Archive for the ‘Cancer’ Category
Cervical cancer worldwide
Friday, December 6th, 2019- There were 570,000 cases and 311,000 deaths worldwide last in 2018.
- The average age of diagnosis was 53.
- In 42 low-resource countries, it was the most common cancer in women.
- A third of the cervical cancer burden fell on China and India together.
Inequities in cervical cancer care in indigenous Peruvian women (about 25% of Peru’s population is indigenous)
Saturday, April 20th, 2019Betel quid chewing & cancer
Thursday, November 30th, 2017“…..People start to enjoy the betel quid chewing starting in the
adolescence, and is associated with alcohol drinking and smoking. The
practice can lead to oral cancer.
In 2017, 67 (22 percent) out of 307 cancer patients in Taungoo public
hospital were suffering from head and neck cancer. Among them, 41 were
males and 26 were females. Males were aged in average 59.2 years
(range 36-81 years) and females were about 58.7 years old (range 19-86
years). Most of the cancers were in the oral cavity (34.3 percent),
followed by larynx (25.4 percent), oropharynx (11.9 percent),
nasopharynx (11.9 percent), hypopharynx (10.4 percent), lips (4.5
percent), and nose (1.5 percent).
As for social factors, about 20 patients (30 percent) had the habit of
betel quid chewing, 19 patients (28 percent) chewed betel quid and
smoked, and 19 patients (28 percent) chewed betel quid, smoked, and
drank alcohol…..”
Betel Quid with Tobacco (Gutka)
Betel quid is a combination of betel leaf, areca nut, and slaked lime.
In many countries, tobacco is also added, and the product is known as gutka, ghutka, or gutkha.
Other ingredients and flavorants are also added according to local preferences and customs (e.g., sweeteners, catechu, or spices such as cardamom, saffron, cloves, anise seeds, turmeric, and mustard).
Gutka is commercially available in foil packets and tins and is consumed by placing a pinch of the mixture in the mouth between the gum and cheek and gently sucking and chewing. The excess saliva produced by chewing may be swallowed or spit out.2
Use
- Betel quid and gutka use is reported to have stimulant and relaxation effects.2
- Global estimates report that up to 600 million men and women use some variety of betel quid.2
- Betel quid with or without tobacco is widely used in the Indian subcontinent (i.e., Bangladesh, India, Pakistan) as well as throughout Asia and the Pacific region (e.g., Cambodia, China, Indonesia, Malaysia, Philippines, Taiwan, Thailand).1,2,3,5
Health Effects
The following conditions have been associated with betel quid/gutka use:
Precancerous conditions
- Oral precancerous lesions, including erythroplakia (a reddened patch in the mouth) and leukoplakia (a white patch on the mucous membranes in the mouth that cannot be wiped off).2,6
- Oral submucous fibrosis (OSF), a precancerous lesion that stiffens the soft pink tissue that lines the inside of the mouth (i.e., oral mucosa).
Cancer
- Oral cancers—predominantly carcinomas of the lip, mouth, tongue, and pharynx2,6,8
- Cancer of the esophagus2
Other health effects
- Reproductive health outcomes such as increased risk of having a low birth-weight infant7
- Nicotine addiction4
References
- National Cancer Institute, Centers for Disease Control and Prevention, Stockholm Centre of Public Health. Smokeless Tobacco Fact Sheets. Third International Conference on Smokeless Tobacco; Stockholm. September 22–25, 2002 [cited 2015 Nov 27].
- World Health Organization. Betel-Quid and Areca-Nut Chewing and Some Areca-Nut-Derived Nitrosamines; Volume 85 [PDF–7.44 MB]. Lyon (France): World Health Organization, International Agency for Research on Cancer, 2004 [accessed 2015 Nov 27].
- Global Surveillance of Oral Tobacco Products: Total Nicotine, Unionised Nicotine and Tobacco-Specific N-nitrosamines. Tobacco Control 2011;20:e2, May 1, 2011 (10.1136/tc.2010.037465) [cited 2015 Nov 27].
- World Health Organization. Tobacco: Deadly in Any Form or Disguise
[PDF–2.58 MB]. Geneva: World Health Organization, 2006 [accessed 2015 Nov 27]. - Centers for Disease Control and Prevention. Use of Cigarettes and Other Tobacco Products Among Students Aged 13–15 Years—Worldwide, 1999–2005. Morbidity and Mortality Weekly Report 2006;55(20):553–6 [accessed 2015 Nov 27].
- Alert for an Epidemic of Oral Cancer Due to Use of the Betel Quid Substitutes Gutkha and Pan Masala: A Review of Agents and Causative Mechanisms. Mutagenesi 2004;19(9):251–62 [accessed 2015 Nov 27].
- Smokeless Tobacco and Health in India and South Asia. Respirology 2003;8(4):419–31 [cited 2015 Nov 27].
- Epidemiology of Betel Quid Usage [PDF–43.77 KB]. Annals Academy of Medicine Singapore 2004;33(Suppl):31S–36S [accessed 2015 Nov 27].
For Further Information
Centers for Disease Control and Prevention
National Center for Chronic Disease Prevention and Health Promotion
Office on Smoking and Health
E-mail: tobaccoinfo@cdc.gov
Phone: 1-800-CDC-INFO
Media Inquiries: Contact CDC’s Office on Smoking and Health press line at 770-488-5493.
February 4 is World Cancer Day: Global Cancer Burden
Saturday, February 4th, 2017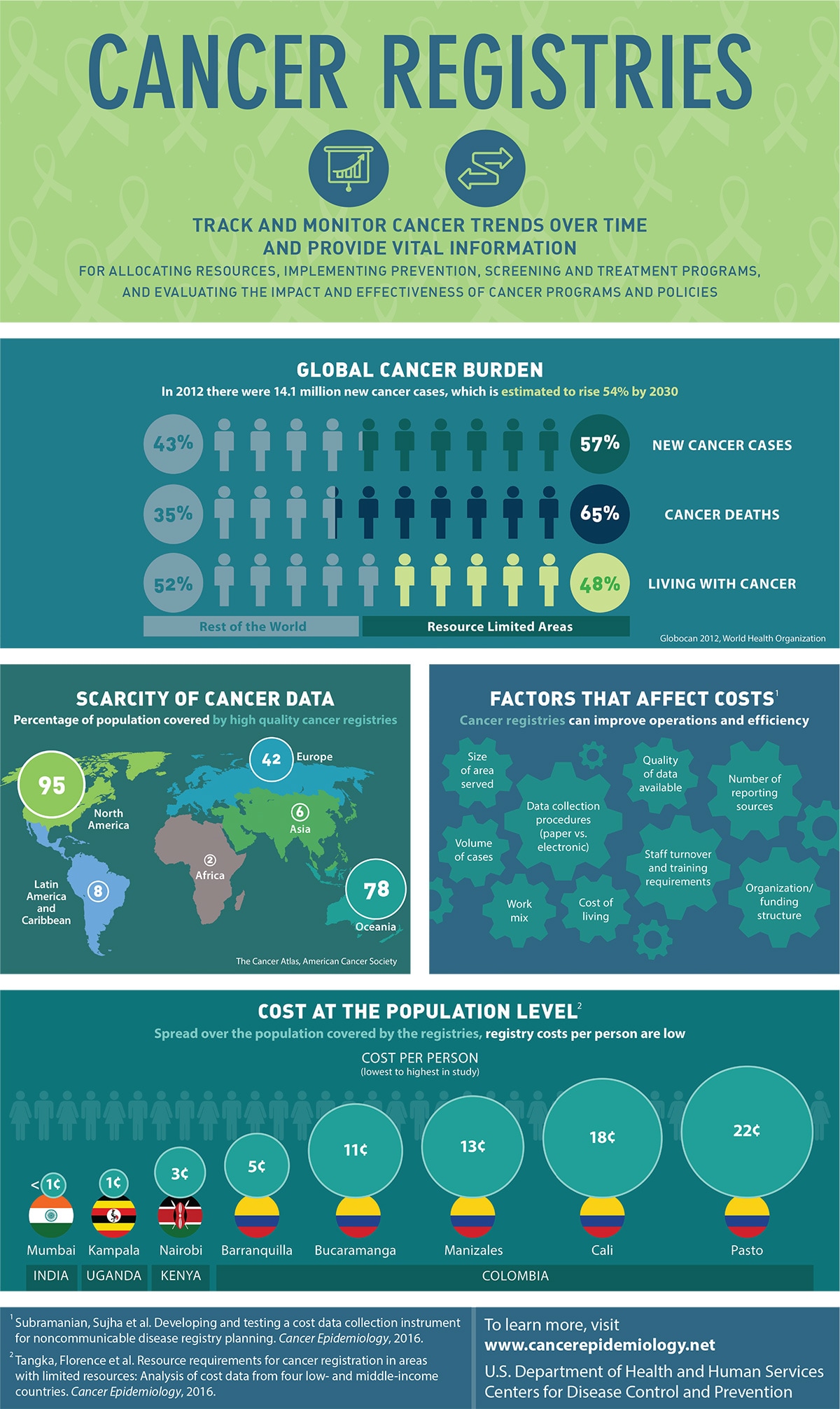
Cancer Registries
Track and monitor cancer trends over time and provide vital information for allocating resources, implementing prevention, screening and treatment programs, and evaluating the impact and effectiveness of cancer programs and policies
Global Cancer Burden
In 2012 there were 14.1 million new cancer cases, which is estimated to rise 54% by 2030
- 57% New cancer cases
- 65% cancer deaths
- 46% Living with cancers
Source: Globocan 2012, World Health Organization
Scarcity of Cancer Data
Percentage of population covered by high quality cancer registries
- 95% North America
- 8% Latin America and Caribbean
- 2% Africa
- 42% Europe
- 6% Asia
- 78% Oceania
Source: The Cancer Atlas, American Cancer Society
Factors that Affect Costs 1
Cancer registries can improve operations and efficiency
- Size of area served
- Data collection procedures (paper vs. electronic)
- Volume of cases
- Quality of Data available
- Number of reporting sources
- Staff turnover and training requirements
- Cost of living
- Organization/funding structure
Cost at the Population Level2
Spread over the population covered by the registries, registry costs per person are low
Cost per person (lowest to highest in study)
India
- Mumbai, less than 1 cent
Uganda
- Kampala, 1 cent
Kenya
- Nairobi, 3 cents
Colombia
- Barranquilla, 5 cents
- Bucaramanga, 11 cents
- Manizales, 13 cents
- Cali, 18 cents
- Pasto, 22 cents
To learn more, visit http://www.cancerepidemiology.net
U.S. Department of Health and Human Services
Centers for Disease Control and Prevention
1Subramanian, Sujha et al. Developing and testing a cost data collection instrument for noncommunicable disease registry planning. Cancer Epidemiology, 2016.
2Tangka, Florence et al. Resource requirements for cancer registration in areas with limited resources: Analysis of cost data from four low- and middle-income countries. Cancer Epidemiology, 2016.
If a proposal introduced by the Health Ministry is adopted, Russia will ban the sale of cigarettes to people born in 2015 and after.
Friday, January 13th, 2017- Tobacco kills about six million people globally each year, according to the World Health Organization, and 300,000 to 400,000 of them are Russians.
- About 33 percent of Russian adults use tobacco products.
** Cancer statistics in China, 2015: China is facing 2.8 million deaths just in in 2015, with lung cancer crowning the top of the list of cancer cases.
Tuesday, February 2nd, 2016CA: A Cancer Journal for Clinicians
With increasing incidence and mortality, cancer is the leading cause of death in China and is a major public health problem. Because of China’s massive population (1.37 billion), previous national incidence and mortality estimates have been limited to small samples of the population using data from the 1990s or based on a specific year. With high-quality data from an additional number of population-based registries now available through the National Central Cancer Registry of China, the authors analyzed data from 72 local, population-based cancer registries (2009-2011), representing 6.5% of the population, to estimate the number of new cases and cancer deaths for 2015. Data from 22 registries were used for trend analyses (2000-2011).
The results indicated that an estimated 4292,000 new cancer cases and 2814,000 cancer deaths would occur in China in 2015, with lung cancer being the most common incident cancer and the leading cause of cancer death. Stomach, esophageal, and liver cancers were also commonly diagnosed and were identified as leading causes of cancer death.
Residents of rural areas had significantly higher age-standardized (Segi population) incidence and mortality rates for all cancers combined than urban residents (213.6 per 100,000 vs 191.5 per 100,000 for incidence; 149.0 per 100,000 vs 109.5 per 100,000 for mortality, respectively). For all cancers combined, the incidence rates were stable during 2000 through 2011 for males (+0.2% per year; P = .1), whereas they increased significantly (+2.2% per year; P < .05) among females. In contrast, the mortality rates since 2006 have decreased significantly for both males (−1.4% per year; P < .05) and females (−1.1% per year; P < .05). Many of the estimated cancer cases and deaths can be prevented through reducing the prevalence of risk factors, while increasing the effectiveness of clinical care delivery, particularly for those living in rural areas and in disadvantaged populations. CA Cancer J Clin 2016. © 2016 American Cancer Society.