Archive for the ‘Animals/Pets’ Category
CDC: Pet Safety in Emergencies
Wednesday, October 23rd, 2019- bringfido.comexternal icon or call 877-411-FIDO
- dogfriendly.comexternal icon or call 888-281-5170
- doginmysuitcase.comexternal icon or call 8880254-0637
- pet-friendly-hotels.netexternal icon or call 866-966-3046
- pets-allowed-hotels.comexternal icon or call 800-250-1625
- petswelcome.comexternal icon
- tripswithpets.comexternal icon
To get started, familiarize yourself with the types of disasters that could affect your area and consider your options for providing care for your pet(s).
Disasters can happen without warning, so be prepared:
- Make sure your pet(s) wear collars and tags with up-to-date contact information and other identification.
- Microchip your pet(s) – this is one of the best ways to ensure that you and your pet are reunited if you are separated. Always be sure to register the microchip with the manufacturer and keep your contact information up to date with the microchip company.
- Keep a leash and/or carrier near the exit.
- Make sure you have proper equipment for pets to ride in the car (carriers, harnesses, pet seatbelts).
- Prepare a Pet Disaster Kitso evacuation will go smoothly for your entire family. Ask your veterinarian for help in putting together your pet’s veterinary records.
Make a Plan
- Plan where you and your pet will stay in case you need to evacuate your home. Pets may not be allowed in local shelters, unless they are service animals. Many disaster evacuation centers (such as Red Cross evacuation centers) do not accept pets and other animals.
- Identify shelters or out-of-town friends or relatives where your pets and other animals can stay.
- Locate boarding facilities or animal hospitals near your evacuation shelter and in the case you are unable to return home right away.
- Create a buddy system in case you’re not home during an emergency. Ask a trusted neighbor who can check on your animals and can evacuate your animals if necessary.
- Locate a veterinarian or animal hospital in the area where you may be seeking temporary shelter and add the veterinarian’s contact information to your emergency kit.
Create an emergency kit for your pet
Prepare an emergency kit for your pet ahead of time.
- Purchase a pet carrier for each of your pets (write your pet’s name, your name, and contact information on each carrier).
- Food and water for at least 2 weeks for each pet
- For cats: litter box and litter
- For dogs: plastic bags for poop
- Medications for at least 2 weeks
- Medical records, including record of vaccination for rabies and other diseases, prescription medications, and medical history.
- Sturdy leashes or harnesses
- Microchip number
- Contact information (cell phone, work phone, home phone) of owner and close relative or friends
Practice evacuating your pet
- Train your pets to be in their carriers by making it a comfortable place.
- Practice transporting your pet by taking them for rides in a vehicle similar to one you would be evacuating in. If you do not have a car, make arrangements with neighbors, family, and friends. You can also contact your local government to learn about transportation options during a disaster.
- Know where your pet might hide when stressed or scared. Practice catching your pet, if needed.
- For cats, you can practice removing your cat from his/her hiding spot and using your cat’s carrier, a pillowcase, a sturdy box — anything to get your cat quickly out of harm’s way.
- Have your entire family practice evacuating with your pets so everyone knows what to take, where to find the pets, and where to meet.
If you don’t have a plan and need information quickly in an emergency, contact:
Local Animal Shelters
Search for local shelters and rescue groups on Petfinder’s Shelter Centerexternal icon. Local animal shelters may be able to offer advice on what to do with your pets if you are asked to evacuate your home.
Local Government
Local government animal control or service agencies can provide guidance on how to protect your pets in an emergency.
Relief Organizations
RedRover shelters and cares for animals displaced by natural disasters and other crises in the United States and Canada. If you need sheltering assistance, please call RedRover at (800) 440-3277 or visit RedRover.orgexternal icon.
Sheltering during an evacuation
- Remember, during a disaster, what is good for you is good for your pet. If you leave your pets behind, they may be lost, injured – or worse. Never leave a pet chained outdoors.
- Contact your local emergency management office and ask if they offer accommodations for owners and their pets. If accommodations are needed for your pet(s):
- Contact local veterinary clinics, boarding facilities, local animal shelters, family or friends outside the evacuation area, or a pet-friendly hotel, particularly along evacuation routes.
- Visit the Humane Society websiteexternal iconexternal iconto find a shelter in your area.
- Remember to take your pet’s emergency kit with you.
- Learn what to expect if you take your pet to an evacuation center.
Sheltering in place
When sheltering at home with your pet, make sure the room chosen is pet-friendly in the following ways:
- Select a safe room, preferably an interior room with no (or few) windows.
- Remove any toxic chemicals or plants.
- Close off small areas where frightened cats could get stuck in (such as vents or beneath heavy furniture).
Diseases that can spread between pets and people during a natural disaster
Natural disasters can contribute to the transmission of some diseases. Exposure to inclement weather conditions, stagnant water, wildlife or unfamiliar animals, and overcrowding can put your pet at risk for getting sick. Some of these illnesses can be transmitted between pets and people (also known as zoonotic diseases or zoonoses). Some common disaster-related diseases that pets can pass to people are the following: rabies, leptospirosis, and diseases spread by mosquitoes, fleas, and ticks.
- Rabies is a virus that affects the nervous system in both animals and people. Rabies is transmitted through bites from rabid animals or through contact with their saliva. To protect you and your pet: Report any bite wounds to medical personnel immediately. Practice safe handling of pets in a stressful situation. Keep your pet in a carrier or on a leash. Do not allow your pet to interact with other animals
- Leptospirosis is a bacterial disease found in the urine of infected animals that can cause kidney damage and affect other organs. It is transmitted through contact with infected urine or contaminated water, soil, and food. Wash your hands after coming in contact with urine. Avoid stagnant water, especially after flooding occurring after natural disasters. Don’t allow pets to play in or drink contaminated water.
- Diseases spread by mosquitoes, fleas, and ticks: Mosquitoes, fleas, and ticks are common pests of stray animals and can be a problem immediately following a disaster situation. Their bites irritate the skin and may also spread a variety of diseases (Lyme disease, West Nile virus) harmful to both people and animals. To help prevent illnesses associated with mosquitoes, fleas, and ticks: Keep your pet away from wildlife and stray animals. Talk to your veterinarian about the use of a regular preventative treatment for fleas, ticks, and parasites for your pet.

How to Keep Yourself and Your Pets Healthy During a Disaster
- Wash your hands after handling your pet, its food, or its waste.
- Do not let your pet lick your face or hands.
- Keep your pet up-to-date on all vaccinations and heartworm, flea, and tick preventatives.
- Practice safe handling of your pet, because your pet may behave differently during a stressful situation.
- Keep your pet in a carrier or on a leash.
- Do not allow your pet to interact with other animals, especially wildlife and stray animals.
- Report any bite wounds to medical personnel immediately.
- Properly clean and disinfect cages and litterboxes. Wash your pet’s bedding regularly.
- Avoid stagnant water, especially after flooding occurring after natural disasters.
- Don’t allow pets to play in or drink contaminated water.
After an emergency, familiar scents and landmarks may have changed. Pets can become confused and lost, so it’s important to keep pets on leash or in a carrier when they’re being transported or when you go outside. Some hazards to be aware of for pets and people include snakes and other wildlife, especially after flooding, and downed power lines.
Returning home
- Check your home for sharp objects, spilled chemicals, and exposed wiring to protect your family and your pets from injury.
- The behavior of animals may change dramatically after a flood, flash flood, thunderstorm, or hurricane. Normally quiet and friendly animals may become irritable.
- Monitor animals closely and only release them in a safe and secure environment.
- Contact a veterinarian if you notice any signs of stress, discomfort, or illness in your pets.
Finding a lost pet
- Make sure that your family is in a safe location before you begin your search.
- If you are in a shelter that houses pets, inform one of the pet caretakers. Give the pet caretaker a missing pet flyer.
- Many shelters and organizations will house pets lost during disasters. Contact your local humane society, animal welfare organization, or county or state animal response team to find the shelters or organizations near you. . The National Animal Rescue and Sheltering Coalitionexternal icon may also be able to help find the right local response organization.
- In addition to shelters and rescue organizations, you can contact local animal control about your lost pet and post missing pet flyers in the area once conditions are safe.
- If your pet has a microchip, call the microchip company to let them know your pet is missing and make sure all the information about your pet including your current contact information is updated and current.
Pet first aid
- Emergency treatment and first aid for pets should never be used as a substitute for veterinary care. But, it may save your pet’s life before you can get your pet to a veterinarian.
- The American Veterinary Medical Associationexternal icon offers specific advice for basic first aid in the case of poisoning, seizures, fractures, external and internal bleeding, burns, choking, heatstroke, and what to do if your pet has no heartbeat or is not breathing.

Tips for handling injured pets
- Never assume that even the gentlest pet will not bite or scratch if injured.
- Pain and fear can make animals unpredictable or even dangerous.
- Don’t attempt to hug an injured pet, and always keep your face away from its mouth, which might scare the animal more or cause them pain.
- Perform any contact with your pet slowly and gently.
- Stop if your animal becomes more agitated or stressed.
- Try to get your pet to a veterinarian as quickly as possible without risking injury or illness to yourself or your family.
- CDC
- Pets in Evacuation Centers
- Pet Project: 5 Ways to Prep Your Pet for Emergencies
- Keep your pets safe in an emergency: 5 things to know
- Pet Disaster Preparedness Kit
- Pet Boarding Instructions pdf icon[PDF – 2 pages]
- Missing Pet Flyer Template word icon[Doc – 1 page]
- Interim Guidelines for Animal Health and Control of Disease Transmission in Pet Shelters
- Ready Wrigley
- American Veterinary Medical Association (AVMA)
AMVA offers a variety of resources to assist veterinarians, animal owners, and others interested in the well-being of animals to prepare for animal safety in the event of a disaster. Visit AVMA’s Disaster Preparedness Siteexternal icon - RedRover
Through its volunteer-driven RedRover Responders (formerly the Emergency Animal Rescue Service or EARS), RedRover shelters and cares for animals displaced by natural disasters and other crises in the United States and Canada. If you need sheltering assistance, please call RedRover at (800) 440-3277. Visit redrover.orgexternal icon. - Federal Emergency Management Agency (FEMA)
FEMA is the federal agency that leads the effort to prepare the nation for all hazards and effectively manage federal response and recovery efforts following any national incident. Visit ready gov: Caring for Animalsexternal icon - Humane Society of the United States: Making a disaster plan for petsexternal icon
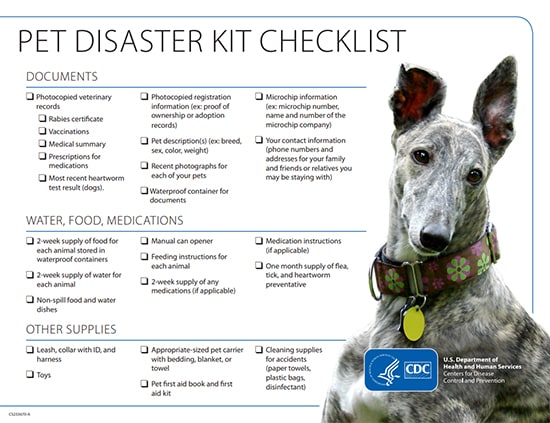
Pet Disaster Preparedness Kit
Wednesday, June 26th, 2019Prepare a disaster kit for your pet(s) with these items. Ask your veterinarian for help putting it together.
Documents
- Photocopied veterinary records
- Rabies certificate
- Vaccinations
- Medical summary
- Prescriptions for medications
- Most recent heartworm test result (dogs)
- Most recent FeLV/FIV test result (cats)
- Photocopied registration information (ex: proof of ownership or adoption records)
- Pet description(s) (ex: breed, sex, color, weight)
- Recent photographs of each of your pets
- Waterproof container for documents
- Microchip information (ex: microchip number, name and number of the microchip company)
- Your contact information (phone numbers and addresses for your family and friends or relatives you may be staying with)
- Pet boarding instructions Cdc-pdf[PDF – 2 pages]
Water, Food, Medications
- 2-week supply of food for each animal stored in waterproof containers
- 2-week supply of water for each animal
- Non-spill food and water dishes
- Manual can opener
- Feeding instructions for each animal
- 2-week supply of any medications (if applicable)
- Medication instructions (if applicable)
- 1-month supply of flea, tick, and heartworm preventative
Other Supplies
- Leash, collar with ID, and harness
- Litter and litterbox (cats)
- Toys
- Appropriate-sized pet carrier with bedding, blanket, or towel
- Pet first aid book and first aid kit
- Cleaning supplies for accidents (paper towels, plastic bags, disinfectant)
Pet Project: 5 Ways to Prep Your Pet for Emergencies
Wednesday, June 26th, 2019
Posted on June 24, 2019 by
Your pet is family. Their safety and wellbeing is a priority for you every day, but have you thought about what you would do with your pet in an emergency?
Many people don’t think about being prepared until an emergency is at their doorstep. When disaster strikes, they may choose to ignore evacuation orders because they don’t know what to do with their pets. Try to imagine having to make the decision to leave your pet behind during a flood, fire, hurricane, or other emergency—this was a reality for many pet owners during recent emergencies including hurricanes Florence and Michael, the California wildfires, and the eruption of Hawaii’s Kīlauea volcano in 2018.
Although you can never completely control what will happen during an emergency, you can take steps to be as prepared as possible for advance-notice disasters, like hurricanes, and no-notice emergencies, like house fires. By taking some easy actions now, you can avoid having to make difficult and dangerous decisions during an emergency.
- Get your pet microchipped. It is relatively inexpensive to have a veterinarian implant a microchip that contains the owner’s contact information. Owners can be located if a shelter or veterinary clinic scans the chip. Finding a lost pet that hasn’t be microchipped can be extremely difficult and many times impossible. If your pet is already microchipped, make sure the registration info is up-to-date so you can be contacted if your pet is found.
- Prepare a disaster kit for your pet ahead of time, along with your family’s personal needs. Include everything your pet will need, from food and prescriptions to leashes and bedding. Although this may mean purchasing twice as much stuff, it will be faster and easier to gather your pet’s items if you have them all together and ready for an emergency.
Collect and protect your pet’s veterinary records, rabies vaccination certificates, microchip information, and any prescriptions. Make sure items are stored with your important paperwork in waterproof containers. And don’t forget the most basic, but important, information—your contact information and a photo of your pet; preferably one of you with your pet as further proof of ownership.
Visit CDC’s Healthy Pets, Healthy People website for a detailed checklist of items to include in your pet’s emergency kit.
- Plan where your pet will stay in case you need to evacuate. Pets are often not allowed in evacuation centers unless they are service animals. You can ask out-of-town friends or relatives about keeping your pet in an emergency ahead of time, or you can check a website that lists pet-friendly hotels (com or tripswithpets.com) so you have some locations ready to book.Locate veterinary clinics and boarding facilities in areas where you plan to evacuate just in case you need to temporarily house your pet. You can also contact your local emergency management office to ask if they offer accommodations for owners and pets during a disaster.
- Use a buddy system with friends, family, and neighbors in case you’re not home during an emergency. Have a trusted person you can call to check on pets and evacuate them if necessary. Having a kit ready to go will make it easier for them if you aren’t there.
- Practice evacuating or sheltering in place with your pet. This will help familiarize your pet with the process so when the time comes, it won’t be scary for them. Training pets to be in their carriers can make them more comfortable and reduce the stress of getting everyone out safely. Know exactly how and where you will place your pet’s carrier and supplies in a vehicle.
For sheltering in place, pick a room with few or no windows, no toxic chemicals or plants, and make sure to close off small areas where frightened pets could get stuck. Include your pet in your family’s plan—everyone should know who will grab the pet(s), supplies, and where you will meet during an emergency.
Learn more about preparing your pet for emergencies on CDC’s Healthy Pets, Healthy People website.

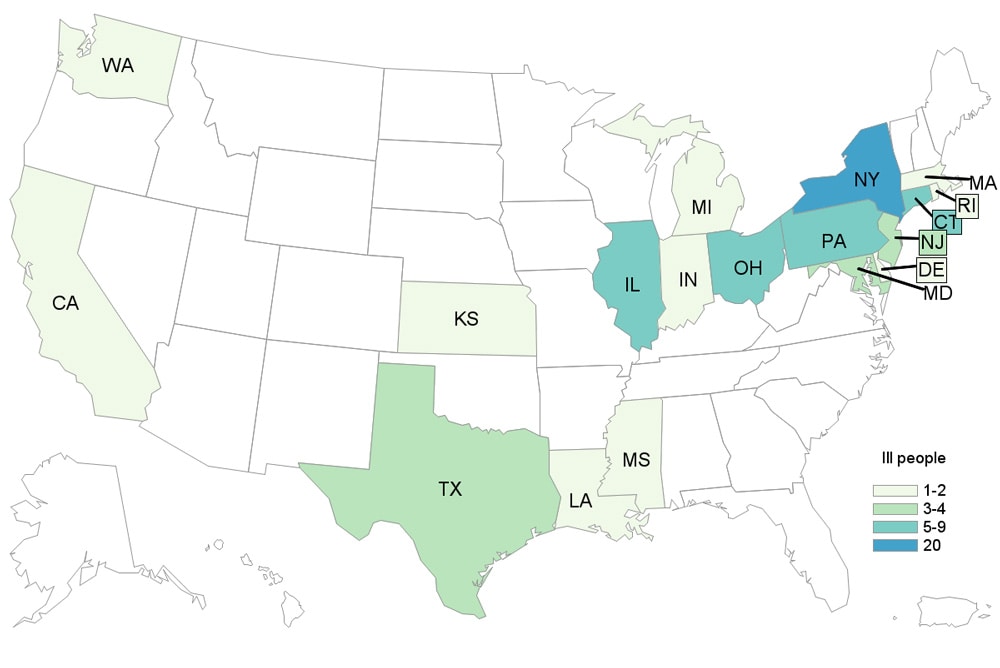
CDC: A multistate outbreak of Salmonella infections linked to contact with pet hedgehogs.
Saturday, June 1st, 2019
- Reported Cases: 27
- States: 17
- Hospitalizations: 2
- Deaths: 0
“……
- Since the last update on March 29, 2019, illnesses in an additional 10 people and six states have been added to this investigation.
- Twenty-seven people infected with the outbreak strain of Salmonella Typhimurium have been reported from 17 states.
- Two people were hospitalized. No deaths have been reported.
- Forty-two percent are children aged 12 or younger.
- Epidemiologic and laboratory evidence indicate that contact with pet hedgehogs is the likely source of this outbreak.
- In interviews, 18 (90%) of 20 ill people reported contact with a hedgehog.
- A common source of hedgehogs has not been identified.
- The outbreak strain making people sick was identified in samples collected from 10 hedgehogs in Minnesota, including 5 hedgehogs from the homes of five ill patients……”
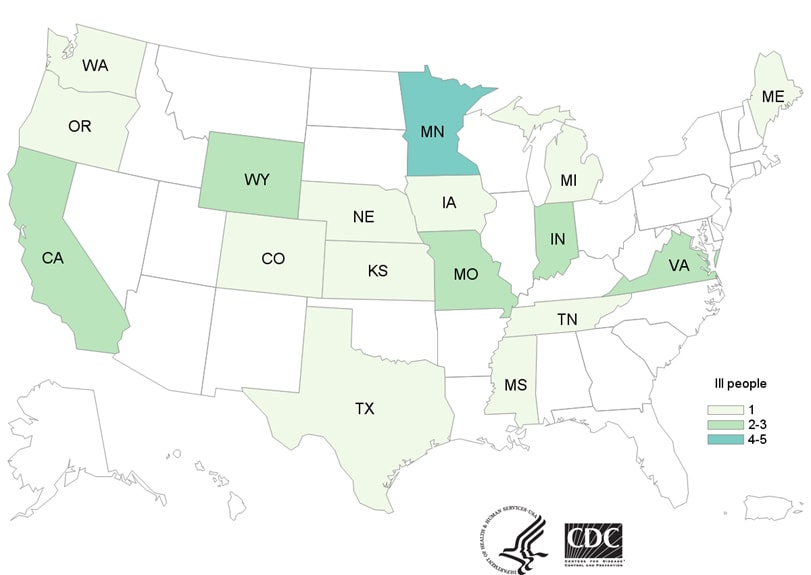
Epidemiologic, laboratory, and traceback evidence indicates that puppies sold through the commercial dog industry, an uncommon source of Campylobacter outbreaks, were the source of a multistate outbreak of multidrug-resistant Campylobacter infections.
Friday, September 21st, 2018“….The outbreak, which began in January 2016, affected a total of 118 people in 18 states through Feb 4, including 29 pet store employees, with 26 hospitalizations and no deaths reported….”
North Carolina & Florence: Millions of chickens and thousands of pigs died
Thursday, September 20th, 2018Flood Statement
National Weather Service Raleigh, NC
945 PM EDT Wed Sep 19 2018
…The Flood Warning continues for the following rivers in North
Carolina…
Little River At Manchester affecting Cumberland County
PRECAUTIONARY/PREPAREDNESS ACTIONS…
Safety message. If you encounter deep water while driving, do not
attempt to drive through. Turn around, dont drown.
&&
NCC051-201344-
/O.EXT.KRAH.FL.W.0011.000000T0000Z-180924T1648Z/
/MANN7.3.ER.180915T1619Z.180917T2200Z.180924T0448Z.NR/
945 PM EDT Wed Sep 19 2018
The Flood Warning continues for
the Little River At Manchester.
* At 9:30 PM Wednesday the stage was 28.0 feet.
* Flood stage is 18.0 feet.
* Major flooding is occurring and Major flooding is forecast.
* Forecast…The river will continue to fall to below flood stage by
early Monday morning.
* Impact…At 30.0 feet, Water reaches the base of the Bragg Blvd (Hwy
24/87) bridge across the Little River.
* Impact…At 28.0 feet, Flooding reaches the road surface of the
Manchester Road bridge.
* Impact…At 27.0 feet, Major flood stage. The Starlite motel is
flooded and Manchester Road is closed.
* Impact…At 25.0 feet, Water reaches the base of the Manchester Road
bridge and the foundation of the Starlite motel at the intersection
of Manchester Road and Bragg Blvd (Hwy 24/87).
* Impact…At 24.0 feet, Moderate flood stage. Manchester Road is
flooded.
* Impact…At 23.0 feet, Minor flooding begins on Manchester Road near
the Fort Bragg water treatment plant.
* Impact…At 18.0 feet, Flood stage. Minor flood problems begin in
Fort Bragg near the water treatment plant.
USDA: Safeguarding Food, Pets, Livestock before Hurricane Florence
Thursday, September 13th, 2018USDA Urges Local Residents to Safeguard Food, Pets, Livestock before Hurricane Florence
USDA Office of Communications sent this bulletin at 09/12/2018 10:44 AM EDT
You are subscribed to USDA Office of Communications.
Release No. 0182.18
Contact: USDA Press
Email: press@oc.usda.gov
USDA Urges Local Residents to Safeguard Food, Pets, Livestock before Hurricane Florence
WASHINGTON, Sept. 12, 2018 – The U.S. Department of Agriculture (USDA) reminds rural communities, farmers and ranchers, families and small businesses in the path of Hurricane Florence that USDA has programs that provide assistance in the wake of disasters. USDA staff in the regional, state and county offices that stand ready and eager to help.
“If we know anything about American farmers, it’s that they can handle adversity. Even so, USDA is ready to help with the resources they need to be able to weather storms and recover from damages,” U.S. Secretary of Agriculture Sonny Perdue said. “As hurricanes approach, we have USDA personnel in counties throughout the nation, standing by to assist in any way possible.”
Hurricane Florence currently is forecast to make landfall Saturday morning near the border between North Carolina and South Carolina, and then travel westward through South Carolina.
At the same time, Tropical Storm Isaac’s path may include Puerto Rico and the American Virgin Islands by Saturday morning. In the Pacific, Tropical Storm Olivia is forecast to move over the Hawaiian Islands late Tuesday into Wednesday, and Super Typhoon Mangkhut is moving away from Guam.
USDA encourages those in the path of the storms to take precautions to protect the safety of their food and animals.
Tips to best protect food safety before losing power:
- Keep appliance thermometers in both the refrigerator and the freezer to ensure temperatures remain food safe during a power outage. Safe temperatures are 40°F or lower in the refrigerator, 0°F or lower in the freezer.
- Freeze water in small plastic storage bags or containers prior to a storm. These containers are small enough to fit around the food in the refrigerator and freezer to help keep food cold.
- Freeze refrigerated items, such as leftovers, milk and fresh meat and poultry that you may not need immediately—this helps keep them at a safe temperature longer.
- Consider getting 50 pounds of dry or block ice if a lengthy power outage is possible. This amount of ice should keep a fully-stocked 18-cubic-feet freezer cold for two days.
- Group foods together in the freezer—this ‘igloo’ effect helps the food stay cold longer.
- Keep a few days’ worth of ready-to-eat foods that do not require cooking or cooling.
USDA’s Animal and Plant Health Inspection Service (APHIS) is urging everyone in the potential path of the hurricane to prepare now – not just for yourselves, but also for your pets and your livestock.
Protecting livestock during a disaster:
- Plan For Evacuation – Know how you will evacuate and where you will go. If it is not feasible to evacuate your livestock, be sure to provide adequate food and water that will last them until you can return, and a strong shelter.
- If you are planning to move livestock out of state, make sure to contact the State Veterinarian’s Office in the receiving state before you move any animals. You also may contact APHIS Veterinary Services state offices for information and assistance about protecting and moving livestock.
- Listen to Emergency Officials – Evacuate if asked to do so.
When major disasters strike, USDA has an emergency loan program that provides eligible farmers low-interest loans to help them recover from production and physical losses. USDA’s emergency loan program is triggered when a natural disaster is designated by the Secretary of Agriculture or a natural disaster or emergency is declared by the President under the Stafford Act. USDA also offers additional programs tailored to the needs of specific agricultural sectors to help producers weather the financial impacts of major disasters and rebuild their operations.
Helping producers weather financial impacts of disasters:
Livestock owners and contract growers who experience above normal livestock deaths due to specific weather events, as well as to disease or animal attacks, may qualify for assistance under USDA’s Livestock Indemnity Program.
Livestock, honeybee and farm-raised fish producers who suffer animal, feed, grazing and associated transportation cost losses due to an extreme weather event may qualify for assistance through USDA’s emergency assistance program tailored for their agricultural sectors. Producers who suffer losses to or are preventing from planting agricultural commodities not covered by federal crop insurance may be eligible for assistance under USDA’s Noninsured Crop Disaster Assistance Programs if the losses were due to natural disasters.
Helping operations recover after disasters:
USDA also can provide financial resources through its Environmental Quality Incentives Program to help with immediate needs and long-term support to help recover from natural disasters and conserve water resources.
Farmers and ranchers needing to rehabilitate farmland damaged by natural disasters can apply for assistance through USDA’s Emergency Conservation Program. USDA also has assistance available for eligible private forest landowners who need to restore forestland damaged by natural disasters through the Emergency Forest Restoration Program. USDA’s Emergency Watershed Protection Program also can help relieve imminent threats to life and property caused by flood, fires and other natural disasters that impair a watershed.
Orchardists and nursery tree growers may be eligible for assistance through USDA’s Tree Assistance Program to help replant or rehabilitate eligible trees, bushes, and vines damaged by natural disasters.
Producers with coverage through the Risk Management Agency (RMA) administered Federal crop insurance program should contact their crop insurance agent for issues regarding filing claims. Those who purchased crop insurance will be paid for covered losses. Producers should report crop damage within 72 hours of damage discovery and follow up in writing within 15 days. The Approved Insurance Providers (AIP), loss adjusters and agents are experienced and well trained in handling these types of events. As part of its commitment to delivering excellent customer service, RMA is working closely with AIPs that sell and service crop insurance policies to ensure enough loss adjusters will be available to process claims in the affected areas as quickly as possible. Please visit the RMA website – www.rma.usda.gov for more details.
UN: The Korean peninsular and Southeast Asia may be next to report outbreaks of African swine fever after the rapid onset of the deadly pig disease in China
Wednesday, August 29th, 2018A United States-FAO partnership working to strengthen the capacity of developing countries to manage outbreaks of diseases in farm animals has in just 12 months succeeded in training over 4,700 veterinary health professionals in 25 countries in Africa, Asia and the Middle East.
Wednesday, March 14th, 2018March 2018, Rome – A United States-FAO partnership working to strengthen the capacity of developing countries to manage outbreaks of diseases in farm animals has in just 12 months succeeded in training over 4,700 veterinary health professionals in 25 countries in Africa, Asia and the Middle East.
The FAO-provided technical trainings covered a gamut of key competencies, including disease surveillance and forecasting, laboratory operations, biosafety and biosecurity, prevention and control methods and outbreak response strategies.
All told, 3,266 vets in Asia, 619 in West Africa, 459 in East Africa, and 363 in the Middle East benefitted. They are on the front line of the effort to stop new diseases at their source. (Full list below)
“Over the course of this relationship we’ve learned that there are many mutually beneficial areas of interest between the food and agricultural community and the human health community,” said Dennis Carroll, Director of USAID’s Global Health Security and Development Unit.
“A partnership with FAO not only enables us to protect human populations from future viral threats, but also to protect animal populations from viruses that could decimate food supplies. It’s not just a global health, infectious disease issue, but also a food security, food safety, and economic growth issue,” Carroll added.
“Some 75 percent of new infectious diseases that have emerged in recent decades originated in animals before jumping to us Homo sapiens, a terrestrial mammal. This is why improving adequately discovering and tackling animal disease threats at source represents a strategic high-ground in pre-empting future pandemics,” said Juan Lubroth, FAO Chief Veterinary Officer
“A proactive approach is absolutely critical, and for that, the world needs well-trained, up-to-speed professionals — biologists, ecologists, microbiologists, modellers, physicians and veterinarians — which is why the United States’ consistent support for building up that kind of capacity has been invaluable,” Lubroth said.
Viral risks
Population growth, agricultural expansion and environmental encroachment, and the rise of inter-continental food supply chains in recent decades have dramatically altered how diseases emerge, jump species boundaries, and spread, FAO studies have shown.
A new study just published by USAID’s Dennis Carroll and experts from several institutions including FAO suggests that just 0.01 percent of the viruses behind zoonotic disease outbreaks are known to science. The authors have proposed an international partnership, The Global Virome Project, aimed at characterizing the most risky of these. Doing so would allow more proactive responses to disease threats, with benefits not only for public health but also for the livelihoods of poor, livestock-depending farming communities.
Partnering for global health security
The close FAO-USAID partnership on animal health goes back over a decade.
Experts from the two organizations are meeting in Rome this week to review progress achieved in the past year and how to respond to threats like species-jumping zoonotic illnesses and the growing trends of antimicrobial resistance and options for intervention measures in food production and protection of public health.
In addition to trainings, via the USAID- Emerging Pandemic Threats (EPT) programme, FAO conducts research and advises on policy in order to help countries increase their resilience to disease emergence and protect animal and human health.
And to enable rapid responses by governments to disease events FAO has leveraged USAID support to work with the United Nations Humanitarian Response Depots to establish a series of emergency equipment and gear stockpiles in 15 countries that facilitate rapid and adequate responses to outbreaks.
FAO is also key player and advisor to the Global Health Security Agenda (GHSA), a growing partnership of over 60 countries, NGOs and international organizations working to improve early detection of and responses to infectious disease threats. USAID support under the GHSA umbrella is helping FAO engage with 17 countries in Africa and Asia to strengthen capabilities to detect and respond to zoonotic diseases.
Thanks to USAID support for the EPT and GSHA, FAO is actively tackling disease issues and building national capacities in over 30 countries
Economic impacts as well as health consequences
Beyond the risks posed to human health, animal diseases can cost billions of dollars and hamstringing economic growth.
The most damaging outbreaks of high impact disease in recent decades all had an animal source, including H5N1 highly pathogenic avian influenza, H1N1 pandemic influenza, Ebola, severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS).
For example, the H5N1 outbreak of the mid-2000s caused an estimated $30 billion in economic losses, globally; a few years later, H1N1 racked up as much as $55 billion in damages.
Not to mention that for millions of the world’s poorest people, animals are their primary capital assets — “equity on four legs”. Losing them can push these families out of self-reliance and into destitution.
Note to editors. The countries where the trainings took place were: Bangladesh, Burkina Faso, Cambodia, Cameroon, China, Democratic Republic of the Congo, Egypt, Ghana, Guinea, Indonesia, Jordan, Kenya, Laos People’s Democratic Republic , Liberia, Mali, Myanmar, Nepal, Senegal, Sierra Leone, United Republic of Tanzania, Uganda and Viet Nam.