Archive for the ‘MERS-CoV’ Category
MERS: Up close
Monday, January 27th, 2020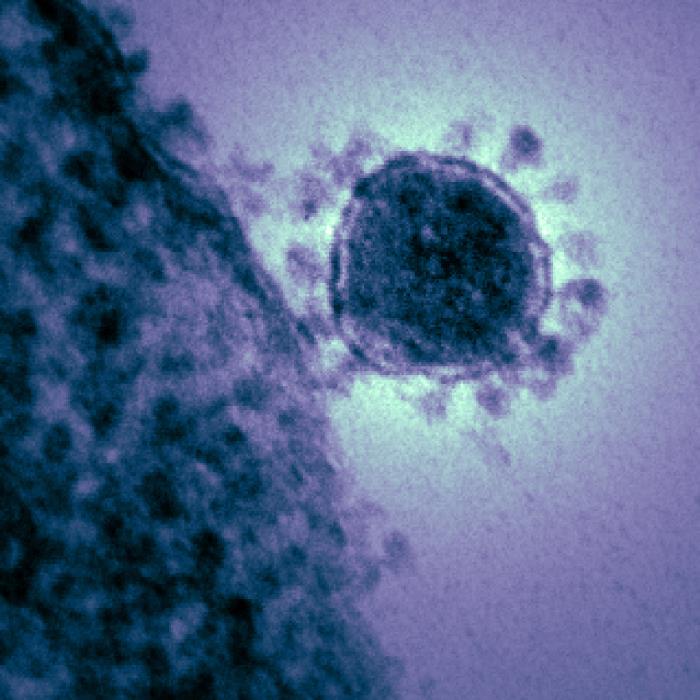
MERS-CoV in Pakistan
Thursday, November 7th, 2019ABSTRACT: ” A high percentage of camel handlers in Saudi Arabia are seropositive for Middle East respiratory syndrome coronavirus. We found that 12/100 camel handlers and their family members in Pakistan, a country with extensive camel MERS-CoV infection, were seropositive, indicating that MERS-CoV infection of these populations extends beyond the Arabian Peninsula.
Zheng J, Hassan S, Alagaili AN, Alshukairi AN, Amor NMS, Mukhtar N, et al. Middle East respiratory syndrome coronavirus seropositivity in camel handlers and their families, Pakistan. Emerg Infect Dis. 2019 Dec [date cited]. https://doi.org/10.3201/eid2512.191169
As of Sep 19, the WHO has stated that, since 2012 officials have confirmed 2,468 MERS cases worldwide, at least 850 of them fatal and the vast majority of infections have been in Saudi Arabia.
Thursday, October 17th, 2019Date التاريخ
Event# رقم الحدث
Description
الوصف
13/10/2019 19-1957
MERS in Khamis meshait city: 26-year-old female in Khamis meshait city, Aseer region Contact with camels: Unknown Case classification: Secondary Current status: Active
62
13/10/2019 19-1958
MERS in Buraidah city: 27-year-old female in Wadi Aldwasir city, Riyadh region Contact with camels: Unknown Case classification: Primary Current status: Active
MERS SITUATION UPDATE AUGUST 20
Friday, September 20th, 20192464 Laboratory-confirmed cases reported since April 2012
12 countries reported cases since April 2012
27 countries reported cases globally
850 deaths reported since April 2012 in the Eastern Mediterranean Region
Saudi Arabia reports 9 additional laboratory-confirmed cases of Middle East respiratory syndrome (MERS-CoV) infection and 4 associated deaths.
Tuesday, August 27th, 2019Middle East respiratory syndrome coronavirus (MERS-CoV) – The Kingdom of Saudi Arabia
From 1 through 31 July 2019, the National IHR Focal Point of Saudi Arabia reported 9 additional laboratory-confirmed cases of Middle East respiratory syndrome (MERS-CoV) infection and 4 associated deaths. The cases were reported from Riyadh (5 cases), Najran (3 cases), Al-Qassim (1 case) regions. There were no clusters of cases reported during this time period.
The link below provides details of the 9 reported cases :
From 2012 until 31 July 2019, the total number of laboratory-confirmed MERS-CoV infection cases reported globally to WHO is 2458, with 849 associated deaths. The global number reflects the total number of laboratory-confirmed cases reported to WHO under International Health Regulations (IHR 2005) to date. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected member states.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high mortality. Humans are infected with MERS-CoV from direct or indirect contact with dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
The notification of additional cases does not change the overall risk assessment. WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, animal products (for example, consumption of camel’s raw milk), or humans (for example, in a health care setting or household contacts).
WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV infection early because like other respiratory infections, the early symptoms of MERS-CoV infection are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures.
Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
MERS-CoV causes more severe disease in people with underlying chronic medical conditions such as diabetes mellitus, renal failure, chronic lung disease, and compromised immune systems. Therefore, people with these underlying medical conditions should avoid close unprotected contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine or eating meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
Investigating a cluster of Middle East respiratory syndrome (MERS) cases in a women-only dormitory in Riyadh, Saudi Arabia
Tuesday, August 20th, 2019Van Kerkhove MD, Aswad S, Assiri A, Perera RAPM, Peiris M, El Bushra HE, et al. Transmissibility of MERS-CoV infection in closed setting, Riyadh, Saudi Arabia, 2015. Emerg Infect Dis. 2019 Oct [date cited]. https://doi.org/10.3201/eid2510.190130
“…..We hypothesize that the increased human-to-human transmission within villas resulted from the clustering of the women’s activities. For example, the same women who lived together typically ate and socialized together, worked together, and traveled to and from work together. These activities added to the likelihood of intense direct physical contact among the women and probably facilitated limited but effective human-to-human transmission within their residence.….”
WHO reviews the current state of MERS-CoV
Saturday, August 10th, 2019WHO MERS Global Summary and Assessment of Risk
“…..Between 2012 and 30 June 2019, 2449 laboratory confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection were reported to WHO, of which 84.0% were reported by the Kingdom of Saudi Arabia.
In total, cases have been reported from 27 countries in the Middle East, North Africa, Europe, the United States of America, and Asia. Males above the age of 60 with an underlying medical conditions, such as diabetes, hypertension and renal failure, are at a higher risk of severe disease, including death. To date, 845 individuals have died (crude CFR 34.5%).
Since the last global update published on 30 June 2018, 219 laboratory-confirmed cases of MERS-CoV from four countries were reported to WHO (204 from Saudi Arabia, 13 from Oman, 1 from the Republic of Korea, and 1 from the United Kingdom), of whom 53 (24.2%) have died. Among these cases, 79.0% were male and the median age was 52 years old (IQR 39-65; range 16-94 years old). The median age is similar to the median age of all cases reported to WHO since 2012 (52 years old, IQR 37-65).
At the time of writing, 49 of the 219 (22.4%) patients were reported as asymptomatic or having mild disease. At least one underlying condition was reported in 145 cases (66.2%) since the last update, including chronic renal failure, heart disease, diabetes mellitus, and hypertension…….”
MERS-CoV is known to spread more easily in healthcare settings
Thursday, August 8th, 2019“……Over the past year, a cluster of 61 cases in Wadi ad-Dawasir in February and March sickened 61 people, 14 of them health workers. The outbreak involved six healthcare facilities, and human-to-human spread occurred in two of them. Then in April, one of two unlinked clusters in Khafji resulted in 10 cases, 5 of them involving healthcare workers……
The main epidemiologic pattern for MERS-CoV (Middle East respiratory syndrome coronavirus) remains the same—many introductions from dromedary camels in the Middle East and secondary transmission in healthcare settings, the WHO said. Household transmission among close family members is still limited for unknown reasons, but healthcare-associated outbreaks in the region are occurring more often, are typically small, and can affect several hospitals…..”
Results from the world’s first phase 1 trial of a vaccine against MERS-CoV (Middle East respiratory syndrome coronavirus) demonstrated a strong immune response after two doses and a good safety profile.
Friday, July 26th, 2019“…..Between Feb 17 and July 22, 2016, we enrolled 75 individuals and allocated 25 each to 0·67 mg, 2 mg, or 6 mg GLS-5300. No vaccine-associated serious adverse events were reported. The most common adverse events were injection-site reactions, reported in 70 participants (93%) of 75.
Overall, 73 participants (97%) of 75 reported at least one solicited adverse event; the most common systemic symptoms were headache (five [20%] with 0·67 mg, 11 [44%] with 2 mg, and seven [28%] with 6 mg), and malaise or fatigue (five [20%] with 0·67 mg, seven [28%] with 2 mg, and two [8%] with 6 mg). The most common local solicited symptoms were administration site pain (23 [92%] with all three doses) and tenderness (21 [84%] with all three doses). Most solicited symptoms were reported as mild (19 [76%] with 0·67 mg, 20 [80%] with 2 mg, and 17 [68%] with 6 mg) and were self-limiting. Unsolicited symptoms were reported for 56 participants (75%) of 75 and were deemed treatment-related for 26 (35%). The most common unsolicited adverse events were infections, occurring in 27 participants (36%); six (8%) were deemed possibly related to study treatment. There were no laboratory abnormalities of grade 3 or higher that were related to study treatment; laboratory abnormalities were uncommon, except for 15 increases in creatine phosphokinase in 14 participants (three participants in the 0·67 mg group, three in the 2 mg group, and seven in the 6 mg group). Of these 15 increases, five (33%) were deemed possibly related to study treatment (one in the 2 mg group and four in the 6 mg group).
Seroconversion measured by S1-ELISA occurred in 59 (86%) of 69 participants and 61 (94%) of 65 participants after two and three vaccinations, respectively. Neutralising antibodies were detected in 34 (50%) of 68 participants. T-cell responses were detected in 47 (71%) of 66 participants after two vaccinations and in 44 (76%) of 58 participants after three vaccinations. There were no differences in immune responses between dose groups after 6 weeks. At week 60, vaccine-induced humoral and cellular responses were detected in 51 (77%) of 66 participants and 42 (64%) of 66, respectively. ……”
Since 2012, Middle East respiratory syndrome (MERS) coronavirus has infected 2,442 persons and killed 842 worldwide.
Tuesday, July 9th, 2019Donnelly CA, Malik MR, Elkholy A, Cauchemez S, Van Kerkhove MD. Worldwide reduction in MERS cases and deaths since 2016. Emerg Infect Dis. 2019 Sep [date cited]. https://doi.org/10.3201/eid2509.190143