinal fluid [CSF] pleocytosis [>5 white blood cells per mm3]), or “not a case.”
Among 106 patients with acute flaccid limb weakness classified during January 1–November 2, 2018, 80 cases of AFM were classified as confirmed (from 25 states) (Figure), 6 as probable, and 20 as noncases. This represents a threefold increase in confirmed cases compared with the same period in 2017. Among confirmed cases, the median patient age was 4 years (range = 7 months–32 years; interquartile range [IQR] = 2.4–7.6 years), 47 (59%) were male, and, among 65 patients with information on race available, 56 (86%) were white. During the 4 weeks preceding the onset of limb weakness, signs and symptoms consistent with a viral illness were reported for 79 (99%), including fever for 65 (81%), respiratory symptoms (e.g., cough, rhinorrhea, and congestion) for 62 (78%), and gastrointestinal symptoms (e.g., vomiting and diarrhea) for 30 (38%) patients with confirmed AFM. Upper limb only involvement was reported by 38 (47.5%) patients, lower limb only by 7 (8.8%), two to three upper and lower limbs by 12 (15.0%), and all four limbs by 23 (28.8%). All patients with confirmed AFM were hospitalized, and 47 (59%) were admitted to intensive care units; no deaths have been reported.
Among 78 (98%) confirmed cases with available CSF results, 65 (83%) had pleocytosis, with a median cell count of 103 cells per mm3 (range = 6–814; IQR = 56–194); most had a lymphocyte predominance. Median CSF protein and glucose were 47 mg per dL (range = 8–289; IQR = 37–62; normal <45) and 59 mg per dL (range = 40–138; IQR = 52–65; normal ≥40), respectively. The median interval from limb weakness to CSF collection was 1 day (range = 0–16; IQR = 1–3). The median interval from sign or symptom onset to CSF collection was 7 days (range = 0–23; IQR = 5–8) for respiratory illness, 4 days (range = 0–22; IQR = 3–7) for gastrointestinal symptoms, and 3 days (range = 0–17; IQR = 2–6) for fever.
CDC conducts enterovirus/rhinovirus (EV/RV) testing for all patients meeting the clinical criteria for AFM, when specimens are available. Of the 80 confirmed cases in 2018, testing was performed on a total of 125 clinical specimens from 71 (89%) patients, including 21 CSF, 59 upper respiratory, and 45 stool/rectal swab specimens (Table). Among these, specimens from 38 (54%) patients were positive by EV/RV real-time reverse transcription–polymerase chain reaction testing, including 11 (29%) for EV-A71, 14 (37%) for EV-D68, and 13 (34%) for other viruses, primarily from nonsterile sites. CSF specimens from two patients were positive. One CSF specimen was positive for EV-A71; this patient also had a stool specimen positive for EV-A71. The second patient had a CSF specimen positive for EV-D68; this patient also had EV-D68 and parechovirus-A6 identified in a respiratory specimen. Two additional patients had more than one virus detected in a single respiratory specimen, including one with EV-D68 and echovirus 6 and one with RV-A24 and parechovirus-A6. All stool specimens tested negative for poliovirus. Among the 20 patients who did not meet the AFM case definition and were classified as noncases, 1 (5%) had a positive CSF specimen (echovirus 25), 7 (35%) had positive respiratory specimens (EV-A71, RV-A24, RV-A56, RV-A90, EV/RV not typed), and 6 (30%) had positive stool or rectal swab specimens (EV-D68, EV-A71, RV-A90, echovirus 9, echovirus 11, echovirus 25).
Because some enteroviruses can cause acute flaccid limb weakness, and there was a temporal association with AFM and a nationwide severe respiratory outbreak of EV-D68 in 2014 (2), CDC performs EV/RV testing in an effort to identify etiologies for AFM cases. Despite a subsequent peak of AFM in 2016 (https://www.cdc.gov/acute-flaccid-myelitis/afm-surveillance.html), CDC did not receive reports of large outbreaks of severe respiratory illness in 2016. Further, there has been limited detection of pathogens in CSF in these cases; virus identified in CSF would be considered etiologic. Almost all patients with AFM have reported signs and symptoms consistent with viral illness in the weeks preceding limb weakness. Clinical, laboratory, and epidemiologic evidence to date suggest a viral association. CDC and collaborators continue to investigate risk factors for AFM and to study the causes and mechanisms of AFM.
Parents and caregivers are urged to seek immediate medical care for a child who develops sudden weakness of the arms or legs. In the evaluation of a child with acute flaccid limb weakness, clinicians are advised to inquire about recent fever with or without antecedent respiratory or gastrointestinal symptoms and to collect timely specimens for viral testing, including CSF, serum, respiratory, and stool specimens. Additional information for clinicians is available at https://www.cdc.gov/acute-flaccid-myelitis/hcp/index.html. Patients with acute flaccid limb weakness should be reported to their health departments as soon as possible regardless of laboratory or MRI findings.
From August 2014 through October 2018, CDC has received information on a total of 404 confirmed cases of AFM across the US; most of the cases have occurred in children.
Tuesday, November 6th, 2018CDC: So far in 2018, there are 72 confirmed cases of AFM.
Wednesday, October 31st, 2018
At a Glance
- CDC is concerned about AFM, a serious condition that causes weakness in the arms or legs.
- From August 2014 through October 2018, CDC has received information on a total of 396 confirmed cases of AFM across the US; most of the cases have occurred in children.
- Even with an increase in cases since 2014, AFM remains a very rare condition. Less than one in a million people in the United States get AFM each year.
- While we don’t know the cause of most of the AFM cases, it’s always important to practice disease prevention steps, such as staying up-to-date on vaccines, washing your hands, and protecting yourself from mosquito bites.

