Archive for the ‘Listeria’ Category
CDC: A multistate outbreak of Listeria infections linked to deli-sliced meats and cheeses.
Friday, April 19th, 2019
- A total of 8 people infected with the outbreak strain of Listeria monocytogenes have been reported from 4 states.
- All 8 people have been hospitalized, and one death has been reported from Michigan.
- Epidemiologic and laboratory evidence indicates that meats and cheeses sliced at deli counters might be contaminated with Listeria monocytogenes and could make people sick.
- In interviews, ill people report eating different types and brands of products, including meats and cheeses, purchased from and sliced at deli counters in many different retail locations.
- The outbreak strain has been identified in samples taken from meat sliced at a deli and from deli counters in multiple stores.
- A single, common supplier of deli products has not been identified.
- CDC is not advising that consumers avoid eating products prepared at delis, or that retailers stop selling deli-sliced products.
- Retailers should clean and sanitize deli slicers frequently and other areas where deli products are prepared, stored, or served to avoid cross contamination.
- This outbreak is a reminder that people at higher risk for severe Listeria infection should handle deli-sliced meats and cheeses carefully to prevent illness. Pregnant women and their newborns, adults age 65 and older, and people with weakened immune systems are more likely to get sick with listeriosis.
Ontario, Canada: Listeria monocytogenes associated with pasteurized chocolate milk
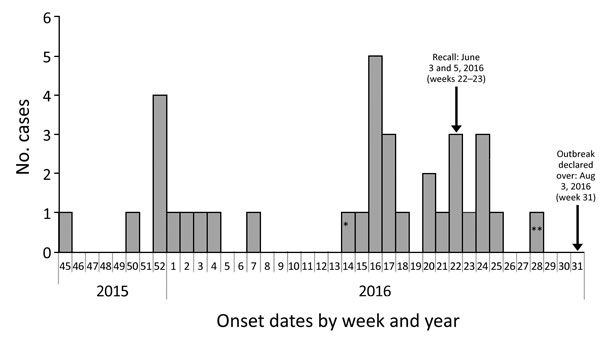
Sunday, February 3rd, 2019“……Thirty-four case-patients met the outbreak definition; only Ontario residents were identified. Eleven case-patients had an onset date during November 14, 2015–February 14, 2016. Onset dates ranged from April 11 to June 20, 2016, for 21 case-patients in the second wave; the remaining 2 case-patients were outliers (Figure 1). Median age was 73 years (range <1 years–90 years). More than half of the case-patients were female (20/34, 59%). Hospitalizations occurred for 32 (94%) case-patients, and 4 deaths (12%) were reported...…”
Hanson H, Whitfield Y, Lee C, Badiani T, Minielly C, Fenik J, et al. Listeria monocytogenes associated with pasteurized chocolate milk, Ontario, Canada. Emerg Infect Dis. 2019 Mar [date cited]. https://doi.org/10.3201/eid2503.18-0742

South Africa: The world’s largest known listeria outbreak and it was all due to tainted baloney!
Monday, April 2nd, 2018The world’s largest known listeria outbreak has spread throughout South Africa for 15 months, killing 189 people. Health officials believe they have identified the source: bologna.
Since January last year, 982 confirmed cases of listeriosis had been recorded, the National Institute for Communicable Diseases in South Africa reported on Thursday. The infection, caused by food that has been contaminated with the bacterium Listeria monocytogenes, is often lethal.
A cluster of gastroenteritis cases among toddlers in a Johannesburg hospital this January led authorities to the sandwich meat in a day care center’s refrigerator — and in turn, to a meat production facility in the northern city of Polokwane. There, officials said they detected traces of LST6, the listeria strain identified in 91 percent of the outbreak’s cases.
The Listeriosis outbreak in South Africa is now the largest ever reported to the WHO.
Friday, March 30th, 2018In South Africa, an outbreak of listeriosis, a serious foodborne disease, has been ongoing since the start of 2017. Between 1 January 2017 through 14 March 2018, 978 laboratory-confirmed listeriosis cases have been reported to the National Institute for Communicable Diseases (NICD) from all provinces. The majority of cases have come from three provinces: 581 (59%) from Gauteng, 118 (12%) from Western Cape and 70 (7%) from KwaZulu-Natal provinces, with the remaining cases coming from the other provinces in South Africa. The outcome of illness is known for 674 patients, of whom 183 (27%) of them died; this case fatality rate is comparable to other recorded listeriosis outbreaks worldwide. Most of the cases are persons who have higher risks for a severe disease outcome, such as neonates, pregnant women, the elderly and immunocompromised persons. In this outbreak, 42% of the cases are neonates who were infected during pregnancy or delivery.
Whole genome sequencing was performed on isolates from a large subset of patients. Ninety one percent of the strains belonged to Listeria monocytogenes Sequence Type 6 (ST6). The same ST6 sequence type was identified in a widely consumed ready-to-eat processed meat product called “Polony”. The same strain was also found in the processing environment of the manufacturer of the implicated product. On 4 March 2018, the Ministry of Health, announced that this product was believed to be the source of the outbreak.
The food processing company and three of its retailers export to 15 countries1 in the African region . All of these countries have issued recalls for the implicated products. Environmental samples from other food production companies in South Africa have also tested positive for Listeria but with strains different from the outbreak strain. These companies have also issued food recalls. Some of their products have been exported to some of the countries mentioned above.
Nine percent of the reported cases in the present outbreak in South Africa were infected with different strains of Listeria than the predominant ST6 outbreak strain. This may indicate that more than one outbreak is ongoing. Comprehensive investigations to identify the source of infection of these cases should be conducted.
Number of Laboratory-Confirmed Cases of Listeriosis by Week of Sample Collection and Province, South Africa, 01 January 2017 to 12 March 2018 (n=978)
Source: National Institute for Communicable Diseases (NICD), South Africa2.
Public health response
The country has activated a national multisectoral task force to coordinate investigation and response activities:
- The Minister of Health, South Africa, held a press conference on 4 March 2018 to announce the source of the outbreak.
- Following the source identification, the national authorities have taken measures to limit further infections and associated mortality, including but not limited to the issuance of safety recall notices, compliance notices, and measures related to exportation of implicated products and risk communication with vulnerable groups.
- The Southern African Development Community (SADC) Health Ministers held a meeting in Johannesburg on 15 March 2018, to share information and to enhance preparedness and response for listeriosis. Health Ministers were further reminded about their rights and obligations under the International Health Regulations (IHR) with regards to additional health measures for international travel and trade.
- Listeriosis has been made a notifiable medical condition in South Africa Since December 2017.
- National risk communication activities have been initiated since December 2017 around the “WHO five keys to safer food messages”.
WHO risk assessment
Globally, this is the largest outbreak of listeriosis that has been detected. Due to the potentially long incubation period of listeriosis (one to three weeks and up to 70 days) further cases are expected before the impact of the food recall is observed.
Following the identification of the source of this outbreak, WHO is now concerned that the export of implicated products may have resulted in listeriosis cases in other countries. Detailed information on the implicated product batches exported to each of the identified 15 countries should be shared with WHO and the International Food Safety Authorities Network (INFOSAN) Secretariat. This will help to facilitate efficient recalls of these products.
Recently, Namibia reported a confirmed case of listeriosis. It is important that this case and other possible cases be properly investigated and the implicated food sources identified. The isolated Listeria strains should be sequenced to determine potential links to the outbreak in South Africa. Some of these countries may not have well-established surveillance systems and laboratory diagnostic services in place to detect cases of listeriosis. In such cases, WHO is ready to provide support and has reached out to 16 African nations (two West African countries and 14 members of SADC) to provide support for preparedness and response.
An increase in public concern about the outbreak has been reflected in media reports and discussions in various social media platforms.
WHO advice
Countries should strengthen national food safety and disease surveillance systems as a prerequisite to prevent similar events in the future and to ensure a safe food supply for their populations. Additionally, countries are urged to pay closer attention to common foodborne pathogens such as Salmonella species, Campylobacter jejuni, Escherichia coli and Listeria monocytogenes, to make listeriosis a notifiable disease if not yet done, to make the best use of a new “WHO manual to strengthen surveillance of and response to foodborne diseases”, which was published on November 2017 and to refer to the “WHO Factsheet on Listeriosis”. See below, in the “Further Information” section for links to these documents.
Responsible authorities are encouraged to proactively provide public health advice on the prevention and control of listeriosis, including, strengthened risk communication, to address public concerns and promote outbreak control measures .
WHO does not currently recommend any travel or trade restrictions in relation to this outbreak, other than the recall of processed meat products indicated by the South African Government.
While WHO understands the desire by sovereign governments to take measures to protect the health of their populations, States Parties to the IHR have obligations not to take actions that significantly interfere with international travel and trade which are not based on scientific principles and which may be viewed as excessive. Indeed such measures contravene the spirit and purpose of the IHR, and can impede public health objectives.
Currently, 12 out of 15 countries have recalled the implicated processed meat products, and banned imports of the same, while three out of these countries have additionally banned imports of other food products. WHO continues to monitor the travel and trade measures taken by countries in relation to this outbreak and their compliance with requirements under the IHR.
For travellers, it is advisable to practice good food hygiene, such as avoiding uncooked food, avoiding food that has been kept at room temperature for several hours, and always washing hands thoroughly with soap and water before preparing or consuming food.
1The 15 countries include: Angola, Botswana, Democratic Republic of the Congo, Ghana, Lesotho, Madagascar, Malawi, Mauritius, Mozambique, Namibia, Nigeria, Swaziland, Uganda, Zambia, and Zimbabwe.
2The provinces are: Western Cape (WC), North West (NW), Northern Cape (NC), Mpumalanga (MP), Limpopo (LP), KwaZulu-Natal (KZ), Gauteng (GA), Free State (FS) and Eastern Cape (EC).
Further information:
WHO & Listeria: Nearly 200 South Africans have died since January 2017 as a result of contaminated ready-to-eat meat products
Wednesday, March 21st, 201820 March 2018 | Brazzaville, Republic of the Congo – The World Health Organization has reached out to 16 African nations to provide support for preparedness and response to a listeriosis outbreak that started in South Africa in 2017 but is now threatening other countries on the continent.
Nearly 200 South Africans have died since January 2017 as a result of contaminated ready-to-eat meat products that are widely consumed in South Africa and may also have been exported to two West African countries and 14 members of the South African Development Community (SADC).[1]
South African health authorities recently declared the source of the outbreak as a factory in Polokwane, South Africa. This prompted a national and international recall of the food products. However, in light of the potentially long incubation period of listeriosis and the challenges relating to large scale nationwide recall processes, further cases are likely to occur.
Namibia has reported one confirmed case of listeriosis, a man who was admitted to hospital in early March. An investigation is ongoing to determine whether the case is connected to the outbreak in South Africa.
WHO’s Health Emergencies programme, the Global Outbreak alert and Response Network (GOARN) and the International Food Safety Authorities Network (INFOSAN) are working with the 16 priority countries to improve their ability to prepare for, detect and respond to potential outbreaks.
Immediate steps will include increasing awareness on listeriosis, enhancing active surveillance and laboratory diagnosis, ensuring readiness of Rapid Response Teams, and strengthening coordination and contingency planning. Experts have been deployed to South Africa, Lesotho and Swaziland to support these efforts.
“This outbreak is a wake up call for countries in the region to strengthen their national food safety and disease surveillance systems,” said Dr Matshidiso Moeti, WHO Regional Director for Africa.
The link between the contaminated products, the producing company and strains of Listeria isolated from the patients was made by the use of whole genome sequencing of isolated strains of the Listeria bacteria. WHO is supporting further genome sequencing to determine which cases are linked to this on-going outbreak.
In March, South Africa hosted a meeting of SADC health ministers to address regional preparedness and response to listeriosis. Ministers committed to regional collaboration, exchanging information and strengthening national food safety systems in line with international standards.
WHO does not currently recommend any trade related measures in relation to the current outbreak of listeriosis in South Africa, other than the recall of products identified as sources of infection.
Countries are encouraged to pay more attention to common foodborne pathogens such as Salmonella, Campylobacter, E.coli and Listeria, to notify WHO of listeriosis outbreaks in line with the International Health Regulations (2005), and to make use of WHO guidelines to strengthen surveillance of and response to the foodborne disease
***
[1] Angola, Botswana, the Democratic Republic of the Congo, Ghana, Lesotho, Madagascar, Malawi, Mauritius, Mozambique, Namibia, Nigeria, Swaziland, Tanzania, Uganda, Zambia and Zimbabwe