Archive for the ‘Lassa Fever’ Category
Health authorities in Liberia on Monday declared a health emergency following the outbreak of Lassa fever which has so far claimed 21 lives this year.
Wednesday, September 4th, 2019Illnesses on the rise from mosquito, tick, and flea bites
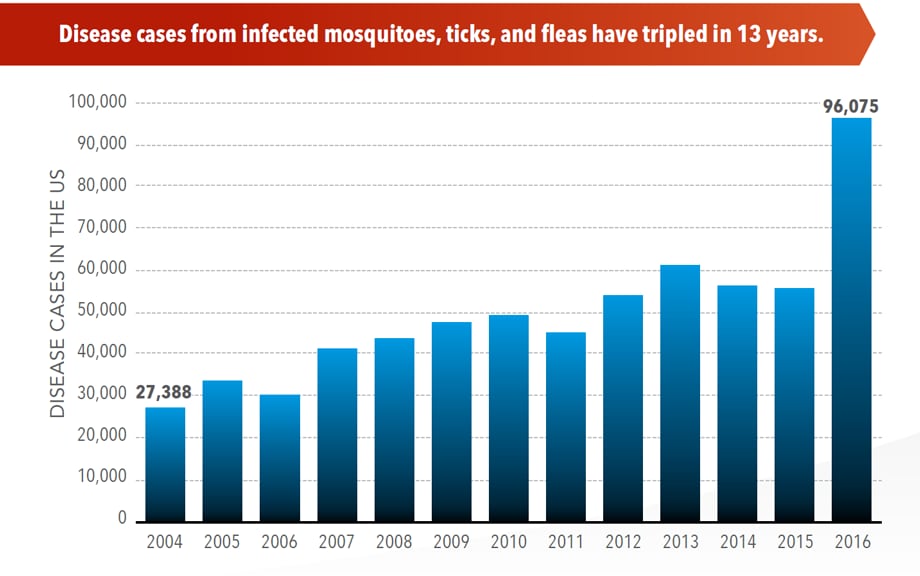
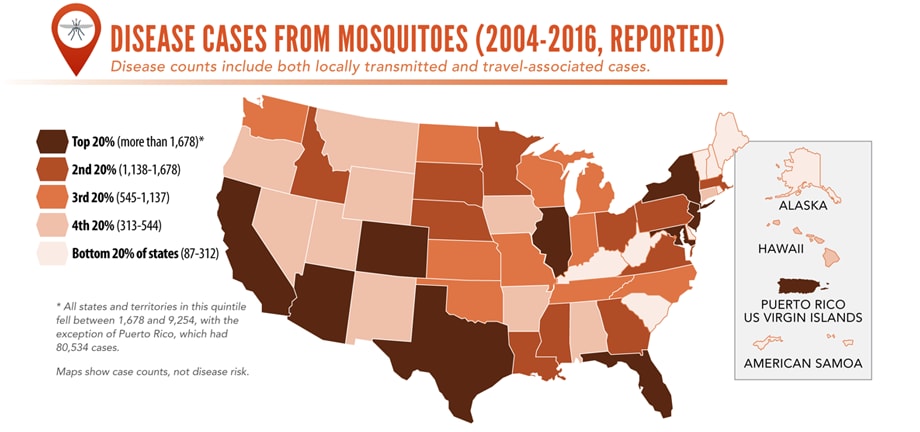
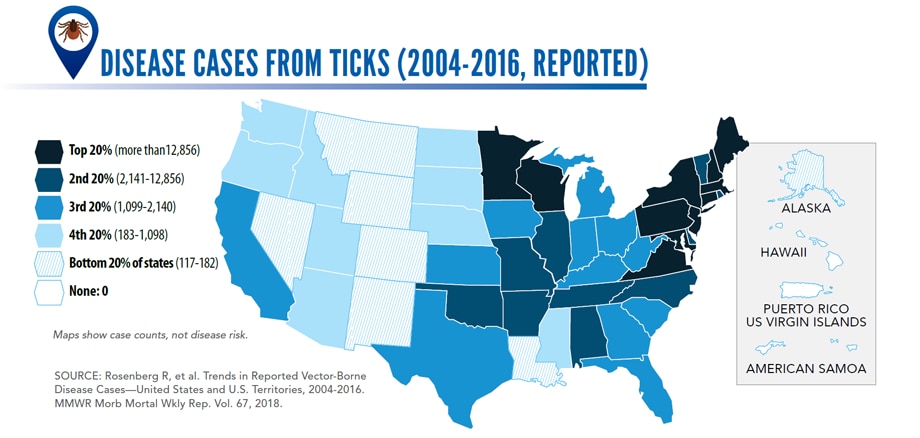
Sunday, June 2nd, 2019Almost everyone has been bitten by a mosquito, tick, or flea. These can be vectors for spreading pathogens (germs). A person who gets bitten by a vector and gets sick has a vector-borne disease, like dengue, Zika, Lyme, or plague. Between 2004 and 2016, more than 640,000 cases of these diseases were reported, and 9 new germs spread by bites from infected mosquitoes and ticks were discovered or introduced in the US. State and local health departments and vector control organizations are the nation’s main defense against this increasing threat. Yet, 84% of local vector control organizations lack at least 1 of 5 core vector control competencies. Better control of mosquitoes and ticks is needed to protect people from these costly and deadly diseases.
State and local public health agencies can
- Build and sustain public health programs that test and track germs and the mosquitoes and ticks that spread them.
- Train vector control staff on 5 core competencies for conducting prevention and control activities. http://bit.ly/2FG1OMwExternal
- Educate the public about how to prevent bites and control germs spread by mosquitoes, ticks, and fleas in their communities.
Increasing threat, limited capacity to respond
More cases in the US (2004-2016)
- The number of reported cases of disease from mosquito, tick, and flea bites has more than tripled.
- More than 640,000 cases of these diseases were reported from 2004 to 2016.
- Disease cases from ticks have doubled.
- Mosquito-borne disease epidemics happen more frequently.
More germs (2004-2016)
- Chikungunya and Zika viruses caused outbreaks in the US for the first time.
- Seven new tickborne germs can infect people in the US.
More people at risk
- Commerce moves mosquitoes, ticks, and fleas around the world.
- Infected travelers can introduce and spread germs across the world.
- Mosquitoes and ticks move germs into new areas of the US, causing more people to be at risk.
The US is not fully prepared
-
- Local and state health departments and vector control organizations face increasing demands to respond to these threats.
- More than 80% of vector control organizations report needing improvement in 1 or more of 5 core competencies, such as testing for pesticide resistance.
- More proven and publicly accepted mosquito and tick control methods are needed to prevent and control these diseases.
Lassa Fever Outbreak in Nigeria, 2018
Friday, May 24th, 2019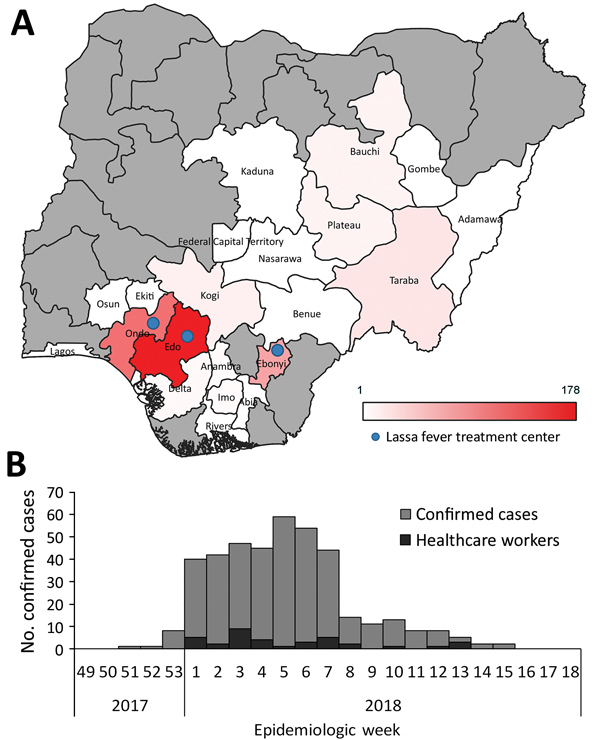
Ilori EA, Furuse Y, Ipadeola OB, et al. Epidemiologic and Clinical Features of Lassa Fever Outbreak in Nigeria, January 1–May 6, 2018. Emerging Infectious Diseases. 2019;25(6):1066-1074. doi:10.3201/eid2506.181035.
“Lassa fever (LF) is endemic to Nigeria, where the disease causes substantial rates of illness and death. In this article, we report an analysis of the epidemiologic and clinical aspects of the LF outbreak that occurred in Nigeria during January 1–May 6, 2018. A total of 1,893 cases were reported; 423 were laboratory-confirmed cases, among which 106 deaths were recorded (case-fatality rate 25.1%). Among all confirmed cases, 37 occurred in healthcare workers. The secondary attack rate among 5,001 contacts was 0.56%. Most (80.6%) confirmed cases were reported from 3 states (Edo, Ondo, and Ebonyi). Fatal outcomes were significantly associated with being elderly; no administration of ribavirin; and the presence of a cough, hemorrhaging, and unconsciousness. The findings in this study should lead to further LF research and provide guidance to those preparing to respond to future outbreaks.“
Lassa and Crimean-Congo Hemorrhagic Fever in Mali
Saturday, April 27th, 2019Baumann, J., Knüpfer, M., Ouedraogo, J., Traoré, B. Y., Heitzer, A., Kané, B….Wölfel, R. (2019). Lassa and Crimean-Congo Hemorrhagic Fever Viruses, Mali. Emerging Infectious Diseases, 25(5), 999-1002.
“…..We detected LASV RNA in blood samples from 2 patients, a 5-year-old boy and a 13-year-old girl. Both children were treated for episodes of high fever during September–October 2016 at the Hôpital du Mali……..Using reverse transcription quantitative PCR, we detected acute CCHFV infection in 2 patients hospitalized at Hospital Gabriel Touré in April 2017, a 1-year-old boy (cycle threshold 32.74) and a 2-year-old boy (cycle threshold 36.95)…….”
2018: Lassa Fever in Nigeria
Saturday, April 27th, 2019| Ilori EA, Frank C, Dan-Nwafor CC, Ipadeola O, Krings A, Ukponu W, et al. Increase in Lassa Fever Cases in Nigeria, January–March 2018. Emerg Infect Dis. 2019;25(5):1026-1027.
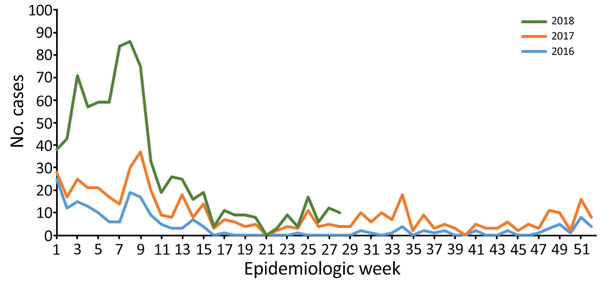
Weekly trends of confirmed Lassa fever cases, Nigeria, 2016–2018.
“……A total of 107 laboratory-confirmed cases were reported during the first 12 weeks of 2017 and 394 during the same period in 2018. Among confirmed and probable cases, 50 deaths were reported during the peak season in 2017 and 104 in 2018. ……” |
Nigeria: 15 newly recorded Lassa Fever cases raise the outbreak total to 510 cases.
Thursday, April 4th, 2019The Lassa fever outbreak in Nigeria grew by 23 cases in the past week
Wednesday, March 27th, 2019 In the reporting Week 11 (11th – 17th March, 2019) 23 new confirmedi cases were reported from nine states – Edo(8), Ondo(4), Ebonyi(3), Bauchi(3), Taraba(1), Imo(1), Enugu(1), Benue(1) and Kebbi(1) with four new deaths in Edo (2), Benue(1) and Bauchi(1) States From 1st January to 17th March, 2019, a total of 1801 suspectedi cases have been reported from states. Of these, 495 were confirmed positive, 15 probable and 1277 negative (not a case)-Table 1 Since the onset of the 2019 outbreak, there have been 114* deaths in confirmed cases. Case fatality ratio in confirmed cases is 23.0%
Weekly summary of major outbreaks in Africa
Wednesday, March 13th, 2019Plague: Uganda
2 Cases
1 Death: 50% CFR
Ebola virus disease: Democratic Republic of the Congo
921 Cases
582 Deaths: 63% CFR
Hepatitis E: Namibia
4 669 Cases
41 Deaths: 0.9% CFR
Lassa fever: Nigeria
420 Cases
93 Deaths: CFR 22.1%
From 1 January through 10 February 2019, 327 cases of Lassa fever (324 confirmed cases and three probable cases) with 72 deaths (case fatality ratio = 22%) have been reported in Nigeria
Sunday, February 17th, 2019Lassa Fever – Nigeria
From 1 January through 10 February 2019, 327 cases of Lassa fever (324 confirmed cases and three probable cases) with 72 deaths (case fatality ratio = 22%) have been reported across 20 states and the Federal Capital Territory, with the majority of cases being reported from Edo (108) and Ondo (103) states. Twelve cases have been reported among healthcare workers in seven states – Edo (4), Ondo (3), Ebonyi (1), Enugu (1), Rivers (1), Bauchi (1) and Benue (1) including one death in Enugu.
The number of confirmed cases reported across Nigeria remains high. In week 6, 2019 (week ending 10 February 2019), 37 new confirmed cases including 10 deaths (case fatality ratio = 27%) were reported from nine states across Nigeria. The majority of cases were reported from Ondo (12) and Edo (10) states. The number of confirmed cases reported in week 6, 2019 represents a slight decrease compared to week 5 when 68 confirmed cases were reported (Figure 1).
Of the 3746 contacts identified since January 2019, 2658 are still under follow-up while 1045 have completed 21 days of follow-up. Sixty contacts became symptomatic, of which 39 tested positive.
Ninety-one case-patients are currently in admission at treatment centers across the country. The case-patients are being treated with standard supportive care.
Figure 1: Number of confirmed and probable Lassa fever cases in Nigeria reported by the week of illness onset from 1 January through 10 February 2019
Source: Nigeria Centre for Disease Control (NCDC)
Public health response
- On 22 January 2019, the Nigeria Center for Disease Control (NCDC) declared the outbreak an emergency.
- Multi-sectoral One Health national rapid response teams have been deployed to Ondo, Edo, Ebonyi, Plateau, and Bauchi to support field investigation and response activities.
- Enhanced surveillance is ongoing in all states following alert communication and a press release from NCDC.
- Treatment of Lassa fever cases is also ongoing at designated treatment centres across the country.
- Risk communication and community engagement activities continue in the states. National awareness was improved through the recently concluded international Lassa fever conference which took place from 16 through 17 January 2019.
WHO risk assessment
Lassa fever is a viral haemorrhagic fever that is transmitted to humans via contact with food or household items contaminated with rodent urine or faeces. Person-to-person infections and laboratory transmission can also occur. The overall case fatality rate is 1%; it is 15% among patients hospitalized with severe illness. There is currently no approved vaccine. Early supportive care with rehydration and symptomatic treatment improves survival.
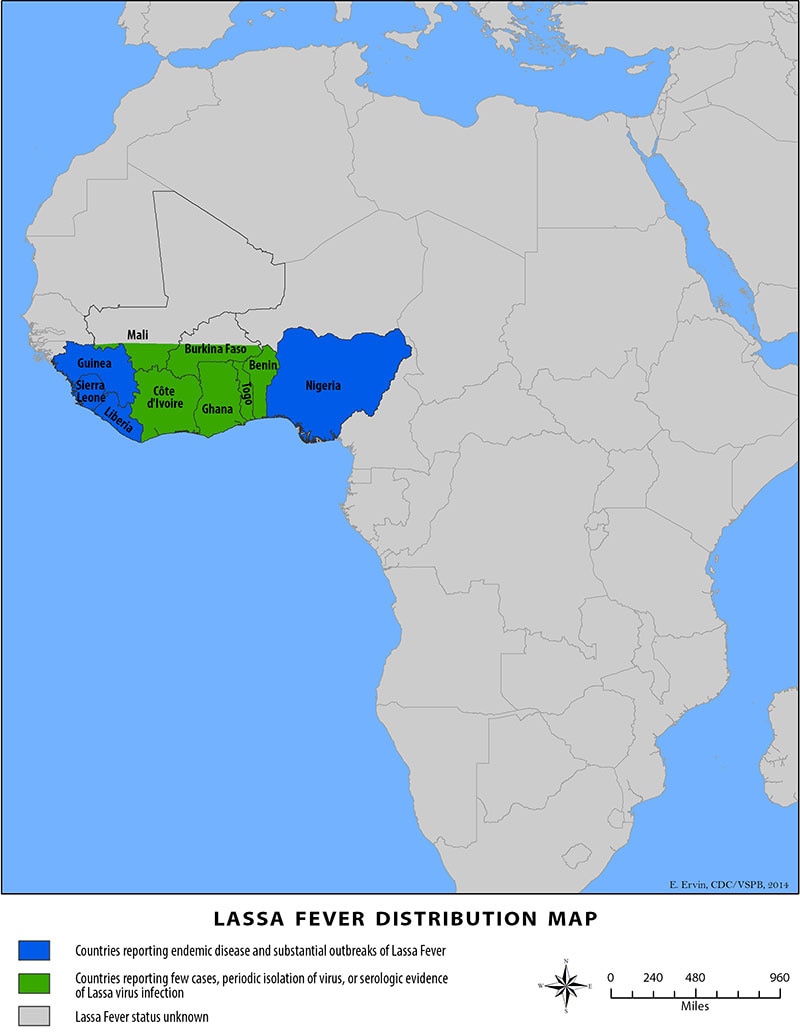
Although Lassa fever is known to be endemic in Nigeria with the peak season anticipated from December through June, the current increase in new confirmed cases and deaths should be monitored closely and addressed appropriately. Cases in neigbouring Benin and Togo potentially originating from Nigeria have been reported in previous years and therefore neighbouring countries should be monitored accordingly.
With twelve confirmed cases so far among healthcare workers, there is evidence of nosocomial transmission of the disease amidst reports of inadequate infection prevention and control (IPC) supplied in some health facilities and complacency on the part of health workers towards maintaining IPC measures.
WHO advice
Prevention of Lassa fever relies on community engagement and promoting hygienic conditions to discourage rodents from entering homes. In healthcare settings, staff should consistently implement standard infection prevention and control measures when caring for patients to prevent nosocomial infections. WHO continues to advice all countries in the Lassa fever belt on the need to enhance early detection and treatment of cases to reduce the case fatality rate as well as strengthen cross-border collaboration.
WHO does not recommend any travel or trade restriction to Nigeria based on the currently available information.
For more information on Lassa fever, please see the link below: