Archive for the ‘Documents’ Category
The legal determinants of health: harnessing the power of law for global health and sustainable development
Saturday, October 31st, 2020-
Published:April 30, 2019DOI:https://doi.org/10.1016/S0140-6736(19)30233-8
“……Key messages
- 1
Law affects global health in multiple ways, by structuring, perpetuating, and mediating the social determinants of health.
- 2
Although law has been central to major public health achievements in the past, its capacity to advance global health with justice remains substantially underutilised, particularly among professionals in the fields of health and science.
- 3
The right to health, a legally binding norm, provides a foundation for advancing global health with justice and should underpin health-related legal reforms.
- 4
Every human being has a right to affordable, high quality health services. By embedding equity and accountability in all health systems, the law and the rule of law can achieve health coverage that is truly universal—delivering the Sustainable Development Goals’ promise to leave no one behind.
- 5
Although the ability to enforce compliance with international legal obligations is generally limited, and largely dependent on power dynamics and political will, creative mechanisms can foster compliance and help establish impetus for action.
- 6
Law can address the pressing health concerns of the 21st century, across diverse areas. From tobacco control, non-communicable diseases, and road safety, to health emergencies, law can implement fair, evidence-based interventions to save lives. The global health community should champion evidence-based legal interventions and build the research case for legal action.
- 7
Laws that stigmatise or discriminate against marginalised populations are especially harmful and exacerbate health disparities. The global health community must oppose laws that undermine the right to health and to equity.
- 8
To realise the full potential of law to advance global health with justice, the global health community should build legal capacity and establish a sustained dialogue with legislators, regulators, judges, civil society, and researchers……”
Interim case reporting form for 2019 Novel Coronavirus (2019-nCoV) of confirmed and probable cases
Monday, January 27th, 2020
CDC: Wuhan, China
Cervical cancer worldwide
Friday, December 6th, 2019- There were 570,000 cases and 311,000 deaths worldwide last in 2018.
- The average age of diagnosis was 53.
- In 42 low-resource countries, it was the most common cancer in women.
- A third of the cervical cancer burden fell on China and India together.
Global Humanitarian Overview 2020
Thursday, December 5th, 2019Recent trends and challenges
In 2019, many more people needed humanitarian assistance than we had forecast, largely because of conflicts and extreme climate events. Donors provided a record $16 billion for inter-agency appeals between January and November 2019.
Compliance with international law is declining. Armed conflicts are killing and maiming a record number of children, forcing them to flee their homes. They are becoming a lost generation. Women and girls are at higher risk of sexual and gender-based violence. One in five people living in conflict areas has a mental health condition.
Highly violent conflicts are causing widespread hunger, displacement, death and destruction around the world. They are taking a heavy toll on civilians, who account for 90 per cent of the casualties when explosive weapons are used in populated areas.
There were 791 attacks against health workers and health-care facilities in the first nine months of 2019, resulting in 171 deaths. In 2018, 131 aid workers were killed and 130 were kidnapped in 400 attacks. Attacks against health and aid workers are putting millions of people at risk by denying them care and aid.
Emerging trends and risks
Climate change is increasing people’s vulnerability to humanitarian crises. The world’s eight worst food crises are all linked to both conflict and climate shocks.
Infectious diseases are becoming more prevalent and harder to control, because of conflict, weak health systems, poor water and sanitation, and lack of access to vaccinations.
In 2019, 33 low-income countries were in, or at risk of, debt distress. Of these, 12 countries with humanitarian appeals are home to 40 per cent of the people in need of humanitarian assistance. A global economic slowdown could further increase vulnerability in countries already experiencing economic stress and debt problems.
Humanitarian needs and requirements
In 2020, nearly 168 million people will need humanitarian assistance and protection. This represents one in about 45 people in the world, and is the highest figure in decades. The United Nations and partner organizations aim to assist nearly 109 million of the most vulnerable people. This will require funding of $28.8 billion.
The situation will keep getting worse unless climate change and the root causes of conflict are better addressed. On current trends, projections show that more than 200 million people could be in need of assistance by 2022.
The humanitarian system is more effective better prioritized, more innovative and more inclusive than ever. In the first nine months of 2019, humanitarian organizations reached 64 per cent of people targeted to receive aid through Humanitarian Response Plans (HRPs).
Globally, at the start of 2019 some 821 million people were undernourished, including 113 million who suffered from acute hunger. Conflict is the key driver of hunger. By the beginning of 2019, armed conflicts and persecution had driven a record number of nearly 71 million people from their homes.
Regional and country overview
Yemen is the world’s worst humanitarian crisis, and the number of people in need is expected to remain close to 2019 levels of 24 million, almost 80 per cent of the population. The humanitarian response in Yemen is also the world’s largest, despite huge challenges.
The conflict in Syria continues to drive the world’s largest refugee crisis, with 5.6 million refugees in the region. In addition, more than 6 million Syrians are internally displaced.
Humanitarian needs will also remain exceptionally high in the Democratic Republic of the Congo, Somalia and South Sudan.
In Sudan, a deepening economic crisis has significantly increased food insecurity and weakened essential services, including health, water and education. The new civilian authorities need more international support.
In the Sahel, displacement has dramatically increased, and hunger has reached critical levels. In the Lake Chad Basin, the humanitarian crisis shows no signs of abating as it enters its seventh year.
The needs have also grown significantly in several other countries, including Afghanistan, where almost one quarter of the population is likely to need humanitarian assistance following years of violent conflict, as well as severe drought.
In Venezuela, a deepening economic crisis has led to a severe reduction in the income of many households and a sharp deterioration in water, power and health services, prompting many to leave.
A deepening political and socioeconomic crisis has also significantly increased needs in Haiti, with 4.2 million people expected to be food insecure by March 2020.
More people-centred humanitarian action We are getting better at addressing the needs of women and girls, and people with disabilities. We are strengthening efforts to combat sexual and gender-based violence.
We are working better together to deliver cash, which can often meet more needs, more efficiently.
We are also strengthening collaboration between humanitarian and development organizations.
Innovative humanitarian financing
Humanitarian organizations have a better understanding of what is needed most urgently, and by whom. In 2019, anticipatory finance enabled early action in several crises, and risk insurance provided speedy payouts to support rapid response.
The value of timely and strategic pooled funds was again clearly demonstrated. As of mid-November 2019, the Central Emergency Response Fund (CERF) had allocated more than $494 million to support urgent needs in 47 countries and territories, while Country-Based Pooled Funds (CBPFs) had allocated $701 million in 18 countries.
A U.S. SECRET SERVICE ANALYSIS OF TARGETED SCHOOL VIOLENCE
Thursday, November 21st, 2019“……Some of the key findings from this study, and their implications for informing school violence prevention efforts, include:
• There is no profile of a student attacker, nor is there a profile for the type of school that has been targeted: Attackers varied in age, gender, race, grade level, academic performance, and social characteristics. Similarly, there was no identified profile of the type of school impacted by targeted violence, as schools varied in size, location, and student-teacher ratios. Rather than focusing on a set of traits or characteristics, a threat assessment process should focus on gathering relevant information about a student’s behaviors, situational factors, and circumstances to assess the risk of violence or other harmful outcomes.
• Attackers usually had multiple motives, the most common involving a grievance with classmates: In addition to grievances with classmates, attackers were also motivated by grievances involving school staff, romantic relationships, or other personal issues. Other motives included a desire to kill, suicide, and seeking fame or notoriety. Discovering a student’s motive for engaging in concerning behavior is critical to assessing the student’s risk of engaging in violence and identifying appropriate interventions to change behavior and manage risk.
• Most attackers used firearms, and firearms were most often acquired from the home: Many of the attackers were able to access firearms from the home of their parents or another close relative. While many of the firearms were unsecured, in several cases the attackers were able to gain access to firearms that were secured in a locked gun safe or case. It should be further noted, however, that some attackers used knives instead of firearms to perpetrate their attacks. Therefore, a threat assessment should explore if a student has access to any weapons, with a particular focus on weapons access at home. Schools, parents, and law enforcement must work together rapidly to restrict access to weapons in those cases when students pose a risk of harm to themselves or others.
• Most attackers had experienced psychological, behavioral, or developmental symptoms: The observable mental health symptoms displayed by attackers prior to their attacks were divided into three main categories: psychological (e.g., depressive symptoms or suicidal ideation), behavioral (e.g., defiance/misconduct or symptoms of ADHD/ADD), and neurological/developmental (e.g., developmental delays or cognitive deficits). The fact that half of the attackers had received one or more mental health services prior to their attack indicates that mental health evaluations and treatments should be considered a component of a multidisciplinary threat assessment, but not a replacement. Mental health professionals should be included in a collaborative threat assessment process that also involves teachers, administrators, and law enforcement.
• Half of the attackers had interests in violent topics: Violent interests, without an appropriate explanation, are concerning, which means schools should not hesitate to initiate further information gathering, assessment, and management of the student’s behavior. For example, a student who is preoccupied or fixated on topics like the Columbine shooting or Hitler, as was noted in the backgrounds of several of the attackers in this study, may be the focus of a school threat assessment to determine how such an interest originated and if the interest is negatively impacting the student’s thinking and behavior.
• All attackers experienced social stressors involving their relationships with peers and/or romantic partners: Attackers experienced stressors in various areas of their lives, with nearly all experiencing at least one in the six months prior to their attack, and half within two days of the attack. In addition to social stressors, other stressors experienced by many of the attackers were related to families and conflicts in the home, academic or disciplinary actions, or other personal issues. All school personnel should be trained to recognize signs of a student in crisis. Additional training should focus on crisis intervention, teaching students skills to manage emotions and resolve conflicts, and suicide prevention.
• Nearly every attacker experienced negative home life factors: The negative home life factors experienced by the attackers included parental divorce or separation, drug use or criminal charges among family members, or domestic abuse. While none of the factors included here should be viewed as predictors that a student will be violent, past research has identified an association between many of these types of factors and a range of negative outcomes for children.
• Most attackers were victims of bullying, which was often observed by others: Most of the attackers were bullied by their classmates, and for over half of the attackers the bullying appeared to be of a persistent pattern which lasted for weeks, months, or years. It is critical that schools implement comprehensive programs designed to promote safe and positive school climates, where students feel empowered to report bullying when they witness it or are victims of it, and where school officials and other authorities act to intervene.
• Most attackers had a history of school disciplinary actions, and many had prior contact with law enforcement: Most attackers had a history of receiving school disciplinary actions resulting from a broad range of inappropriate behavior. The most serious of those actions included the attacker being suspended, expelled, or having law enforcement interactions as a result of their behavior at school. An important point for school staff to consider is that punitive measures are not preventative. If a student elicits concern or poses a risk of harm to self or others, removing the student from the school may not always be the safest option. To help in making the determination regarding appropriate discipline, schools should employ disciplinary practices that ensure fairness, transparency with the student and family, and appropriate follow-up.
• All attackers exhibited concerning behaviors. Most elicited concern from others, and most communicated their intent to attack: The behaviors that elicited concern ranged from a constellation of lower-level concerns to objectively concerning or prohibited behaviors. Most of the attackers communicated a prior threat to their target or communicated their intentions to carry out an attack. In many cases, someone observed a threatening communication or behavior but did not act, either out of fear, not believing the attacker, misjudging the immediacy or location, or believing they had dissuaded the attacker. Students, school personnel, and family members should be encouraged to report troubling or concerning behaviors to ensure that those in positions of authority can intervene.….”
“According to a new U.S. Army report, Americans could face a horrifically grim future from climate change involving blackouts, disease, thirst, starvation and war. The study found that the US military itself might also collapse. This could all happen over the next two decades…..”
Thursday, October 31st, 2019“…….The report, titled Implications of Climate Change for the U.S. Army, was launched by the U.S. Army War College in partnership with NASA in May at the Wilson Center in Washington DC. The report was commissioned by Gen. Milley during his previous role as the Army’s Chief of Staff……..


The two most prominent scenarios in the report focus on the risk of a collapse of the power grid within “the next 20 years,” and the danger of disease epidemics. Both could be triggered by climate change in the near-term………
The report also warns that the US military should prepare for new foreign interventions in Syria-style conflicts, triggered due to climate-related impacts. Bangladesh in particular is highlighted as the most vulnerable country to climate collapse in the world…..
“The permanent displacement of a large portion of the population of Bangladesh would be a regional catastrophe with the potential to increase global instability,” the report warns. “This is a potential result of climate change complications in just one country. Globally, over 600 million people live at sea level.”
Sea level rise, which could go higher than 2 meters by 2100 according to one recent study, “will displace tens (if not hundreds) of millions of people, creating massive, enduring instability,” the report adds……..“


Children, Food, and Nutrition: UNICEF
Saturday, October 19th, 2019UNICEF: Document
“High rates of childhood obesity are a problem in a rising number of low- and middle-income countries, according to a new global assessment of child malnutrition by UNICEF. It’s the agency’s most comprehensive nutrition report in two decades.
The report paints a complex, dire picture of the state of children’s health. Overall, it found that around 200 million children under age 5, or 1 in 3 worldwide, are either undernourished or overweight. Wasting (below-average weight for height) and micronutrient deficiency remain persistent challenges in Africa and South Asia. Still, there’s some good news: Stunting (below-average height for age) has dropped sharply in the last two decades on every continent except Africa.
Meanwhile, at least 340 million adolescents worldwide between ages 5-19, and 40 million children under age 5, have been classified as overweight, the report found. The most profound increase has been in the 5-19 age group, where the global rate of overweight increased from 10.3% in 2000 to 18.4% in 2018…..”
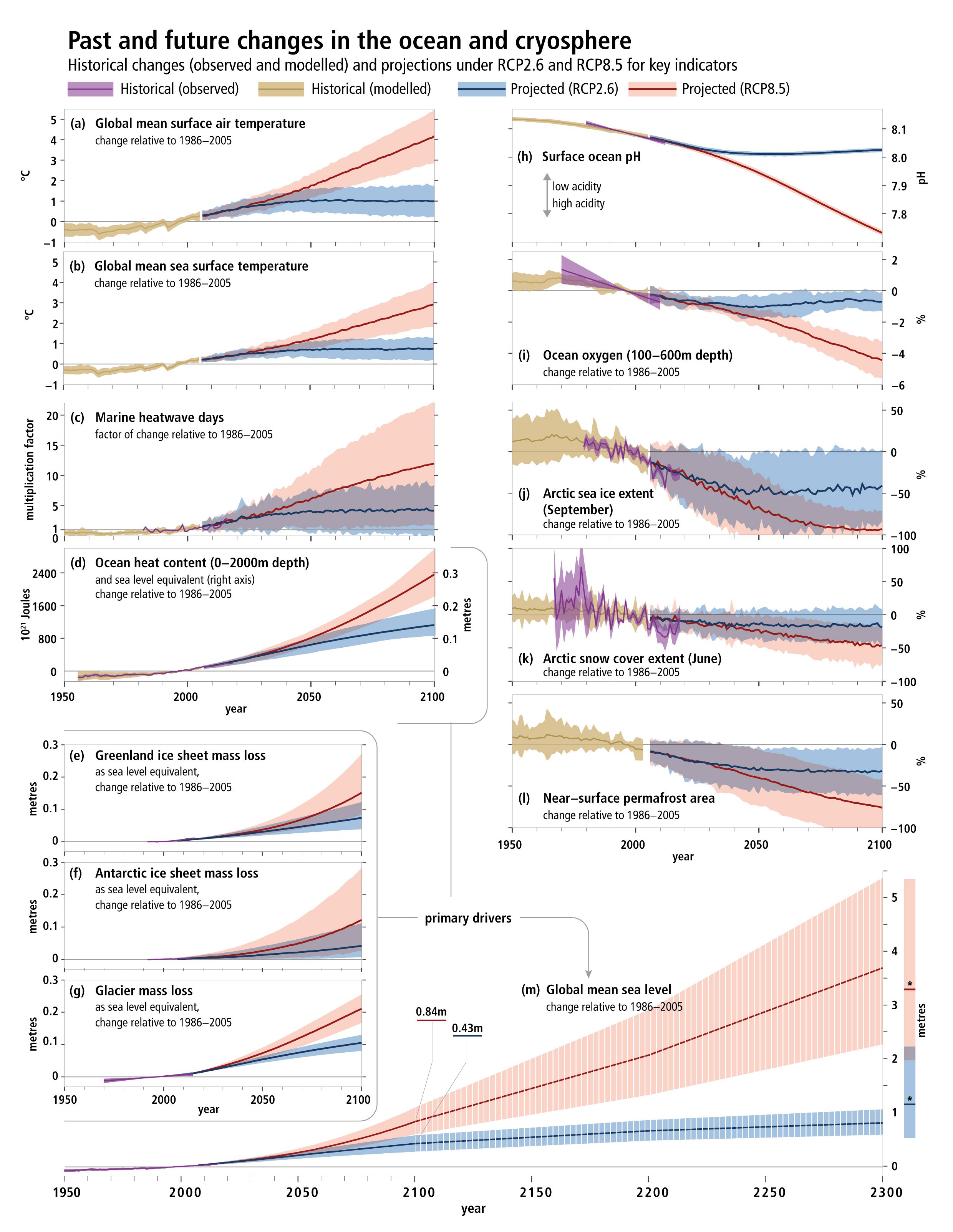
Special Report on the Ocean and Cryosphere in a Changing Climate
Wednesday, September 25th, 2019NYT: “……Earth’s oceans are under severe strain from climate change, a major new United Nations report warns, threatening everything from the ability to harvest seafood to the well-being of hundreds of millions of people living along the coasts.
Rising temperatures are contributing to a drop in fish populations in many regions, and oxygen levels in the ocean are declining while acidity levels are on the rise, posing risks to important marine ecosystems, according to the report issued Wednesday by the Intergovernmental Panel on Climate Change, a group of scientists convened by the United Nations to guide world leaders in policymaking.
In addition, warmer ocean waters, when combined with rising sea levels, threaten to fuel ever more powerful tropical cyclones and floods, the report said, further imperiling coastal regions and worsening a phenomenon that is already contributing to storms like Hurricane Harvey, which devastated Houston two years ago……”
Nourishing Lives and Building the Future: the History of Nutrition at USAID
Wednesday, August 14th, 2019Nourishing Lives and Building the Future: the History of Nutrition at USAID
For more than 50 years, USAID has worked to address the devastating effects of malnutrition, continually learning and adapting our response to ever-evolving nutrition needs and understanding. This resource describes the Agency’s investments and contributions to global progress to improve nutrition, achieved through close collaboration with implementing partners, host countries, civil society, the private sector, researchers, and other key stakeholders.
Chapter 1: Introduction and Overview
USAID’s nutrition programming was established in the 1960s, and the U.S government was providing food assistance even earlier through Title II, or the Food for Peace Act, which built the foundation for nutrition at USAID. In addition to detailing the origins of nutrition at USAID, this chapter also outlines the evolution of USAID’s nutrition programming and investments over time.
Chapter 2: Improving Nutrition for Women and Young Children
Improving the dietary practices and nutritional status of women and children has always been at the core of USAID’s nutrition and health programs. This chapter presents the history of USAID’s advancements to cross-cutting approaches for improving the delivery of nutrition services and enhance maternal, infant and young child nutrition, including the Agency’s community-based focus and its innovations in social and behavior change.
Chapter 3: From Vitamin A to Zinc: Addressing Micronutrient Malnutrition
Micronutrients are essential for good nutrition, proper growth and development, and overall health. As this chapter details, USAID has worked for decades to ensure individuals in need receive the nutrients they lack– particularly vitamin A, iron, iodine, and zinc which have a direct impact on maternal and child survival.
Chapter 4: Combating the HIV Epidemic through Food and Nutrition
Poor nutrition magnifies HIV infection for affected individuals, including increasing the risk of infection, hospitalization, and mortality. Since the early 2000s, USAID has supported critical research on nutrition and HIV, developed country guidance and training materials, strengthened health systems, and provided HIV-affected families with food commodities and nutrition support to meet the nutritional needs of individuals living with HIV.
Chapter 5: Multi-sectoral Nutrition and Food Security
In the early 1970s, USAID and other global actors recognized the need for a multi-sectoral approach to reducing malnutrition— working across sectors to address the many causes and consequences of inadequate nutrition. Working closely with partners, USAID has played a key role in identifying the causes of malnutrition, addressing them through a multi-sectoral lens, and exploring how to improve nutrition through agriculture and food security efforts.
Chapter 6: Research and Measurement for Understanding and Reducing Malnutrition
Findings from nutrition research are critical to advancing the work of country governments, foundations, international organizations, partners, and the entire nutrition community. For decades, USAID has supported cutting-edge research, translated key findings into practice, and invested to improve how nutritional status is measured, examples of which are described throughout this chapter.
Spotlight: Capacity Building and Knowledge Management
Long-term support for the development of country-level human and institutional capacity is a vital component of sustaining the results of USAID’s investments beyond the end of external assistance. Capacity building and knowledge management are therefore important elements of our nutrition investments, and this spotlight section offers examples of the Agency’s support.
Chapter 7: Adapting to a Changing World
Nutrition programming will need to seek creative new ways to improve food systems, food quality, nutrition behaviors, and social norms around eating, in addition to continuing to implement and scale up established approaches to improve nutrition. To achieve this, USAID will seek out strategic and innovative ways to support partner countries in becoming more self-reliant and capable of leading their own development journeys.
Rabies: Zero by 30
Saturday, August 10th, 2019Overview

Why eliminate rabies?
An estimated 59 000 people die from rabies each year. That’s one person every nine minutes of every day, 40% of whom are children living in Asia and Africa. As dog bites cause almost all human cases, we can prevent rabies deaths by increasing awareness, vaccinating dogs to prevent the disease at its source and administering life-saving treatment after people have been bitten. We have the vaccines, medicines, tools and technologies to prevent people from dying from dog-mediated rabies. For a relatively low cost it is possible to break the disease cycle and save lives.
A country’s health system benefits from the capacity-building required for rabies surveillance. This core activity strengthens the health system by improving the mechanisms for surveillance of other disease and expanding access to health care. Minimizing duplication and improving efficiencies by pooling resources and developing strong health service networks saves money and makes the most of resources. Countries can maximize the impact of each dollar invested.
Investing in rabies elimination saves lives and strengthens both human and veterinary health systems. A collaborative response, through rabies programmes, contributes to disease prevention and preparedness. This means integrated rabies elimination is a model for One Health collaboration.
In the past, the global response has been fragmented and uncoordinated. We need to break the status quo and come together with a combined will, an achievable goal and a common plan. That combined will was evident in 2015, and the resulting global call to action made it clear that now is the time to act.
A call for action
In 2015, the world called for action by setting a goal of zero human dog-mediated rabies deaths by 2030, worldwide. Now, for the first time, four organizations – the World Health Organizaton (WHO), the World Organisation for Animal Health (OIE), the Food and Agriculture Organization of the United Nations (FAO) and the Global Alliance for Rabies Control (GARC) – have joined forces, as the United Against Rabies collaboration, and are determined to reach this goal.
The United Against Rabies collaboration leverages existing tools and expertise in a coordinated way to empower, engage and enable countries to save human lives from this preventable disease. The global strategic plan puts countries at the centre with renewed international support to act.This country-centric engagement will be flexible and consider different contexts and capacities. Countries will lead efforts, driving the changes needed to reach Zero by 30, empowered by the United Against Rabies collaboration, as they build sustainable institutional capacity and end human deaths from dog-mediated rabies.