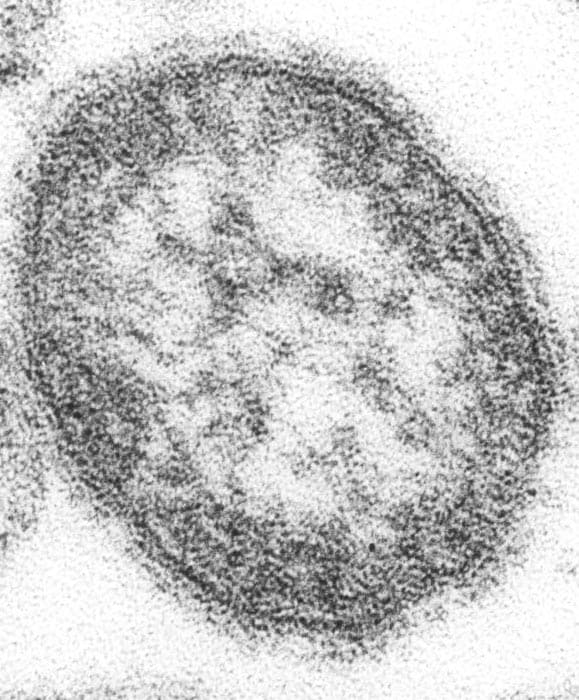
Archive for the ‘Measles’ Category
Eliminating measles globally
Friday, December 6th, 2019CDC: https://www.cdc.gov/mmwr/volumes/68/wr/mm6848a1.htm?s_cid=mm6848a1_e&deliveryName=USCDC_921-DM14806
Patel MK, Dumolard L, Nedelec Y, et al. Progress Toward Regional Measles Elimination — Worldwide, 2000–2018. MMWR Morb Mortal Wkly Rep 2019;68:1105–1111. DOI: http://dx.doi.org/10.15585/mmwr.mm6848a1external icon
What is already known about this topic?
In 2012, the World Health Assembly endorsed the Global Vaccine Action Plan; countries in all six World Health Organization regions have adopted goals to eliminate measles by 2020.
What is added by this report?
During 2000–2018, annual reported measles incidence decreased 66%, and annual estimated measles deaths decreased 73%. Since 2000, measles vaccination has prevented an estimated 23.2 million deaths globally. However, measles incidence increased in five regions during 2016–2018.
What are the implications for public health practice?
To achieve regional measles elimination goals, resource commitments are needed to strengthen routine immunization systems, close immunity gaps, and improve case-based surveillance.
National Update on Measles Cases and Outbreaks — United States, January 1–October 1, 2019.
Saturday, October 5th, 2019Patel M, Lee AD, Clemmons NS, et al. National Update on Measles Cases and Outbreaks — United States, January 1–October 1, 2019. MMWR Morb Mortal Wkly Rep. ePub: 4 October 2019. DOI: http://dx.doi.org/10.15585/mmwr.mm6840e2external icon
Summary
What is already known about this topic?
Measles was eliminated in the United States in 2000. High national coverage with measles, mumps, and rubella vaccine and rapid implementation of measles control measures prevent widespread measles transmission.
What is added by this report?
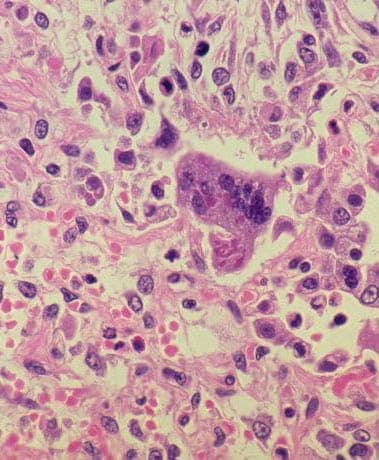
- During January–September 2019, 1,249 U.S. measles cases were reported, the highest annual number since 1992.
- Eighty-nine percent of measles patients were unvaccinated or had an unknown vaccination status, and 10% were hospitalized.
- Eighty-six percent of cases were associated with outbreaks in underimmunized, close-knit communities, including two outbreaks in New York Orthodox Jewish communities that threatened measles elimination status in the United States.
What are the implications for public health practice?
Ensuring high rates of measles immunization in all communities is critical to sustaining measles elimination.
CDC: The year’s total number of measles cases = 1,109
Tuesday, July 9th, 2019| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Measles Cases | 63 | 220 | 55 | 187 | 667 | 188 | 86 | 120 | 372 | 1109 |
“…..The states that have reported cases to CDC are Arizona, California, Colorado, Connecticut, Florida, Georgia, Idaho, Illinois, Indiana, Iowa, Kentucky, Maine, Maryland, Massachusetts, Michigan, Missouri, New Mexico, Nevada, New Hampshire, New Jersey, New York, Oklahoma, Oregon, Pennsylvania, Texas, Tennessee, Virginia, and Washington.…”
Unlike two dozen other states this year, not a single person in Mississippi has been infected with measles
Tuesday, July 2nd, 2019“…….Mississippi adopted its first compulsory vaccination law in 1900, adding a religious exemption in 1960. Almost 20 years later, in 1979, the religious exemption was challenged in court, with the plaintiff arguing that the state must expand the exemption to include any religion, not just religions officially recognized by the state. In response, the Mississippi Supreme Court struck down religious exemptions altogether, ruling that non-medical vaccine exemptions violate people’s constitutional right to equal protection under the law.
The decision was a big win for public health, but it certainly has not stopped attempts to water down Mississippi’s vaccine rules…..”

From January 1 to June 20, 2019, 1,077 individual cases of measles have been confirmed in 28 states.
Tuesday, June 25th, 2019DRC: In the first five months of 2019, more than 1,500 measles-related deaths were officially recorded
Wednesday, June 12th, 2019“……Alongside a tough battle against Ebola, the Democratic Republic of the Congo (DRC) health ministry yesterday declared a measles outbreak, spanning 23 of the country’s 26 provinces and piling up 87,000 suspected cases since the first of the year.…”



Measles in America: 1,001 cases so far
Friday, June 7th, 2019“……In response to the current situation, CDC has:
- Implemented an Incident Management Structure (IMS) within the National Center for Immunization and Respiratory Diseases to respond to the measles outbreaks.
- Reinforced to healthcare providers the guidelines for recognition and prevention of measles.
- Developed a toolkit with resources for physicians about measles and vaccines and has begun implementing a strategy to address vaccine hesitancy, including creating new resources and updating existing ones to counter misinformation.
- Undertaken outreach to rabbinical, camp, and medical associations to help spread clear, consistent, and credible vaccine information through trusted sources.
- Deployed a field team to Rockland County, NY, to provide technical assistance with case identification and contact tracing.
- Continued to work with local communities to figure out how to develop culturally appropriate communications resources for affected areas in New York.
- Since January 1, 2019, conducted 73 air contact investigations for measles and identified over 1,500 individuals who were exposed to the measles virus during travel.
- Deployed an immunization program project officer to Albany……”
From January 1 to May 24, 2019, 940 individual cases of measles have been confirmed in 26 states.
Wednesday, May 29th, 2019| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Measles Cases | 63 | 220 | 55 | 187 | 667 | 188 | 86 | 120 | 372 | 940 |
Since January, the Philippines has had one of the worst measles outbreaks in the world: more than 33,000 cases and 466 deaths from the vaccine-preventable disease.
Saturday, May 25th, 2019Measles in the Americas
Tuesday, May 21st, 2019PAHO
- In 2019 to date, 12 countries in the Region have reported confirmed measles cases: Argentina, the Bahamas, Brazil, Canada, Chile, Colombia, Costa Rica, Mexico, Peru, the United States of America, Uruguay, and the Bolivarian Republic of Venezuela.
- No fatal cases have been reported in 2019 in the Region. There was one additional confirmed measles case reported in the Region onboard a cruise ship that sailed between Aruba and Curacao.
- Since the prior PAHO/WHO Epidemiological Update on Measles published on 18 April 20191, 9 countries have reported additional cases of measles: Brazil (70 cases), Canada (12 cases), Chile (1 case), Colombia (27 cases), Costa Rica (1 case), Peru (1 case), the United States of America (284 cases), Uruguay (6 cases), and the Bolivarian Republic of Venezuela (63 cases).