Archive for the ‘Food-borne diseases’ Category
Food Safety form your FDA
Thursday, September 5th, 2019Prepare Yourself Before Power Emergencies
- Make sure you have appliance thermometers in your refrigerator and freezer.
- Check to ensure that the freezer temperature is at or below 0° F, and the refrigerator is at or below 40° F.
- In case of a power outage, the appliance thermometers will indicate the temperatures in the refrigerator and freezer to help you determine if the food is safe.
- Freeze containers of water for ice to help keep food cold in the freezer, refrigerator, or coolers in case the power goes out. If your normal water supply is contaminated or unavailable, the melting ice will also supply drinking water.
- Freeze refrigerated items such as leftovers, milk, and fresh meat and poultry that you may not need immediately. This helps keep them at a safe temperature longer.
- Group food together in the freezer. This helps the food stay cold longer.
- Have coolers on hand to keep refrigerated food cold if the power will be out for more than 4 hours.
- Purchase or make ice cubes in advance, and freeze gel packs ahead of time. Store all of these in the freezer for future use in the refrigerator or in coolers.
- Check out local sources to know where dry ice and block ice can be purchased, in case it should be needed.
-
- Store food on shelves that will be safely out of the way of contaminated water in case of flooding.
- Make sure to have a supply of bottled water stored where it will be as safe as possible from flooding. If your bottled water has an odor, do not drink or use it. Instead, dispose of it, or if applicable, call your bottled water provider to make arrangements to get a replacement.
During an emergency, if you use food or beverage containers to hold non-food substances like gasoline, dispose of them after use and do not recycle them.
Power Outages: During and After
When the Power Goes Out . . .
Here are basic tips for keeping food safe:
- Keep the refrigerator and freezer doors closed as much as possible to maintain the cold temperature.
- The refrigerator will keep food cold for about 4 hours if it is unopened.
- A full freezer will keep the temperature for approximately 48 hours (24 hours if it is half full) if the door remains closed.
- Buy dry or block ice to keep the refrigerator as cold as possible if the power is going to be out for a prolonged period of time. Fifty pounds of dry ice should keep an 18 cubic foot, fully stocked freezer cold for two days.
-
- If you plan to eat refrigerated or frozen meat, poultry, fish, or eggs while they are still at safe temperatures, it is important that each item is thoroughly cooked to a safe minimum internal temperature to ensure that any foodborne bacteria that may be present are destroyed. However, if at any point the food was above 40º F for 2 hours or more (or 1 hour if temperatures are above 90 º F) — discard it.
Once Power is Restored . . .
Determine the safety of your food:
- If an appliance thermometer was kept in the freezer, check the temperature when the power comes back on. If the freezer thermometer reads 40° F or below, the food is safe and may be refrozen.
- If a thermometer has not been kept in the freezer, check each package of food to determine its safety. You can’t rely on appearance or odor. If the food still contains ice crystals or is 40° F or below, it is safe to refreeze or cook.
- Refrigerated food should be safe as long as the power was out for no more than 4 hours and the refrigerator door was kept shut. Discard any perishable food (such as meat, poultry, fish, eggs, or leftovers) that has been at temperatures above 40° F for 2 hours or more (or 1 hour if temperatures are above 90º F).
Perishable food such as meat, poultry, seafood, milk, and eggs that are not kept adequately refrigerated or frozen may cause illness if consumed, even when they are thoroughly cooked.
If Flooding Occurs
-
Be prepared to safely handle food and water in the event that flooding occurs.
Keep Water Safe
Follow these steps to keep your WATER SAFE during and after flood conditions.
- Only use water from a safe source for drinking and washing or preparing food.
- Use bottled water that has not been exposed to flood waters, if it is available.
- If you don’t have bottled water, you should boil or disinfect water to make it safe. (see steps below)
- If you have a well that has been flooded, the water should be tested and disinfected after flood waters recede. If you suspect that your well may be contaminated, contact your local or state health department or agricultural extension agent for specific advice.
How to Boil or Disinfect Water To Make It Safe
If the water is cloudy, first filter it through clean cloths, or allow it to settle and then draw off the clear water for boiling/ disinfecting. Then, follow one of these two procedures:
- Boiling Boiling water will kill most types of disease-causing organisms that may be present.
- Boil the water for 1 minute.
- Let it cool, and store it in clean containers with covers.
Disinfecting with Bleach
Bleach will kill some, but not all, types of disease-causing organisms that may be in the water.
- Add 1/8 teaspoon (or 8 drops) of unscented household (5.25% concentration) liquid bleach for each gallon of water.
- Stir it well and let it stand for 30 minutes before you use it.
- Store disinfected water in clean containers with covers.
Keep Food Safe
Follow these steps to keep your FOOD SAFE during and after flood conditions.
- Do not eat any food that may have come into contact with flood water.
- Discard any food and beverage that is not in a waterproof container if there is any chance that it has come into contact with flood water.
- Food containers that are waterproof include undamaged, commercially prepared foods in all-metal cans and “retort pouches” (like flexible, shelf-stable juice or seafood pouches).
-
-
- Food containers that are not waterproof include those with screw-caps, snap lids, pull tops, and crimped caps.
- Also discard cardboard juice/milk/baby formula boxes and home canned foods if they have come in contact with flood water, because they cannot be effectively cleaned and sanitized.
- Discard any food in damaged cans. Damaged cans are those with swelling, leakage, punctures, holes, fractures, extensive deep rusting, or crushing/denting that is severe enough to prevent normal stacking or opening with a manual, wheel-type can opener. See box on next page for steps to clean/save undamaged packages.
- Thoroughly wash metal pans, ceramic dishes, and utensils (including can openers) with soap and water, using hot water if available. Rinse and then sanitize them by boiling in clean water or immersing them for 15 minutes in a solution of 1 tablespoon of unscented household (5.25% concentration) liquid bleach per gallon of water.
- Thoroughly wash countertops with soap and water, using hot water if available. Rinse and then sanitize by applying a solution of 1 tablespoon of unscented household (5.25% concentration) liquid bleach per gallon of water. Allow to air dry.
How To Save Undamaged Food Packages Exposed to Flood Water
-
- Undamaged, commercially prepared foods in all-metal cans and “retort pouches” (like flexible, shelf-stable juice or seafood pouches) can be saved if you follow this procedure.
- Remove the labels, if they are the removable kind, since they can harbor dirt and bacteria.
- Brush or wipe away any dirt or silt.
- Thoroughly wash the cans or retort pouches with soap and water, using hot water if it is available.
- Rinse the cans or retort pouches with water that is safe for drinking, if available, since dirt or residual soap will reduce the effectiveness of chlorine sanitation.
- Sanitize cans and retort pouches by immersion in one of the two following ways:
- Place in water and allow the water to come to a boil and continue boiling for 2 minutes.
- Place in a solution of 1 cup (8 oz/250 mL) of unscented household (5.25% concentration) bleach mixed with 5 gallons of water and soak for 15 minutes.
- Air dry cans or retort pouches for a minimum of 1 hour before opening or storing.
- If the labels were removable, then re-label your cans or retort pouches, including the expiration date, with a permanent marking pen.
Food in reconditioned cans or retort pouches should be used as soon as possible thereafter.
Baby Formula Tip
For infants, try to use prepared, canned baby formula that requires no added water. Otherwise, dilute any concentrated baby formula in reconditioned, all-metal containers with clean drinking water.
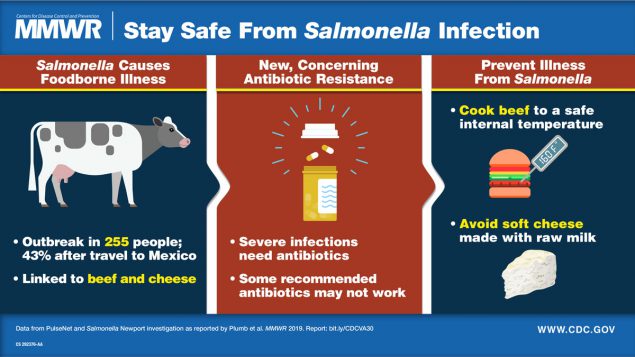
“…During June 2018–March 2019, an outbreak caused by multidrug-resistant Salmonella Newport with decreased susceptibility to azithromycin led to 255 infections and 60 hospitalizations. Infections were linked to Mexican-style soft cheese obtained in Mexico and beef obtained in the United States….”
Saturday, August 24th, 2019Plumb ID, Schwensohn CA, Gieraltowski L, et al. Outbreak of Salmonella Newport Infections with Decreased Susceptibility to Azithromycin Linked to Beef Obtained in the United States and Soft Cheese Obtained in Mexico — United States, 2018–2019. MMWR Morb Mortal Wkly Rep 2019;68:713–717. DOI: http://dx.doi.org/10.15585/mmwr.mm6833a1external icon
The Costa Rican government has issued a national alert saying that alcohol tainted with methanol is behind 19 deaths.
Saturday, July 27th, 2019Daily Mail
CDC: 62 people in 8 US states have fallen ill this year from Salmonella related to fresh papayas imported from Mexico
Sunday, June 30th, 2019“……The illnesses range from mid-January up to June 8, with the highest number occurring in April. Of those who’ve gotten sick, 23 have been hospitalized.
So far, no deaths are reported…..”
A methanol poisoning cluster in Malaysia and deaths have been reported.
Tuesday, June 25th, 2019“…..For the period of June 11 to June 21, 2019, where three methanol poisoning clusters reported to the National Crisis Preparedness and Response Center (CPRC).
The incidents involved 19 cases…..”

WHO: Food Safety Facts
Sunday, June 9th, 2019Food Safety Facts
- An estimated 600 million people – almost 1 in 10 people in the world – fall ill after eating contaminated food and 420 000 die every year.
- Children aged under 5 carry 40% of the foodborne disease burden, with 125 000 deaths every year.
- Foodborne illnesses are caused by bacteria, viruses, parasites or chemical substances entering the body through contaminated food or water.
- Foodborne diseases impede socioeconomic development by straining health care systems and harming national economies, tourism and trade.
- The value of trade in food is US$ 1.6 trillion, which is approximately 10% of total annual trade globally.
- Recent estimates indicate that the impact of unsafe food costs low- and middle-income economies around US$ 95 billion in lost productivity each year.
- Improving hygiene practices in the food and agricultural sectors helps to reduce the emergence and spread of antimicrobial resistance along the food chain and in the environment.
The first UN World Food Safety Day to be marked on Friday 7 June
Friday, June 7th, 2019The first ever celebration of the United Nations World Food Safety Day, to be marked globally on 7 June, aims to strengthen efforts to ensure that the food we eat is safe.
Every year, nearly one in ten people in the world (an estimated 600 million people) fall ill and 420,000 die after eating food contaminated by bacteria, viruses, parasites or chemical substances. Unsafe food also hinders development in many low- and middle-income economies, which lose around US$ 95 billion in productivity associated with illness, disability, and premature death suffered by workers.
World Food Safety Day 2019’s theme is that food safety is everyone’s business. Food safety contributes to food security, human health, economic prosperity, agriculture, market access, tourism and sustainable development.
The UN has designated two of its agencies, the Food and Agriculture Organization (FAO) and the World Health Organization (WHO) to lead efforts in promoting food safety around the world.
FAO and WHO are joining forces to assist countries to prevent, manage and respond to risks along the food supply chain, working with food producers and vendors, regulatory authorities and civil society stakeholders, whether the food is domestically produced or imported.
“Whether you are a farmer, farm supplier, food processor, transporter, marketer or consumer, food safety is your business,” FAO Director-General José Graziano da Silva said. “There is no food security without food safety,” he said.
“Unsafe food kills an estimated 420,000 people every year. These deaths are entirely preventable,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “World Food Safety Day is a unique opportunity to raise awareness about the dangers of unsafe food with governments, producers, handlers and consumers. From farm to plate, we all have a role to play in making food safe.”
Investing in sustainable food systems pays off
FAO and WHO underline the importance of everyone’s access to safe, nutritious and sufficient food, and that safe food is critical to promoting health and ending hunger, two of the primary aims of the Sustainable Development Goals.
Safe food allows for suitable intake of nutrients and contributes to a healthy life. Safe food production improves sustainability by enabling market access and productivity, which drives economic development and poverty alleviation, especially in rural areas.
Investment in consumer food safety education has the potential to reduce foodborne disease and return savings of up to $10 for each dollar invested.
Get involved in World Food Safety Day
Activities around the world for World Food Safety Day aim to inspire action to help prevent, detect and manage foodborne health risks.
The right actions along the food supply chain, from farmers to consumers, as well as good governance and regulations, are essential to food safety.
FAO and WHO have created a new guide to show how everyone can get involved. The guide includes five steps to make a sustained difference to food safety:
- Ensure it’s safe. Governments must ensure safe and nutritious food for all.
- Grow it safe. Agriculture and food producers need to adopt good practices.
- Keep it safe. Business operators must make sure food is safely transported, stored and prepared.
-
- Check it’s safe. Consumers need access to timely, clear and reliable information about the nutritional and disease risks associated with their food choices.
- Team up for safety. Governments, regional economic bodies, UN organizations, development agencies, trade organizations, consumer and producer groups, academic and research institutions and private sector entities must work together on food safety issues.
Starting in 2019, every 7 June will be a time to highlight the benefits of safe food. World Food Safety Day was adopted by the United Nations General Assembly in December 2018. The process was initiated in 2016 by Costa Rica through the Codex Alimentarius Commission, which is managed by FAO and WHO.
People infected with the outbreak strain of E. coli O103, by state of residence, as of May 10, 2019 (n=196)
Wednesday, May 15th, 2019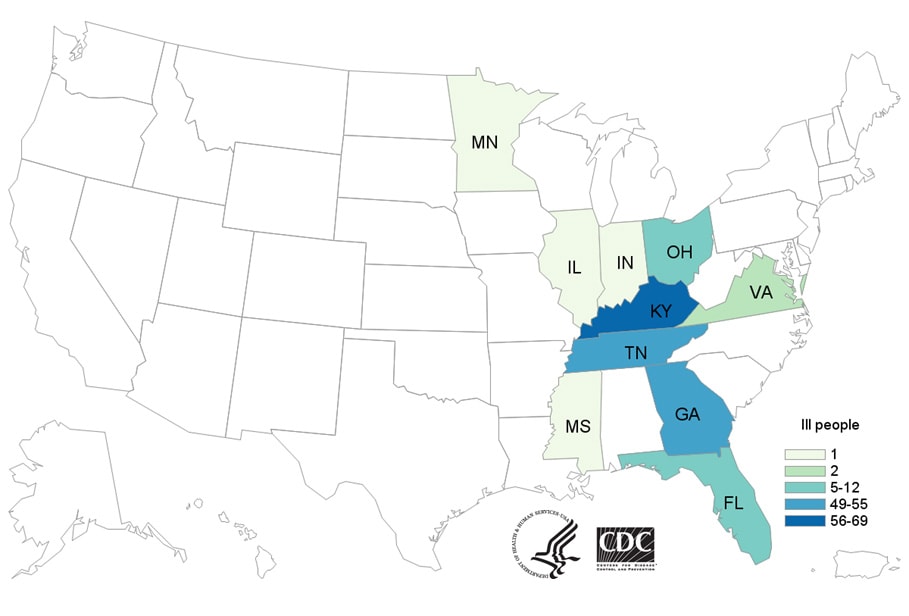
India: At least 7 have died and 87 others were taken seriously ill after allegedly consuming spurious liquor.
Thursday, May 2nd, 2019“……“After the polls were over, a group of local youths held a feast to rejoice and consumed liquor there. They came back home in the night and slept outside their houses as it was too hot inside. They complained of severe stomach pain and headache in the wee hours and were rushed to hospitals, where seven of them died,” said a local youth on condition of anonymity. …..”
CDC: Annual snapshot of foodborne illnesses
Monday, April 29th, 2019
Tack DM, Marder EP, Griffin PM, et al. Preliminary Incidence and Trends of Infections with Pathogens Transmitted Commonly Through Food — Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2015–2018. MMWR Morb Mortal Wkly Rep 2019;68:369–373. DOI: http://dx.doi.org/10.15585/mmwr.mm6816a2External.


