Archive for the ‘CDC’ Category
CDC: During week 51 (December 17-23, 2017), influenza activity increased sharply in the United States.
Saturday, December 30th, 2017During week 51 (December 17-23, 2017), influenza activity increased sharply in the United States.
- Viral Surveillance: The most frequently identified influenza virus subtype reported by public health laboratories during week 51 was influenza A(H3). The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased.
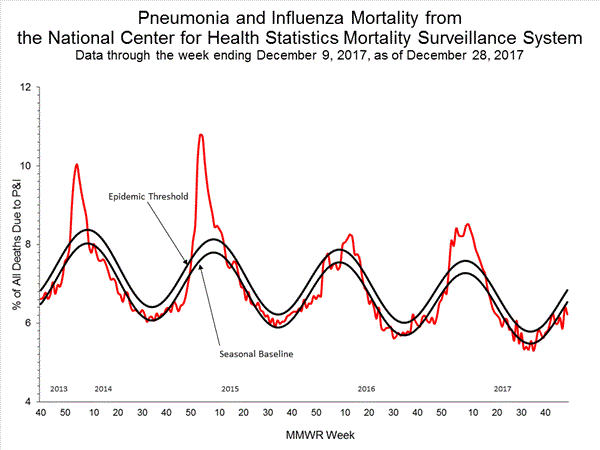
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
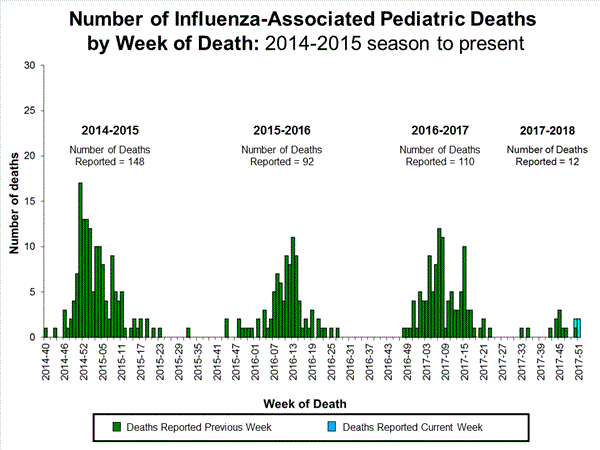
- Influenza-associated Pediatric Deaths: Three influenza-associated pediatric deaths were reported.
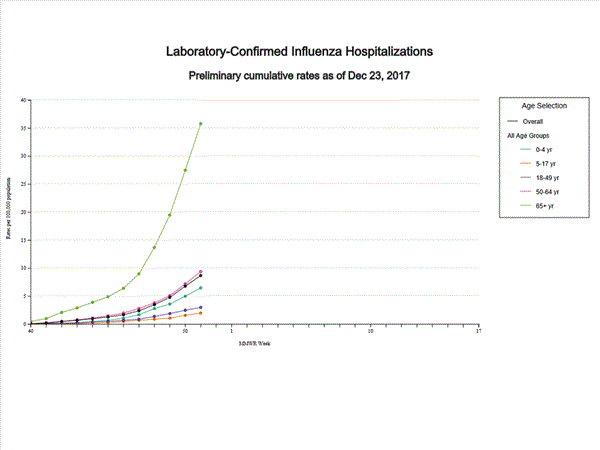
- Influenza-associated Hospitalizations: A cumulative rate of 8.7 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) was 5.0%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above region-specific baseline levels. Twenty-one states experienced high ILI activity; New York City and five states experienced moderate ILI activity; eight states experienced low ILI activity; 14 states experienced minimal ILI activity; and the District of Columbia, Puerto Rico and two states had insufficient data.
- Geographic Spread of Influenza:The geographic spread of influenza in 36 states was reported as widespread; Puerto Rico and 13 states reported regional activity; one state reported local activity; and the District of Columbia, the U.S. Virgin Islands, and Guam did not report.
CDC on hepatitis
Sunday, November 26th, 2017Viral hepatitis is the term that describes inflammation of the liver that is caused by a virus. There are actually five types of hepatitis viruses; each one is named after a letter in the alphabet: A, B, C, D and E.
The most common types of viral hepatitis are A, B and C. These three viruses affect millions of people worldwide, causing both short-term illness and long-term liver disease. The World Health Organization estimates 325 million people worldwide are living with chronic hepatitis B or chronic hepatitis C. In 2015, 1.34 million died from viral hepatitis, a number that is almost equal to the number of deaths caused by tuberculosis and HIV combined.
Hepatitis B and hepatitis C are the most common types of viral hepatitis in the United States, and can cause serious health problems, including liver failure and liver cancer. In the U.S., an estimated 3.5 million people are living with hepatitis C in the US and an estimated 850,000 are living with Hepatitis B. Unfortunately, new liver cancer cases and deaths are on the rise in the United States. This increase is believed to be related to infection with hepatitis B or hepatitis C.
Many people are unaware that they have been infected with hepatitis B and hepatitis C, because many people do not have symptoms or feel sick. CDC developed an online Hepatitis Risk Assessment to help determine if you should get tested or vaccinated for viral hepatitis. The assessment takes only five minutes and will provide personalized testing and vaccination recommendations for hepatitis A, hepatitis B, and hepatitis C.
Hepatitis A
Hepatitis A is a short-term disease caused by infection with the hepatitis A virus. Hepatitis A is usually spread when a person ingests the virus from contact with objects, food, or drinks contaminated by solid waste from an infected person. Hepatitis A was once very common in the United States, but now less than 3,000 cases are estimated to occur every year. Hepatitis A does not lead to liver cancer and most people who get infected recover over time with no lasting effects. However, the disease can be fatal for people in poor health or with certain medical conditions.
Hepatitis A is easily prevented with a safe and effective vaccine, which is believed to have caused the dramatic decline in new cases in recent years. The vaccine is recommended for all children at one year of age and for adults who may be at risk, including people traveling to certain international countries.
Hepatitis B
Hepatitis B is a liver disease that results after infection with the hepatitis B virus. Hepatitis B is common in many parts of the world, including Asia, the Pacific Islands and Africa. Like Hepatitis A, Hepatitis B is also preventable with a vaccine. The hepatitis B virus can be passed from an infected woman to her baby at birth, if her baby does not receive the hepatitis B vaccine. As a result, the hepatitis B vaccine is recommended for all infants at birth.
Unfortunately, many people got infected with hepatitis B before the vaccine was widely available. This is why CDC recommends anyone born in areas where hepatitis B is common, or who have parents who were born in these regions, get tested for hepatitis B. Treatments are available that can delay or reduce the risk of developing liver cancer.
Hepatitis C
Hepatitis C is a liver disease that results from infection with the hepatitis C virus. For reasons that are not entirely understood, people born from 1945 to 1965 are five times more likely to have hepatitis C than other age groups. In the past, hepatitis C was spread through blood transfusions and organ transplants. However, widespread screening of the blood supply in the United States began in 1990.The hepatitis C virus was virtually eliminated from the blood supply by 1992. Today, most people become infected with hepatitis C by sharing needles, syringes, or any other equipment to inject drugs. In fact, rates of new infections have been on the rise since 2010 in young people who inject drugs.
There is currently no vaccine to prevent hepatitis C. Fortunately, new treatments offer a cure for most people. Once diagnosed, most people with hepatitis C can be cured in just 8 to 12 weeks, which reduces their risk for liver cancer.
Find out if you should get tested or vaccinated for viral hepatitis by taking CDC’s quick online Hepatitis Risk Assessment.
For more information visit www.cdc.gov/hepatitis.
Stay Connected
- Join the conversation on hepatitis by following @cdchep on Twitter.
- Sign up for email updates from CDC’s Division of Viral Hepatitis.
Learn more
Everyone Needs Somewhere to Go: World Toilet Day (11/19/17)
Sunday, November 19th, 2017We use toilets every day – at home, school, and work – yet 40% of the world’s population does not have this luxury. Clean and safe toilets are more than just a place to use the restroom. They are essential for health, human dignity, and improved education. Sadly, 2.3 billion people lack even a basic sanitation service, which in many ways represents an ongoing public health crisis that puts much of the world’s population at risk for diseases such as cholera, dysentery, hepatitis, and typhoid fever. Almost 1 billion face the indignity every day of defecating outside without privacy. The 2015 Sustainable Development Goals include a target to ensure universal access to adequate and equitable sanitation and use of safely managed sanitation services by 2030, making sanitation a global development priority. To raise awareness of this issue, the United Nations General Assembly designated November 19 as World Toilet Day.
The Center for Global Health’s Emergency Response and Recovery Branch (ERRB), with support from the National Center for Emerging and Zoonotic Infectious Diseases’ Waterborne Disease Prevention Branch (WDPB), joined the United Nations and other development partners to reach the Sustainable Development Goal by evaluating the safety and acceptability of urine-diverting dry toilets (UDDTs). These types of toilets collect feces (poop) and urine separately for treatment, and because they are installed above ground, they are appropriate for areas where traditional options (e.g., dug pit latrines) are not feasible. This increases the potential for access to clean and safe toilets in difficult environments, such as flood-prone or dry areas.
In 2014, CDC was awarded a grant from Research for Health in Humanitarian Crises (R2HC), an organization working to improve health outcomes by strengthening the evidence for health interventions in humanitarian crises. This grant funds a study of UDDTs in a refugee camp setting to provide guidance on their potential use in humanitarian crises.

WDPB is also involved in efforts to improve sanitation by partnering with a start-up company, Sanivation, to provide in-home container-based urine-diverting toilets to households and to collect and turn the feces into fuel. In 2013, Sanivation received a CDC Innovation Fund Award to begin this waste-to-fuel conversion project in Kenya. Sanivation uses concentrated solar heat to treat the waste and make it safe; then the mix the treated waste with charcoal dust from agricultural waste and transform it into briquettes that widely used for cooking. This method of waste treatment has worked in refugee camp settings and provides a cost-effective and environmentally friendly way to reuse human waste. The project has been so successful, that in 2017, Sanivation received a special CDC Innovation Fund Award to scale-up their waste collection and treatment activities beyond its household subscribers. This new award will enable Sanivation to collect and treat waste from overflowing latrines, leaking septic tanks and other unsafely managed sanitation systems throughout the community, and to expand from one ton of waste collected and treated per month to over four tons. Ultimately, Sanivation plans to expand to other regions of East Africa with the goal of serving over 1 million people by 2020.
Through these efforts, CDC is working to increase the evidence base needed to provide clean and safe toilets and safely managed sanitation services in developing countries with limited resources. CDC’s efforts to improve sanitation are part of a worldwide initiative to break the silence surrounding the sanitation crisis.
To learn more about CDC efforts and other current sanitation initiatives visit:
Multistate Outbreak of Multidrug-Resistant Salmonella Heidelberg Infections Linked to Contact with Dairy Calves
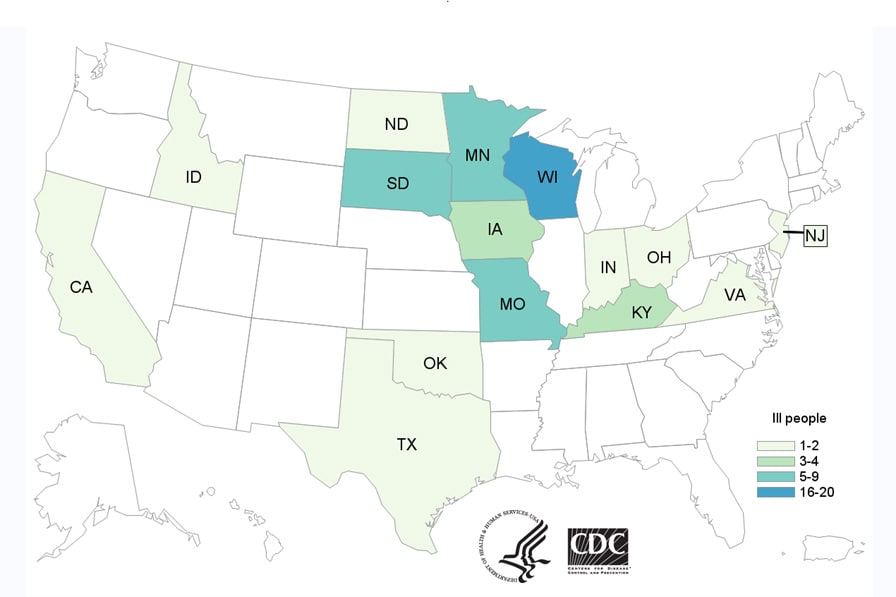
Friday, November 17th, 2017Since the last update on August 2, 2017, eight more ill people have been reported from six states.
- CDC, several states, and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) are investigating a multistate outbreak of multidrug-resistant Salmonella Heidelberg infections.
- A total of 54 people infected with the outbreak strains of Salmonella Heidelberg have been reported from 15 states.
- Seventeen (35%) people have been hospitalized. No deaths have been reported.
- Illnesses started on dates ranging from January 27, 2015 to October 15, 2017.
- Eighteen (33%) people in this outbreak are children under the age of 5.
- Epidemiologic and laboratory investigations linked ill people in this outbreak to contact with calves, including dairy calves.
- In interviews, ill people answered questions about contact with animals and foods eaten in the week before becoming ill. Of the 54 people interviewed, 34 (63%) reported contact with dairy calves or other cattle. Some of the ill people interviewed reported that they became sick after their dairy calves became sick or died.
- Ongoing surveillance in veterinary diagnostic laboratories showed that calves in several states continue to get sick with the outbreak strains of multidrug resistant Salmonella Heidelberg.
- Information collected earlier in the outbreak indicated that most of the calves came from Wisconsin. Regulatory officials in several states are now tracing the origin of the calves that are linked to the newer illnesses.
- Antibiotic resistance testing(https://www.cdc.gov/narms/resources/glossary.html) conducted by CDC on clinical isolates from ill people shows that the isolates were resistant to multiple types of antibiotics.
- Antibiotic resistance may be associated with increased risk of hospitalization, development of a bloodstream infection, or treatment failure in patients.
- Whole genome sequencing has identified multiple antimicrobial resistance genes in outbreak-associated isolates from 43 ill people, 87 isolates from cattle, and 11 isolates from animal environments.
- These findings match results from standard antibiotic resistance testing(https://www.cdc.gov/narms/resources/glossary.html) methods used by CDC’s National Antimicrobial Resistance Monitoring System (NARMS)(https://www.cdc.gov/narms/index.html) laboratory on clinical isolates from eight ill people in this outbreak.
- All eight isolates from ill people were resistant to amoxicillin-clavulanic acid, ampicillin, cefoxitin, ceftriaxone, streptomycin, sulfisoxazole, and tetracycline, and had reduced susceptibility to ciprofloxacin. Seven isolates were also resistant to trimethoprim-sulfamethoxazole. Five were also resistant to nalidixic acid. Three were also resistant to chloramphenicol. All eight isolates tested were susceptible to azithromycin and meropenem.
- Follow these steps to prevent illness when working with any livestock:
- Always wash your hands thoroughly with soap and water right after touching livestock, equipment, or anything in the area where animals live and roam. Use dedicated clothes, shoes, and work gloves when working with livestock. Keep and store these items outside of your home.
- It is especially important to follow these steps if there are children under age 5 in your household. Young children are more likely to get a Salmonella infection because their immune systems are still developing.
- Work with your veterinarian to keep your animals healthy and prevent diseases.
- This investigation is ongoing and we will provide updates as more information becomes available. Livestock owners should continue to watch for increased sicknesses in dairy calves and consult their veterinarian if needed.
CDC recommendations to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas during the period of September 2017 – March 2018.
Wednesday, October 25th, 2017Advice for Providers Treating Patients in or Recently Returned from Hurricane-Affected Areas, Including Puerto Rico and US Virgin Islands
Distributed via the CDC Health Alert Network
October 24, 2017, 1330 ET (1:30 PM ET)
CDCHAN-00408
Summary
The Centers for Disease Control and Prevention (CDC) is working with federal, state, territorial, and local agencies and global health partners in response to recent hurricanes. CDC is aware of media reports and anecdotal accounts of various infectious diseases in hurricane-affected areas, including Puerto Rico and the US Virgin Islands (USVI). Because of compromised drinking water and decreased access to safe water, food, and shelter, the conditions for outbreaks of infectious diseases exist.
The purpose of this HAN advisory is to remind clinicians assessing patients currently in or recently returned from hurricane-affected areas to be vigilant in looking for certain infectious diseases, including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. Additionally, this Advisory provides guidance to state and territorial health departments on enhanced disease reporting.
Background
Hurricanes Irma and Maria made landfall in Puerto Rico and USVI in September 2017, causing widespread flooding and devastation. Natural hazards associated with the storms continue to affect many areas. Infectious disease outbreaks of diarrheal and respiratory illnesses can occur when access to safe water and sewage systems are disrupted and personal hygiene is difficult to maintain. Additionally, vector borne diseases can occur due to increased mosquito breeding in standing water; both Puerto Rico and USVI are at risk for outbreaks of dengue, Zika, and chikungunya.
Health care providers and public health practitioners should be aware that post-hurricane environmental conditions may pose an increased risk for the spread of infectious diseases among patients in or recently returned from hurricane-affected areas; including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. The period of heightened risk may last through March 2018, based on current predictions of full restoration of power and safe water systems in Puerto Rico and USVI.
In addition, providers in health care facilities that have experienced water damage or contaminated water systems should be aware of the potential for increased risk of infections in those facilities due to invasive fungi, nontuberculous Mycobacterium species, Legionella species, and other Gram-negative bacteria associated with water (e.g., Pseudomonas), especially among critically ill or immunocompromised patients.
Cholera has not occurred in Puerto Rico or USVI in many decades and is not expected to occur post-hurricane.
Recommendations
These recommendations apply to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas (e.g., within the past 4 weeks), during the period of September 2017 – March 2018.
- Health care providers and public health practitioners in hurricane-affected areas should look for community and healthcare-associated infectious diseases.
- Health care providers in the continental US are encouraged to ask patients about recent travel (e.g., within the past 4 weeks) to hurricane-affected areas.
- All healthcare providers should consider less common infectious disease etiologies in patients presenting with evidence of acute respiratory illness, gastroenteritis, renal or hepatic failure, wound infection, or other febrile illness. Some particularly important infectious diseases to consider include leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza.
- In the context of limited laboratory resources in hurricane-affected areas, health care providers should contact their territorial or state health department if they need assistance with ordering specific diagnostic tests.
- For certain conditions, such as leptospirosis, empiric therapy should be considered pending results of diagnostic tests— treatment for leptospirosis is most effective when initiated early in the disease process. Providers can contact their territorial or state health department or CDC for consultation.
- Local health care providers are strongly encouraged to report patients for whom there is a high level of suspicion for leptospirosis, dengue, hepatitis A, typhoid, and vibriosis to their local health authorities, while awaiting laboratory confirmation.
- Confirmed cases of leptospirosis, dengue, hepatitis A, typhoid fever, and vibriosis should be immediately reported to the territorial or state health department to facilitate public health investigation and, as appropriate, mitigate the risk of local transmission. While some of these conditions are not listed as reportable conditions in all states, they are conditions of public health importance and should be reported.
For More Information
- General health information about hurricanes and other tropical storms: https://www.cdc.gov/disasters/hurricanes/index.html
- Information about Hurricane Maria: https://www.cdc.gov/disasters/hurricanes/hurricane_maria.html
- Information for Travelers:
- Travel notice for Hurricanes Irma and Maria in the Caribbean: https://wwwnc.cdc.gov/travel/notices/alert/hurricane-irma-in-the-caribbean
- Health advice for travelers to Puerto Rico: https://wwwnc.cdc.gov/travel/destinations/traveler/none/puerto-rico?s_cid=ncezid-dgmq-travel-single-001
- Health advice for travelers to the U.S. Virgin Islands: https://wwwnc.cdc.gov/travel/destinations/traveler/none/usvirgin-islands?s_cid=ncezid-dgmq-travel-leftnav-traveler
- Resources from CDC Health Information for International Travel 2018 (the Yellow Book):
- Post-travel Evaluation: https://wwwnc.cdc.gov/travel/yellowbook/2018/post-travel-evaluation/general-approach-to-the-returned-traveler
- Information about infectious diseases after a disaster: https://www.cdc.gov/disasters/disease/infectious.html
- Dengue: https://www.cdc.gov/dengue/index.html
- Hepatitis A: https://www.cdc.gov/hepatitis/HAV/index.htm
- Leptospirosis: https://www.cdc.gov/leptospirosis/
- Typhoid fever: https://www.cdc.gov/typhoid-fever/index.html
- Vibriosis: https://www.cdc.gov/vibrio/index.html
- Information about other infectious diseases of concern:
- Conjunctivitis: https://www.cdc.gov/conjunctivitis/
- Influenza: https://www.cdc.gov/flu/index.htm
- Scabies: https://www.cdc.gov/parasites/scabies/index.html
- Tetanus and wound management: https://www.cdc.gov/disasters/emergwoundhcp.html
- Tetanus in Areas Affected by a Hurricane: Guidelines for Clinicians https://emergency.cdc.gov/coca/cocanow/2017/2017sept12.asp
Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2017–18 Influenza Season
Saturday, September 23rd, 2017Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2017–18 Influenza Season
Recommendations and Reports / August 25, 2017 / 66(2);1–20
Lisa A. Grohskopf, MD1; Leslie Z. Sokolow, MSc, MPH1,2; Karen R. Broder, MD3; Emmanuel B. Walter, MD4; Joseph S. Bresee, MD1; Alicia M. Fry, MD1; Daniel B. Jernigan, MD1
Summary
This report updates the 2016–17 recommendations of the Advisory Committee on Immunization Practices (ACIP) regarding the use of seasonal influenza vaccines (MMWR Recomm Rep 2016;65[No. RR-5]). Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications. A licensed, recommended, and age-appropriate vaccine should be used.
For the 2017–18 season, quadrivalent and trivalent influenza vaccines will be available. Inactivated influenza vaccines (IIVs) will be available in trivalent (IIV3) and quadrivalent (IIV4) formulations. Recombinant influenza vaccine (RIV) will be available in trivalent (RIV3) and quadrivalent (RIV4) formulations. Live attenuated influenza vaccine (LAIV4) is not recommended for use during the 2017–18 season due to concerns about its effectiveness against (H1N1)pdm09 viruses during the 2013–14 and 2015–16 seasons. Recommendations for different vaccine types and specific populations are discussed. No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one licensed, recommended product is available.
Updates to the recommendations described in this report reflect discussions during public meetings of ACIP held on October 20, 2016; February 22, 2017; and June 21, 2017. New and updated information in this report includes the following:
- Vaccine viruses included in the 2017–18 U.S. trivalent influenza vaccines will be an A/Michigan/45/2015 (H1N1)pdm09–like virus, an A/Hong Kong/4801/2014 (H3N2)-like virus, and a B/Brisbane/60/2008–like virus (Victoria lineage). Quadrivalent influenza vaccines will contain these three viruses and an additional influenza B vaccine virus, a B/Phuket/3073/2013–like virus (Yamagata lineage).
- Information on recent licensures and labelling changes is discussed, including licensure of Afluria Quadrivalent (IIV4; Seqirus, Parkville, Victoria, Australia); Flublok Quadrivalent (RIV4; Protein Sciences, Meriden, Connecticut); and expansion of the age indication for FluLaval Quadrivalent (IIV4; ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada), previously licensed for ≥3 years, to ≥6 months.
- Pregnant women may receive any licensed, recommended, age-appropriate influenza vaccine.
- Afluria (IIV3; Seqirus, Parkville, Victoria, Australia) may be used for persons aged ≥5 years, consistent with Food and Drug Administration–approved labeling.
- FluMist Quadrivalent (LAIV4; MedImmune, Gaithersburg, Maryland) should not be used during the 2017–18 season due to concerns about its effectiveness against influenza A(H1N1)pdm09 viruses in the United States during the 2013–14 and 2015–16 influenza seasons.
This report focuses on the recommendations for use of vaccines for the prevention and control of influenza during the 2017–18 season in the United States. A Background Document containing further information and a summary of these recommendations are available at https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/flu.html. These recommendations apply to licensed influenza vaccines used within Food and Drug Administration–licensed indications, including those licensed after the publication date of this report. Updates and other information are available at CDC’s influenza website (https://www.cdc.gov/flu). Vaccination and health care providers should check CDC’s influenza website periodically for additional information.
Introduction
Influenza viruses typically circulate widely in the United States annually, from the late fall through the early spring. Although most persons with influenza will recover without sequelae, influenza can cause serious illness and death, particularly among older adults, very young children, pregnant women, and those with certain chronic medical conditions (1–6).
Routine annual influenza vaccination for all persons aged ≥6 months who do not have contraindications has been recommended by CDC and CDC’s Advisory Committee on Immunization Practices (ACIP) since 2010 (7). This report updates the 2016–17 ACIP recommendations regarding the use of seasonal influenza vaccines (8) and provides recommendations and guidance for vaccine providers regarding the use of influenza vaccines for the 2017–18 season. A variety of different formulations of influenza vaccine are available (Table 1). Contraindications and precautions to the use of influenza vaccines are summarized (Table 2). Abbreviations are used in this report to denote the various types of vaccines (Box).
This report focuses on the recommendations for use of influenza vaccines for the prevention and control of influenza during the 2017–18 season in the United States. A summary of these recommendations and a Background Document containing additional information on influenza-associated illnesses and influenza vaccines are available at https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/flu.html.
Methods
ACIP provides annual recommendations for the use of influenza vaccines for the prevention and control of influenza. The ACIP Influenza Work Group meets by teleconference once to twice per month throughout the year. Work Group membership includes several voting members of ACIP and representatives of ACIP Liaison Organizations.* Discussions include topics such as influenza surveillance, vaccine effectiveness and safety, vaccine coverage, program feasibility, cost-effectiveness, and vaccine supply. Presentations are requested from invited experts, and published and unpublished data are discussed.
In general, the Background Document is updated to reflect recent additions to the literature related to the following: 1) recommendations that were made in previous seasons, 2) changes in the viral antigen composition of seasonal influenza vaccines, and 3) minor changes in guidance for the use of influenza vaccines (e.g., guidance for timing of vaccination and other programmatic issues, guidance for dosage in specific populations, guidance for selection of vaccines for specific populations that are already recommended for vaccination, and changes that reflect use consistent with Food and Drug Administration [FDA]–licensed indications and prescribing information). The summary included in the Background Document for such topics is not a systematic review, but is intended to provide a broad overview of current literature. In general, systematic review and evaluation of the evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach is performed for new recommendations or substantial changes in the recommendations (e.g., expansion of the recommendation for influenza vaccination to new populations not previously recommended for vaccination or potential preferential recommendations for specific vaccines).
Updates and changes to the recommendations described in this report are of five types: 1) the vaccine virus composition for 2017–18 U.S. seasonal influenza vaccines; 2) recent regulatory actions, including new vaccine licensures and labeling changes for previously licensed vaccines; 3) updated recommendations for the use of influenza vaccines in pregnancy, including a recommendation that pregnant women may receive any licensed, recommended, age-appropriate influenza vaccine; 4) a recommendation that the trivalent inactivated influenza vaccine (IIV3) Afluria (Seqirus, Parkville, Victoria, Australia) may be used for persons aged ≥5 years, consistent with FDA-approved labeling; and 5) a recommendation (continued from the 2016–17 season) that LAIV4 not be used during the 2017–18 season. Systematic review and GRADE were not performed for these updates and changes. Information relevant to these changes includes the following:
- Recommendations for composition of Northern Hemisphere influenza vaccines are made by the World Health Organization (WHO), which organizes a consultation, generally in February of each year. Surveillance data are reviewed and candidate vaccine viruses are discussed. A summary of the WHO meeting for selection of the 2017–18 Northern Hemisphere vaccine viruses is available at http://www.who.int/influenza/vaccines/virus/recommendations/201703_recommendation.pdf. Subsequently, FDA, which has regulatory authority over vaccines in the United States, convenes a meeting of its Vaccines and Related Biological Products Advisory Committee (VRBPAC). This committee considers the recommendations of WHO, reviews and discusses similar data, and makes a final decision regarding vaccine virus composition for influenza vaccines licensed and marketed in the United States. A summary of the FDA VRBPAC meeting of March 9, 2017, at which the composition of the 2017–18 U.S. influenza vaccines was discussed, is available at https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/BloodVaccinesandOtherBiologics/VaccinesandRelatedBiologicalProductsAdvisoryCommittee/UCM552054.pdf.
- With regard to recommendations for newly licensed influenza vaccines and changes to the licensed indications for existing vaccines, ACIP relies on FDA for review of safety, immunogenicity, and effectiveness data pertaining to the licensure of influenza vaccines. Regulatory information pertinent to the two recently licensed products and one labelling change discussed in this report is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm518291.htm (for Afluria Quadrivalent; Seqirus, Parkville, Victoria, Australia), https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm524660.htm (for Flublok Quadrivalent; Protein Sciences, Meriden, Connecticut), and https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm366061.htm (for FluLaval Quadrivalent; ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada).
- For the recommendation that pregnant women may receive any licensed, recommended, and age-appropriate influenza vaccine, because there have been no studies evaluating use of RIV3 or RIV4 in pregnancy, ACIP reviewed available information presented by the manufacturer and summarized in public documents by FDA concerning pregnancies that occurred among women participating in studies of RIV and pregnancy registry data. RIV reports to the Vaccine Adverse Event Reporting System (VAERS) also were presented. Regulatory information pertinent to this discussion is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm524660.htm.
- For the recommendation that Afluria (IIV3; Seqirus, Parkville, Victoria, Australia) may be used for persons aged ≥5 years, ACIP reviewed data from studies performed by the manufacturer concerning the cause of an increase in the rate of febrile seizures that occurred in association with the 2010 Southern Hemisphere formulation of this product, and resulting changes in the vaccine manufacturing process. This change makes the ACIP recommendation consistent with FDA-approved labelling for this product. Minutes of the ACIP presentation of these data are available at https://www.cdc.gov/vaccines/acip/meetings/downloads/min-archive/min-2017-02.pdf. Regulatory information is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094043.htm.
- The recommendation that LAIV4 not be used due to concerns regarding its effectiveness against influenza A(H1N1)pdm09 viruses during the 2013–14 and 2015–16 U.S. seasons was initially made for the 2016–17 season (9). This recommendation continues to be made for the 2017–18 season. ACIP will continue to review data concerning LAIV4 as they become available.
Primary Changes and Updates in the Recommendations
Routine annual influenza vaccination of all persons aged ≥6 months without contraindications continues to be recommended. No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one licensed, recommended product is available. Updated information and guidance in this report includes the following:
- 2017–18 U.S. trivalent influenza vaccines will contain an A/Michigan/45/2015 (H1N1)pdm09–like virus, an A/Hong Kong/4801/2014 (H3N2)–like virus and a B/Brisbane/60/2008–like virus (Victoria lineage). Quadrivalent vaccines will include an additional vaccine virus strain, a B/Phuket/3073/2013–like virus (Yamagata lineage). This represents a change in the influenza A(H1N1)pdm09 virus component from the previous season.
- Recent regulatory actions, including two new licensures and one labelling change are described:
- Afluria Quadrivalent (IIV4; Seqirus, Parkville, Victoria, Australia) was licensed by FDA in August, 2016 for persons aged ≥18 years. Regulatory information is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm518291.htm.
- Flublok Quadrivalent (RIV4; Protein Sciences, Meriden, Connecticut) was licensed by FDA in October 2016, for persons aged ≥18 years. Regulatory information is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm524660.htm.
- The age indication for FluLaval Quadrivalent (IIV4; ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada) was extended from ≥3 years to ≥6 months in November 2016. Regulatory information is available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm366061.htm. Children aged 6 through 35 months may receive FluLaval Quadrivalent at the same 0.5 mL per dose (containing 15 µg of hemagglutinin [HA] per vaccine virus) as is used for older children and adults. This licensure creates an additional option for vaccination of children aged 6 through 35 months, in addition to the previously available 0.25 mL per dose presentation (containing 7.5 µg of HA per vaccine virus) of Fluzone Quadrivalent (IIV4; Sanofi Pasteur, Swiftwater, Pennsylvania).
- Pregnant women may receive any licensed, recommended, age-appropriate influenza vaccine.
- Afluria (IIV3; Seqirus, Parkville, Victoria, Australia) is now recommended for persons aged ≥5 years, consistent with FDA-approved labelling.
- In light of its low effectiveness against influenza A(H1N1)pdm09 in the United States during the 2013–14 and 2015–16 seasons, for the 2017–18 season, ACIP continues the recommendation that LAIV4 should not be used. Because LAIV4 is still a licensed vaccine that might be available and that some providers might elect to use, for informational purposes only, reference is made in this report to previous recommendations for its use.
Recommendations for the Use of Influenza Vaccines, 2017–18 Season
Groups Recommended for Vaccination
Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications. Recommendations regarding timing of vaccination, considerations for specific populations, the use of specific vaccines, and contraindications and precautions are summarized in the sections that follow.
Timing of Vaccination
Optimally, vaccination should occur before onset of influenza activity in the community. Health care providers should offer vaccination by the end of October, if possible. Children aged 6 months through 8 years who require 2 doses (see Children Aged 6 Months through 8 Years) should receive their first dose as soon as possible after vaccine becomes available, to allow the second dose (which must be administered ≥4 weeks later) to be received by the end of October. Although some available data indicate that early vaccination (e.g., in July and August) might be associated with suboptimal immunity before the end of the influenza season, particularly among older adults, the relative contribution of potential waning of immunity compared with those of other determinants of the impact of vaccination (e.g., timing and severity of the influenza season, the impact of missed opportunities when individuals delay vaccination and fail to return later in the season, and programmatic constraints) is unknown. Although delaying vaccination might result in greater immunity later in the season, deferral also might result in missed opportunities to vaccinate, as well as difficulties in vaccinating a population within a more constrained time period. Community vaccination programs should balance maximizing likelihood of persistence of vaccine-induced protection through the season with avoiding missed opportunities to vaccinate or vaccinating after onset of influenza circulation occurs. Revaccination later in the season of persons who have already been fully vaccinated is not recommended.
Vaccination should continue to be offered as long as influenza viruses are circulating and unexpired vaccine is available. To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations when vaccine is available. Vaccination efforts should be structured to ensure the vaccination of as many persons as possible before influenza activity in the community begins.
In any given season, the optimal time to vaccinate cannot be predicted precisely because influenza seasons vary in timing and duration. Moreover, more than one outbreak might occur in a given community in a single year. In the United States, localized outbreaks that indicate the start of seasonal influenza activity can occur as early as October. However, in 74% of influenza seasons from 1982–83 through 2015–16, peak influenza activity (which often is close to the midpoint of influenza activity for the season) has not occurred until January or later, and in 59% of seasons, the peak was in February or later (10).
In recent seasons, initial shipments of influenza vaccine have arrived to some vaccine providers as early as July. Very early availability of vaccine as compared with typical onset and peak of influenza activity raises questions related to the ideal time to begin vaccination. Several observational studies of influenza vaccine effectiveness have reported decreased vaccine protection within a single season, particularly against influenza A(H3N2) (11–14). In some of these studies decline in VE was particularly pronounced among older adults (12,13). Some studies have documented decline in protective antibodies over the course of one season (15–17), with antibody levels decreasing with greater time elapsed postvaccination. However, the rate and degree of decline observed has varied. Among adults in one study, HA and neuraminidase antibody levels declined slowly, with a two-fold decrease in titer estimated to take >600 days (18). A review of studies reporting postvaccination seroprotection rates among adults aged ≥60 years noted that seroprotection levels meeting Committee of Proprietary Medicinal Products standards were maintained for ≥4 months for the H3N2 component in all 8 studies and for the H1N1 and B components in five of seven studies (19). A recent multiseason analysis from the U.S. Influenza Vaccine Effectiveness (U.S. Flu VE) Network found that VE declined by about 7% per month for H3N2 and influenza B, and 6%–11% per month for H1N1pdm09 (20). VE remained greater than zero for at least 5 to 6 months after vaccination. Similar waning effects have not been observed consistently across age groups and virus subtypes in different populations, and the observed decline in protection could be attributable to bias, unmeasured confounding, or the late season emergence of antigenic drift variants that are less well-matched to the vaccine strain.
Vaccination efforts should continue throughout the season because the duration of the influenza season varies and influenza activity might not occur in certain communities until February or March. Providers should offer influenza vaccine routinely, and organized vaccination campaigns should continue throughout the influenza season, including after influenza activity has begun in the community. Although vaccination by the end of October is recommended, vaccine administered in December or later, even if influenza activity has already begun, is likely to be beneficial in the majority of influenza seasons.
Guidance for Use in Specific Populations and Situations
Populations at Higher Risk for Medical Complications Attributable to Severe Influenza
All persons aged ≥6 months without contraindications should be vaccinated annually. However, vaccination to prevent influenza is particularly important for persons who are at increased risk for severe complications from influenza and for influenza-related outpatient, ED, or hospital visits. When vaccine supply is limited, vaccination efforts should focus on delivering vaccination to the following persons at increased risk for medical complications attributable to severe influenza who do not have contraindications (no hierarchy is implied by order of listing):
- all children aged 6 through 59 months;
- all persons aged ≥50 years;
- adults and children who have chronic pulmonary (including asthma) or cardiovascular (except isolated hypertension), renal, hepatic, neurologic, hematologic, or metabolic disorders (including diabetes mellitus);
- persons who are immunocompromised due to any cause (including immunosuppression caused by medications or by HIV infection);
- women who are or will be pregnant during the influenza season;
- children and adolescents (aged 6 months through 18 years) who are receiving aspirin- or salicylate-containing medications and who might be at risk for experiencing Reye syndrome after influenza virus infection;
- residents of nursing homes and other long-term care facilities;
- American Indians/Alaska Natives; and
- persons who are extremely obese (BMI ≥40).
ACIP recommends that LAIV4 not be used during the 2017–18 season for any population. Providers who elect to use it should consider previous guidance for use of LAIV4 for high-risk populations (Table 2).
Persons Who Live With or Care for Persons at Higher Risk for Influenza-Related Complications
All persons aged ≥6 months without contraindications should be vaccinated annually; however, continued emphasis should be placed on vaccination of persons who live with or care for persons at higher risk for influenza-related complications. When vaccine supply is limited, vaccination efforts should focus on delivering vaccination to persons at higher risk for influenza-related complications listed above, as well as these persons:
- health care personnel, including physicians, nurses, and other workers in inpatient and outpatient-care settings, medical emergency-response workers (e.g., paramedics and emergency medical technicians), and employees of nursing home and long-term care facilities who have contact with patients or residents, and students in these professions who will have contact with patients. ACIP guidance for immunization of health care personnel has been published previously (21);
- household contacts (including children) and caregivers of children aged ≤59 months (i.e., aged <5 years) and adults aged ≥50 years, particularly contacts of children aged <6 months; and
- household contacts (including children) and caregivers of persons with medical conditions that put them at high risk for severe complications from influenza.
ACIP recommends that LAIV4 not be used during the 2017–18 season for any population. Providers who elect to use it should consider previous guidance for use of LAIV4 for persons who care for or have contact with immunocompromised persons (22). Health care personnel and persons who are contacts of persons in these groups and who are contacts of severely immunocompromised persons (those living in a protected environment) may receive any IIV or RIV that is otherwise indicated. ACIP and HICPAC have previously recommended that health care personnel who receive LAIV should avoid providing care for severely immunosuppressed patients requiring a protected environment for 7 days after vaccination, and that hospital visitors who have received LAIV4 should avoid contact with severely immunosuppressed persons (i.e., persons requiring a protected environment) for 7 days after vaccination. However, such persons should not be restricted from visiting less severely immunosuppressed patients.
Children Aged 6 Months Through 8 Years
Dose volume for children aged 6 through 35 months: Children aged 6 through 35 months may receive one of two products at the appropriate volume for each dose needed: 0.5 mL FluLaval Quadrivalent (containing 15 µg of HA per vaccine virus) or 0.25 mL Fluzone Quadrivalent (containing 7.5 µg of HA per vaccine virus). These are the only two influenza vaccine products licensed for this age group. Care should be taken to administer the appropriate volume for each needed dose of either product. In either instance, the needed volume may be administered from an appropriate prefilled syringe, a single dose vial, or multidose vial, as supplied by the manufacturer. Note, however, that if a 0.5 mL single-use vial of Fluzone Quadivalent is used for a child aged 6 through 35 months, only half the volume should be administered and the other half should be discarded.
Before November 2016, the only influenza vaccine formulations licensed for children aged 6 through 35 months were the 0.25 mL (containing 7.5 µg of HA per vaccine virus) dose formulations of Fluzone and Fluzone Quadrivalent. The recommendation for use of a reduced dose volume for children in this age group (half that recommended for persons aged ≥3 years) was based on increased reactogenicity noted among children (particularly younger children) following receipt of influenza vaccines in trials conducted during the 1970s. This increased reactogenicity was primarily observed with whole-virus inactivated vaccines (23–27). Studies with vaccines more similar to currently available split-virus inactivated products demonstrated less reactogenicity (27). Recent comparative studies of 0.5 mL vs. 0.25 mL doses of IIV3 conducted among children aged 6 through 23 months (28) and 6 through 35 months (29) noted no significant difference in reactogenicity at the higher dose. In a randomized trial comparing immunogenicity and safety of 0.5 mL FluLaval Quadrivalent with 0.25 mL Fluzone Quadrivalent, safety and reactogenicity were similar between the two vaccines. In a post-hoc analysis, superior immunogenicity was noted for the B components of FluLaval Quadrivalent among infants aged 6 through 17 months and for unprimed children (those who had not previously received at least 2 doses of influenza vaccine) aged 6 through 35 months (30).
Number of doses for children aged 6 months through 8 years: Evidence from several studies indicates that children aged 6 months through 8 years require 2 doses of influenza vaccine (administered a minimum of 4 weeks apart) during their first season of vaccination for optimal protection (31–34). Children aged 6 months through 8 years who have previously received ≥2 total doses of trivalent or quadrivalent influenza vaccine before July 1, 2017 require only 1 dose for 2017–18. The 2 doses of influenza vaccine do not have to have been administered in the same season or consecutive seasons. Children in this age group who have not previously received ≥2 doses of trivalent or quadrivalent influenza vaccine before July 1, 2017 require 2 doses for the 2017–18 season. The interval between the 2 doses should be at least 4 weeks (Figure).
Pregnant Women
Because pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant, ACIP recommends that all women who are pregnant or who might be pregnant in the influenza season receive influenza vaccine. Any licensed, recommended, and age-appropriate influenza vaccine may be used. Influenza vaccine can be administered at any time during pregnancy, before and during the influenza season. ACIP recommends that LAIV4 not be used in any population for the 2017–18 season. Providers should note that, as a live virus vaccine, LAIV4 should not be used during pregnancy.
Although experience with the use of IIVs is substantial, and data from observational studies are available to support the safety of these vaccines in pregnancy, data are more limited for vaccination during the first trimester (see Safety of Influenza Vaccines: Pregnant Women and Neonates in the Background Document). Moreover, there is substantially less experience with more recently licensed IIV products (e.g., quadrivalent, cell culture-based, and adjuvanted vaccines) during pregnancy in general. For RIV (available as RIV3 since the 2013–14 influenza season, and as RIV3 and RIV4 for 2017–18), data are limited to reports of pregnancies occurring incidentally during clinical trials, VAERS reports, and pregnancy registry reports. Pregnancy registries and surveillance studies exist for some products; information may be found in package inserts (35–42), available at https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094045.htm for trivalent vaccines and https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm295057.htm for quadrivalent vaccines.
Older Adults
For persons aged ≥65 years, any age-appropriate IIV formulation (standard-dose or high-dose, trivalent or quadrivalent, unadjuvanted or adjuvanted) or RIV are acceptable options. Fluzone High-Dose (HD-IIV3; Sanofi Pasteur, Swiftwater, Pennsylvania) met prespecified criteria for superior efficacy to that of SD-IIV3 in a randomized trial conducted over two seasons among 31,989 persons aged ≥65 years, and might provide better protection than SD-IIV3 for this age group (43–45). In an exploratory analysis of data from a single-season randomized trial conducted among 8,604 adults aged ≥50 years, Flublok Quadrivalent (RIV4; Protein Sciences, Meriden, Connecticut) was more efficacious than SD-IIV4 (46,47); however, no claim of superiority was approved for the package insert (47). Fluad (aIIV3; Seqirus, Holly Springs, North Carolina) was more effective against laboratory-confirmed influenza than unadjuvanted SD-IIV3 among adults aged ≥65 years (N = 227) in an analysis from a small observational study (48). No preferential recommendation is made for any specific vaccine product. Vaccination should not be delayed if a specific product is not readily available.
Because of the vulnerability of this population to severe influenza illness, hospitalization, and death, efficacy and effectiveness of influenza vaccines among older adults is an area of active research (see Immunogenicity, Efficacy, and Effectiveness of Influenza Vaccines: HD-IIV3, aIIV3, and RIV4 for Older Adults in the Background Document). Recent comparative studies of efficacy/effectiveness against laboratory-confirmed influenza outcomes among older adults have focused on HD-IIV3 (Fluzone High Dose; Sanofi Pasteur, Swiftwater, Pennsylvania) (43,49–51), aIIV3 (Fluad, Seqirus, Holly Springs, North Carolina) (48), and RIV4 (Flublok Quadrivalent; Protein Sciences, Meriden, Connecticut) (46). Characteristics of these studies are summarized (Table 3). In each instance, the comparator vaccines have been standard dose, inactivated vaccines (SD-IIV3 as the comparator for HD-IIV3 and aIIV3; SD-IIV4 as the comparator for RIV4). No data are yet available from studies comparing the efficacy or effectiveness of HD-IIV3, aIIV3, and RIV4 with one another among older adults. This lack of comparative data prevents recommending one of these three vaccines over another for this population. HD-IIV3 exhibited superior efficacy over a comparator standard-dose IIV3 for adults aged ≥65 years in a large (N = 31,989), two-season randomized, controlled, double-blind trial (43,44), and might provide better protection than SD-IIV3s for this age group. Additional data concerning relative efficacy of HD-IIV3 for other clinical outcomes, as well as cost-effectiveness analyses and observational studies, are summarized in the Background Document. In a single-season randomized, controlled, double-blind trial comparing RIV4 with a standard-dose unadjuvanted IIV4 among adults aged ≥50 years (N = 8,604), RIV4 was more effective; however, approval for a claim of superiority was not made as a result of this exploratory analysis (46,47). Additional data, including discussion of immunogenicity studies, are described in the Background Document. Fluad (aIIV3; Seqirus, Holly Springs, North Carolina) was more effective against laboratory-confirmed influenza than unadjuvanted SD-IIV3 among adults aged ≥65 years (N = 227) in an analysis from a small observational study (48); no data are yet available concerning efficacy of Fluad compared with nonadjuvanted IIV3 against laboratory-confirmed influenza outcomes from a randomized trial in this population. Additional data concerning aIIV3, from studies examining immunogenicity and non-laboratory confirmed influenza outcomes, are discussed in the Background Document. ACIP will continue to review data concerning the efficacy and effectiveness of these vaccines as more information emerges.
Immunocompromised Persons
Immunocompromised states comprise a heterogeneous range of conditions. In many instances, limited data are available regarding the use of influenza vaccines in the setting of specific immunocompromised states. ACIP recommends that LAIV4 not be used in any population for the 2017–18 season; providers considering its use should note that live virus vaccines should not be used for persons with most forms of altered immunocompetence (52), given the uncertain but biologically plausible risk for disease attributable to the vaccine virus. In addition to potential safety issues, immune response to live or inactivated vaccines might be blunted in some clinical situations, such as for persons with congenital immune deficiencies, persons receiving cancer chemotherapy, and persons receiving immunosuppressive medications. For this reason, timing of vaccination might be a consideration (e.g., vaccinating during some period either before or after an immunocompromising intervention).
The Infectious Diseases Society of America (IDSA) has published detailed guidance for the selection and timing of vaccines for persons with specific immunocompromising conditions, including congenital immune disorders, stem cell and solid organ transplant, anatomic and functional asplenia, and therapeutic drug-induced immunosuppression, as well as for persons with cochlear implants or other conditions leading to persistent cerebrospinal fluid-oropharyngeal communication (53). ACIP will continue to review accumulating data on use of influenza vaccines in these contexts.
Persons with a History of Guillain-Barré Syndrome Following Influenza Vaccination
A history of Guillain-Barré Syndrome (GBS) within 6 weeks following a previous dose of any type of influenza vaccine is considered a precaution to vaccination (Table 2). Persons who are not at high risk for severe influenza complications (see Populations at Higher Risk for Medical Complications Attributable to Severe Influenza) and who are known to have experienced GBS within 6 weeks of a previous influenza vaccination generally should not be vaccinated. As an alternative to vaccination, physicians might consider using influenza antiviral chemoprophylaxis for these persons (54). However, the benefits of influenza vaccination might outweigh the risks for certain persons who have a history of GBS and who also are at high risk for severe complications from influenza.
Persons with a History of Egg Allergy
As is the case for other vaccines, influenza vaccines contain various different components that might cause allergic and anaphylactic reactions. Not all such reactions are related to egg proteins; however, the possibility of reactions to influenza vaccines in egg-allergic persons might be of concern to these persons and vaccine providers. Currently available influenza vaccines, with the exceptions of RIV3, RIV4 and ccIIV4, are prepared by propagation of virus in embryonated eggs. Only RIV3 and RIV4 are considered egg-free. For ccIIV4 (Flucelvax Quadrivalent; Seqirus, Holly Springs, North Carolina), ovalbumin is not directly measured. During manufacture of ccIIV4, viruses are propagated in mammalian cells rather than in eggs; however, some of the viruses provided to the manufacturer are egg-derived, and therefore egg proteins may potentially be introduced at the start of the manufacturing process. Once these viruses are received by the manufacturer, no eggs are used, and dilutions at various steps during the manufacturing process result in a theoretical maximum of 5×10-8 μg/0.5 mL dose of total egg protein (Seqirus, unpublished data, 2016).
Severe allergic reactions to vaccines, although rare, can occur at any time, despite a recipient’s allergy history. Therefore, all vaccine providers should be familiar with the office emergency plan, and be certified in cardiopulmonary resuscitation (52). For persons who report a history of egg allergy, ACIP recommends the following (based upon the recipient’s previous symptoms after exposure to egg):
- Persons with a history of egg allergy who have experienced only urticaria (hives) after exposure to egg should receive influenza vaccine. Any licensed and recommended influenza vaccine (i.e., any IIV or RIV) that is otherwise appropriate for the recipient’s age and health status may be used.
- Persons who report having had reactions to egg involving symptoms other than urticaria (hives), such as angioedema, respiratory distress, lightheadedness, or recurrent emesis; or who required epinephrine or another emergency medical intervention, may similarly receive any licensed and recommended influenza vaccine (i.e., any IIV or RIV) that is otherwise appropriate for the recipient’s age and health status. The selected vaccine should be administered in an inpatient or outpatient medical setting (including, but not necessarily limited to, hospitals, clinics, health departments, and physician offices). Vaccine administration should be supervised by a health care provider who is able to recognize and manage severe allergic conditions.
- A previous severe allergic reaction to influenza vaccine, regardless of the component suspected of being responsible for the reaction, is a contraindication to future receipt of the vaccine.
No period of postvaccination observation period is recommended specifically for egg-allergic persons. However, ACIP recommends that vaccine providers consider observing patients for 15 minutes following administration of any vaccine to decrease the risk for injury should syncope occur (52).
Persons who are able to eat lightly cooked egg (e.g., scrambled egg) without reaction are unlikely to be allergic. Egg-allergic persons might tolerate egg in baked products (e.g., bread or cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy. Egg allergy can be confirmed by a consistent medical history of adverse reactions to eggs and egg-containing foods, plus skin and/or blood testing for immunoglobulin E directed against egg proteins (55).
Occasional cases of anaphylaxis in egg-allergic persons have been reported to VAERS after administration of influenza vaccines (56,57). ACIP will continue to review available data regarding anaphylaxis cases following influenza vaccines.
Vaccination Issues for Travelers
Travelers who want to reduce the risk for influenza infection should consider influenza vaccination, preferably at least 2 weeks before departure. In particular, persons residing in the United States who are at high risk for complications of influenza and who were not vaccinated with influenza vaccine during the preceding Northern Hemisphere fall or winter should consider receiving influenza vaccine before departure if they plan to travel:
- to the tropics,
- with organized tourist groups or on cruise ships, or
- to the Southern Hemisphere during the Southern Hemisphere influenza season (April–September).
No information is available indicating a benefit to revaccinating persons before summer travel who already were vaccinated during the preceding fall. In many cases, revaccination will not be feasible as Southern Hemisphere formulations of influenza vaccine are not generally available in the United States. Persons at high risk who receive the previous season’s vaccine before travel should receive the current vaccine the following fall or winter. Persons at higher risk for influenza complications should consult with their health care practitioner to discuss the risk for influenza or other travel-related diseases before embarking on travel during the summer.
In temperate climate regions of the Northern and Southern hemispheres, influenza activity is seasonal, occurring approximately from October through May in the Northern Hemisphere and April through September in the Southern Hemisphere. In the tropics, influenza occurs throughout the year. Travelers can be exposed to influenza when travelling to an area where influenza is circulating, or when traveling as part of large tourist groups (e.g., on cruise ships) that include persons from areas of the world in which influenza viruses are circulating (58,59). In a survey of Swiss travelers to tropical and subtropical countries, among 211 who reported febrile illness during or after travelling abroad and who provided paired serum samples, 40 demonstrated serologic evidence of influenza infection (60). Among 109 travelers returning to Australia from travel in Asia who reported acute respiratory infection symptoms, four (3.7%) had evidence of influenza A infection (evidenced by fourfold rise in antibody titer) (61).
Influenza vaccine formulated for the Southern Hemisphere might differ in viral composition from the Northern Hemisphere vaccine. However, with the exception of the Southern Hemisphere formulation of Fluzone Quadrivalent (IIV4; Sanofi Pasteur, Swiftwater, Pennsylvania), Southern Hemisphere formulation seasonal influenza vaccines are not licensed in the United States, and Southern Hemisphere formulations generally are not commercially available in the United States. More information on influenza vaccines and travel is available at https://www.cdc.gov/flu/travelers/travelersfacts.htm.
Use of Influenza Antiviral Medications
Administration of IIV or RIV to persons receiving influenza antiviral medications for treatment or chemoprophylaxis is acceptable. ACIP recommends that LAIV4 should not be used during the 2017–18 season. If used, providers should note that influenza antiviral medications may reduce the effectiveness of LAIV4 if given within 48 hours before to 14 days after LAIV4 (62). Persons who receive influenza antiviral medications during this period surrounding receipt of LAIV4 may be revaccinated with another appropriate vaccine formulation (e.g., IIV or RIV).
Concurrent Administration of Influenza Vaccine with Other Vaccines
Data regarding potential interference following simultaneous or sequential administration for the many potential combinations of vaccines are limited. Therefore, following the ACIP General Best Practice Guidelines for Immunization is prudent (52). IIVs and RIV may be administered concurrently or sequentially with other inactivated vaccines or with live vaccines. LAIV4 is not recommended for use in 2017–18. Providers considering its use should note that although inactivated or live vaccines can be administered simultaneously with LAIV4, after administration of a live vaccine (such as LAIV4), at least 4 weeks should pass before another live vaccine is administered.
Relatively limited data are available on the concurrent administration of influenza vaccines with other vaccines. In a study comparing the immunogenicity of IIV and zoster vaccine given either concurrently or separated by a 4-week interval to adults aged ≥50 years, antibody responses were similar for both schedules (63). In some studies, reduced responses have been noted to PCV13 (64,65), tetanus antigens (66), and pertussis antigens (66) when co-administered with IIV; in most instances the clinical significance of this is uncertain. Reassuring safety profiles have been noted for simultaneous administration of zoster vaccine (63), PCV13 (64,65), PPSV23 (67) and Tdap (66) among adults and of Tdap among pregnant women (68). Increased prevalence of local and/or systemic adverse reactions have been noted with concurrent administration in some of these studies, but these symptoms have generally been reported to be mild or moderate. Among children, co-administration of IIV and PCV13 was associated with increased risk of fever on the day of vaccination and the day following (i.e., days 0–1 postvaccination) after vaccination in children aged 6 through 23 months in a study conducted during the 2011–12 season (69). Increased risk of febrile seizure in this age group has been noted within days 0–1 following coadministration of IIV with PCV7, PCV13, or DTaP-containing vaccines during the 2006–07 through 2010–11 seasons (70), and with PCV13 during the 2014–15 season (71). No changes in the recommendations for administration of these vaccines were made, and these vaccines may be given concomitantly. Surveillance of febrile seizures is ongoing through VAERS, and the Vaccine Safety Datalink annual influenza vaccine safety surveillance includes monitoring for seizures following vaccination.
Concurrent administration to children of LAIV3 with MMR and varicella vaccine was not associated with diminished immunogenicity to antigens in any of the vaccines in one study (72); diminished response to rubella was observed in another examining coadministraion of LAIV3 and MMR (73). Administration of OPV was not associated with interference when administered with LAIV (74). No safety concerns were revealed in these studies.
Influenza Vaccine Composition and Available Products
Influenza Vaccine Composition for the 2017–18 Season
All influenza vaccines licensed in the United States will contain components derived from influenza viruses antigenically similar to those recommended by FDA (75). Both trivalent and quadrivalent influenza vaccines will be available in the United States. The 2017–18 U.S. influenza vaccines will contain the following components:
- an A/Michigan/45/2015 (H1N1)pdm09–like virus,
- an A/Hong Kong/4801/2014 (H3N2)–like virus, and
- a B/Brisbane/60/2008–like virus (Victoria lineage).
The 2017–18 U.S. quadrivalent vaccines will contain the same three antigens and an additional influenza B virus component, a B/Phuket/3073/2013–like virus (Yamagata lineage). Compared with 2016–17, the composition for 2017–18 represents a change in the influenza A(H1N1)pdm09–like virus.
Vaccine Products for the 2017–18 Season
A variety of influenza vaccine products are licensed and available from several different manufacturers (Table 1). For many vaccine recipients, more than one type or brand of vaccine might be appropriate within approved indications and ACIP recommendations. A licensed, age-appropriate influenza vaccine product should be used. Not all products are likely to be uniformly available in any practice setting or locality. Vaccination should not be delayed in order to obtain a specific product when an appropriate one is already available. Within these guidelines and approved indications, where more than one type of vaccine is appropriate and available, no preferential recommendation is made for use of any influenza vaccine product over another.
Since the publication of the previous season’s guidelines, two new influenza vaccine products have been licensed; Afluria Quadrivalent (IIV4; Seqirus, Parkville, Victoria, Australia) and Flublok Quadrivalent (RIV4; Protein Sciences, Meriden, Connecticut). In addition, a labeling change has been approved for a previously-licensed product: FluLaval Quadrivalent (IIV4, ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada) is now licensed for children aged 6 months and older. These are described in the New Influenza Vaccine Product Approvals section. New licensures and changes to FDA-approved labeling might occur subsequent to this report. These recommendations apply to all licensed influenza vaccines used within FDA–licensed indications, including changes in FDA-approved labeling that might occur after publication of this report. As these changes occur, they will be reflected in the online version of Table 1, available at https://www.cdc.gov/flu/protect/vaccine/vaccines.htm.
Dosage, Administration, Contraindications, and Precautions
Inactivated Influenza Vaccines (IIVs)
Available products: IIVs comprise multiple products (Table 1). Both quadrivalent and trivalent formulations are available.
With one exception, U.S.-licensed IIVs are manufactured through propagation of virus in eggs. The exception, the cell culture-based vaccine Flucelvax Quadrivalent (ccIIV4; Seqirus, Holly Springs, North Carolina), contains vaccine viruses propagated in Madin-Darby canine kidney cells. Flucelvax Quadrivalent is not considered egg-free, as some of the initial vaccine viruses provided to the manufacturer by WHO are egg-derived. For the 2017–18 season, the influenza A (H1N1) and both influenza B components will be egg-derived; the influenza A (H3N2) component will be cell-derived.
With one exception, IIVs licensed in the United States contain no adjuvant. The exception, Fluad (aIIV3; Seqirus, Holly Springs, North Carolina) contains the adjuvant MF59.
There are IIVs that are licensed for persons as young as age 6 months. However, age indications for the various individual IIVs differ (Table 1). Only age-appropriate products should be administered. Afluria (IIV3, Seqirus, Parkville, Victoria, Australia), which was previously recommended for persons aged ≥9 years, is now recommended for persons aged ≥5 years. Providers should consult package inserts and updated CDC/ACIP guidance for current information.
Dosage and administration: All IIV preparations contain 15 µg of HA per vaccine virus strain (45 µg total for IIV3s and 60 µg total for IIV4s) per 0.5 mL dose, with two exceptions. Fluzone High Dose (HD-IIV3; Sanofi Pasteur, Swiftwater, Pennsylvania), an IIV3 licensed for persons aged ≥65 years, contains 60 µg of each HA per vaccine virus strain (180 µg total) (44). Fluzone Intradermal Quadrivalent (intradermal IIV4; Sanofi Pasteur, Swiftwater, Pennsylvania), an intradermally administered IIV4 licensed for persons aged 18 through 64 years, contains 9 µg of each HA per vaccine virus strain (36 µg total) (36).
For children aged 6 through 35 months, two IIV products are licensed by FDA. The approved dose volumes differ for these two products. Children in this age group may receive either 1) 0.5 mL of FluLaval Quadrivalent (ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada) (37), which contains 15 µg of HA per virus, or 2) 0.25 mL dose Fluzone Quadrivalent (Sanofi Pasteur, Swiftwater, Pennsylvania) (35), which contains 7.5 µg of HA per virus. Care must be taken to administer each at the appropriate dose for each product in this age group. If prefilled syringes are not available, the appropriate dose can be taken from a single-use or multidose vial, at the appropriate volume for the given product.
Children aged 36 months through 17 years (for whom only intramuscular IIVs are licensed) and adults aged ≥18 years who are receiving intramuscular preparations of IIV should receive 0.5 mL per dose. If a smaller intramuscular vaccine dose (e.g., 0.25 mL) is administered inadvertently to an adult, an additional 0.25 mL dose should be administered to provide a full dose (0.5 mL). If the error is discovered later (after the patient has left the vaccination setting), a full 0.5 mL dose should be administered as soon as the patient can return. Vaccination with a formulation approved for adult use should be counted as a dose if inadvertently administered to a child.
With the exception of Fluzone Intradermal Quadrivalent (Sanofi Pasteur, Swiftwater, Pennsylvania), IIVs are administered intramuscularly. For adults and older children, the deltoid is the preferred site. Infants and younger children should be vaccinated in the anterolateral thigh. Additional specific guidance regarding site selection and needle length for intramuscular administration are provided in the ACIP General Best Practice Guidelines for Immunization (52). Fluzone Intradermal Quadrivalent is administered intradermally, preferably over the deltoid muscle, using the included delivery system (36). Two IIVs, Afluria and Afluria Quadrivalent (Seqirus, Parkville, Victoria, Australia), are licensed for intramuscular administration via jet injector (Stratis; Pharmajet, Golden, Colorado) for persons aged 18 through 64 years (39,76).
Trivalent versus quadrivalent IIVs: Both trivalent and quadrivalent IIVs will be available during the 2017–18 season. Quadrivalent vaccines contain one virus from each of the two influenza B lineages (one B/Victoria virus and one B/Yamagata virus), whereas trivalent vaccines contain one influenza B virus from one lineage. Quadrivalent vaccines are thus designed to provide broader protection against circulating influenza B viruses. However, no preference is expressed for either IIV3 or IIV4.
Contraindications and precautions for the use of IIVs: Manufacturer package inserts and updated CDC/ACIP guidance should be consulted for current information on contraindications and precautions for individual vaccine products. In general, history of severe allergic reaction to the vaccine or any of its components (including egg) is a labeled contraindication to the receipt of IIVs (Table 2). However, ACIP makes specific recommendations for the use of influenza vaccine for persons with egg allergy (see Persons with a History of Egg Allergy). Influenza vaccine is not recommended for persons with a history of severe allergic reaction to the vaccine or to components other than egg. Information about vaccine components is located in package inserts from each manufacturer. Prophylactic use of antiviral agents is an option for preventing influenza among persons who cannot receive vaccine (54).
Moderate or severe acute illness with or without fever is a general precaution for vaccination (52). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2).
Recombinant Influenza Vaccine (RIVs)
Available products: Two RIV products, Flublok (RIV3) and Flublok Quadrivalent (RIV4), are expected to be available for the 2017–18 influenza season. RIV3 and RIV4 are indicated for persons aged ≥18 years. RIVs are manufactured without the use of influenza viruses; therefore, similarly to IIVs, no shedding of vaccine virus will occur. These vaccines are produced without the use of eggs, and are egg-free. No preference is expressed for RIVs versus IIVs within specified indications.
Dosage and administration: RIVs are administered by intramuscular injection. A 0.5 mL dose contains 45 µg of HA derived from each vaccine virus (135 µg total for RIV3 and 180 µg total for RIV4).
Trivalent versus quadrivalent RIV: Both trivalent and quadrivalent RIV will be available during the 2017–18 season. Quadrivalent vaccines contain one virus from each of the two influenza B lineages (one B/Victoria virus and one B/Yamagata virus), whereas trivalent vaccines contain one influenza B virus from one lineage. Quadrivalent vaccines are thus designed to provide broader protection against circulating influenza B viruses. However, no preference is expressed for either RIV3 or RIV4.
Contraindications and precautions for use of RIV: RIVs are contraindicated in persons who have had a severe allergic reaction to any component of the vaccine. Moderate or severe acute illness with or without fever is a general precaution for vaccination (52). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2). Flublok is not licensed for use in children aged <18 years.
Live Attenuated Influenza Vaccine (LAIV4)
Pending further data, for the 2017–18 season, ACIP recommends that LAIV4 not be used because of concerns regarding its effectiveness against influenza A(H1N1)pdm09 viruses in the United States during the 2013–14 and 2015–16 seasons. As it is a licensed vaccine and might be available during 2017–18, the material in this section is provided for information.
Dosage and administration: LAIV4 is administered intranasally using the supplied prefilled, single-use sprayer containing 0.2 mL of vaccine. Approximately 0.1 mL (i.e., half of the total sprayer contents) is sprayed into the first nostril while the recipient is in the upright position. An attached dose-divider clip is removed from the sprayer to administer the second half of the dose into the other nostril. If the vaccine recipient sneezes immediately after administration, the dose should not be repeated. However, if nasal congestion is present that might impede delivery of the vaccine to the nasopharyngeal mucosa, deferral of administration should be considered until resolution of the illness, or another appropriate vaccine should be administered instead.
Contraindications and precautions: ACIP recommends that LAIV4 not be used during the 2017–18 season. Previously issued guidance regarding contraindications and precautions is provided for informational purposes only (Table 2).
New Influenza Vaccine Product Approvals
Since the publication of the previous season’s guidance, there have been two new product approvals (Afluria Quadrivalent and Flublok Quadrivalent) and one change to the approved indication for an existing product (expansion of the age indication for FluLaval Quadrivalent from ≥3 years to ≥6 months).
Afluria Quadrivalent (IIV4)
Afluria Quadrivalent (IIV4, Seqirus, Parkville, Victoria, Australia) was licensed by FDA in August 2016, for persons aged ≥18 years, and was available during the 2016–17 season alongside the trivalent formulation of Afluria. In a prelicensure study of the safety and immunogenicity of Afluria Quadrivalent compared with two formulations of Afluria (each containing one of the two influenza B viruses contained in the quadrivalent) among persons aged ≥18 years, Afluria Quadrivalent met pre-specified criteria for immunologic noninferiority for all four vaccine viruses, and criteria for immunologic superiority for each B virus as compared to the trivalent formulation containing the alternate B virus.
Some local injection site reactions were more common among those who received Afluria Quadrivalent, including an imbalance of Grade 3 injection site induration/swelling at 0.3% in the Afluria Quadrivalent group and 0.06% in the pooled Afluria trivalent groups), but rates of these reactions were low overall (77,78).
Flublok Quadrivalent (RIV4)
Flublok Quadrivalent (RIV4; Protein Sciences, Meriden, Connecticut) was licensed by FDA in October 2016, for persons aged ≥18 years. It is anticipated that Flublok Quadrivalent will be available for the 2017–18 season, alongside the trivalent formulation of Flublok. In a prelicensure analysis of immunogenicity data from a subset of participants enrolled in a randomized relative efficacy trial comparing Flublok Quadrivalent with a licensed comparator standard-dose IIV4 among persons aged ≥50 years during the 2014–15 season, Flublok Quadrivalent met criteria for noninferiority to the comparator IIV4 for the A(H3N2) and B/Yamagata antigens, but not for the A(H1N1) or B/Victoria antigens (47). In an exploratory analysis of data from this trial (N = 8,604), Flublok Quadrivalent demonstrated 30% greater relative efficacy (95% confidence interval [CI] = 10–47) over IIV4 (46,47). In a second prelicensure study, evaluating safety, reactogenicity, and immunogenicity compared with a licensed IIV4 among persons aged 18 through 49 years during the 2014–15 season, Flublok Quadrivalent met criteria for noninferiority to the comparator IIV4 for the A(H1N1), A(H3N2) and B/Yamagata antigens, but not for the B/Victoria antigen. Safety data from both studies suggested comparable safety to the comparator IIV4 for persons aged ≥18 years (47).
FluLaval Quadrivalent (IIV4)
In November 2016, FDA approved expansion of the licensed age indication for FluLaval Quadrivalent (IIV4; ID Biomedical Corporation of Quebec, Quebec City, Quebec, Canada). Previously licensed for persons aged ≥3 years, FluLaval Quadrivalent is now licensed for persons aged ≥6 months. The approved dose volume is 0.5 mL for all ages. This represents a new option for vaccination of children aged 6 through 35 months, for whom previously the only approved influenza vaccine formulation was the 0.25 mL dose volume of Fluzone Quadrivalent. With this approval, children in this age group may receive either 0.5 mL of FluLaval Quadrivalent or 0.25 mL of Fluzone Quadrivalent for each dose needed.
In a prelicensure study comparing the immunogenicity and safety of 0.5 mL of FluLaval Quadrivalent to that of 0.25 mL of Fluzone Quadrivalent among children aged 6 through 35 months, FluLaval Quadrivalent met criteria for immunogenic noninferiority for all four vaccine strains. Safety and reactogenicity were similar between the two vaccines (30,79).
Storage and Handling of Influenza Vaccines
In all instances, approved manufacturer packaging information should be consulted for authoritative guidance concerning storage and handling of all influenza vaccines. Vaccines should be protected from light and stored at recommended temperatures. In general, influenza vaccines are recommended to be stored refrigerated between 2° to 8°C (36° to 46°F) and should not be frozen. Vaccine that has frozen should be discarded. In addition, the cold chain must be maintained when LAIV4 is transported. Single-dose vials should not be accessed for more than one dose. Multiple-dose vials should be returned to recommended storage conditions between uses, and once first accessed should not be kept beyond the recommended period of time. For information on permissible temperature excursions and other departures from recommended storage conditions that are not discussed in the package labelling, contact the manufacturer. Vaccines should not be used after the expiration date on the label.
Additional Sources for Information Regarding Influenza and Vaccines
Influenza Surveillance, Prevention, and Control
Updated information regarding influenza surveillance, detection, prevention, and control is available at https://www.cdc.gov/flu. U.S surveillance data are updated weekly during October–May on FluView (https://www.cdc.gov/flu/weekly). In addition, periodic updates regarding influenza are published in MMWR (https://www.cdc.gov/mmwr). Additional information regarding influenza vaccine can be obtained from CDC by calling 1-800-232-4636. State and local health departments should be consulted about availability of influenza vaccine, access to vaccination programs, information related to state or local influenza activity, reporting of influenza outbreaks and influenza-related pediatric deaths, and advice concerning outbreak control.
Vaccine Adverse Event Reporting System
The National Childhood Vaccine Injury Act of 1986 requires health care providers to report any adverse event listed by the vaccine manufacturer as a contraindication to further doses of the vaccine, or any adverse event listed in the VAERS Table of Reportable Events Following Vaccination (https://vaers.hhs.gov/docs/VAERS_Table_of_Reportable_Events_Following_Vaccination.pdf) that occurs within the specified time period after vaccination. In addition to mandated reporting, health care providers are encouraged to report any clinically significant adverse event following vaccination to VAERS. Information on how to report a vaccine adverse event is available at https://vaers.hhs.gov/index.html. Additional information on VAERS and vaccine safety is available by emailing info@vaers.org or by calling 1-800-822-7967.
National Vaccine Injury Compensation Program
The National Vaccine Injury Compensation Program (VICP), established by the National Childhood Vaccine Injury Act of 1986, as amended, provides a mechanism through which compensation can be paid on behalf of a person determined to have been injured or to have died as a result of receiving a vaccine covered by VICP. The Vaccine Injury Table (https://www.hrsa.gov/vaccinecompensation/vaccineinjurytable.pdf) lists the vaccines covered by VICP and the associated injuries and conditions (including death) that might receive a legal presumption of causation. If the injury or condition is not on the Table, or does not occur within the specified time period on the Table, persons must prove that the vaccine caused the injury or condition. Eligibility for compensation is not affected by whether a covered vaccine is used off-label or inconsistently with recommendations.
To be eligible for compensation under VICP, a claim must be filed within 3 years after the first symptom of the vaccine injury. Death claims must be filed within 2 years of the vaccine-related death and not more than 4 years after the start of the first symptom of the vaccine-related injury from which the death occurred. When a new vaccine is covered by VICP or when a new injury/condition is added to the Table, claims that do not meet the general filing guidelines must be filed within 2 years from the date the vaccine or injury/condition is added to the Table for injuries or deaths that occurred up to 8 years before the Table change (80). Persons of all ages who receive a VICP-covered vaccine might be eligible to file a claim. Additional information is available at https://www.hrsa.gov/vaccinecompensation or by calling 1-800-338-2382.
Additional Resources
ACIP Statements
- General Best Practice Guidelines for Immunization: Best Practices Guidance of the Advisory Committee on Immunization Practices (ACIP). https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html
- Immunization of Healthcare Personnel: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Recomm Rep 2011;60(No. RR-7). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6007a1.htm
- Recommended Immunization Schedules for Adults, 2017: https://www.cdc.gov/vaccines/schedules/hcp/adult.html
- Recommended Immunization Schedule for Children and Adolescents Aged 18 years or Younger, 2017: https://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html
Vaccine Information Sheets (VISs)
- VIS for IIV and RIV: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flu.pdf
- VIS for LAIV: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/flulive.pdf
Influenza Vaccine Package Inserts
- Trivalent Vaccines: https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094045.htm
- Quadrivalent Vaccines: https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm295057.htm
CDC Influenza Antiviral Guidance
- Antiviral Drugs: Information for Healthcare Professionals: https://www.cdc.gov/flu/professionals/antivirals/index.htm
American Academy of Pediatrics (AAP) Guidance
- AAP Recommendations for Prevention and Control of Influenza in Children: https://redbook.solutions.aap.org/ss/influenza-resources.aspx
Infectious Diseases Society of America (IDSA) Guidance
- 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host: https://academic.oup.com/cid/article/58/3/e44/336537/2013–IDSA-Clinical-Practice-Guideline-for
A list of Work Group members may be found on page 20 of this report.*
CDC: Disaster Preparedness for Expectant and New Parents as Maria storms in…….
Tuesday, September 19th, 2017Preparedness for Expectant and New Parents
 Disasters, such as wildfires(https://www.cdc.gov/reproductivehealth/emergency/wildfires.htm), hurricanes(https://www.cdc.gov/disasters/hurricanes/index.html), and floods(https://www.cdc.gov/disasters/floods/index.html), can be unpredictable and devastating. In honor of National Preparedness Month, learn general tips to get prepared before a disaster and what to do in case of a disaster to help keep you and your family safe and healthy.
Disasters, such as wildfires(https://www.cdc.gov/reproductivehealth/emergency/wildfires.htm), hurricanes(https://www.cdc.gov/disasters/hurricanes/index.html), and floods(https://www.cdc.gov/disasters/floods/index.html), can be unpredictable and devastating. In honor of National Preparedness Month, learn general tips to get prepared before a disaster and what to do in case of a disaster to help keep you and your family safe and healthy.
Get Prepared for an Emergency or Disaster
Disasters can be scary and stressful, especially if you’re expecting or have a baby. You can take the following steps now to help you prepare for an emergency and better cope if an emergency happens.
- Talk to your doctor or other healthcare provider about—
- What steps you should take in any emergency.
- Where you will get prenatal care if your doctor’s office is closed.
- Where you will deliver your baby if your hospital is closed.
- Learn the signs of signs of preterm labor(https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm#warning_signs) (labor before 37 weeks of pregnancy) and prepare emergency birth kit supplies.
- Learn about your community’s warning signals (such as tornado sirens) and check with your state emergency management agency to find out how to get emergency alerts and about the best places to take shelter during different types of emergencies.
- Make a family communication plan for how you and your family will contact one another and what steps you will take in different types of situations.
- Prepare an emergency kit that includes a 3-day supply of food and water, health supplies (including any medicines you may be taking), personal and baby care items, safety supplies, electronics (flashlight, radio, cell phone with charger, and extra batteries), and important documents, such as emergency telephone numbers.
- Plan ahead for where your baby will sleep if you have to evacuate your home. Your baby is safest sleeping on his or her back on a surface that is separate from others and does not have pillows, blankets, or toys. Learn more about these and other actions at Parents and Caregivers(https://www.cdc.gov/sids/Parents-Caregivers.htm#prevention) .
 Once you are out of immediate danger, continue your prenatal care even if it is not with your primary doctor.
Once you are out of immediate danger, continue your prenatal care even if it is not with your primary doctor.
What to Do During and Just After Disaster
Expectant Parents
Pregnant women have special medical needs. If you’re pregnant or think you may be pregnant, you and your partner can take the following steps to help you stay safe and healthy in the event of a disaster.
- If you have any signs of preterm labor(https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm#warning_signs) (labor before 37 weeks of pregnancy), call your healthcare provider or 911, or go to the hospital immediately if it is safe to leave.
- If you have to evacuate, be prepared to leave quickly and have your emergency kit ready to go.
- If staying at a shelter or in temporary housing, tell the staff as soon as possible that you are pregnant and if you have any health problems.
- Once you are out of immediate danger, continue your prenatal care, even if it is not with your primary doctor. Tell the doctor or other healthcare provider if you have any health problems and if you take any medications (both over-the-counter and prescription).
- If you have your prenatal vitamins or prescription medicines with you, take them as directed. If you don’t have your prenatal vitamins or prescription medicines with you, ask staff at the shelter for help getting them.
- Protect yourself from infections by washing your hands often and staying away from people who are sick.
- During disasters, harmful chemicals(https://www.cdc.gov/disasters/chemicals.html) from businesses and other places may be released into the environment. Listen to announcements from emergency officials about chemical safety and actions you may need to take to protect yourself. If you have questions about exposure to harmful chemicals during pregnancy, call MotherToBaby at 1-866-626-6847. To reach the nationwide poison control center, call 1-800-222-1222.
- To help with physical stress, drink plenty of water and rest as often as you can. To help relieve emotional stress, talk to a healthcare provider, friend, or family member about your concerns and feelings.
 Your baby is safest sleeping on his or her back on a surface that is separate from others and does not have pillows, blankets, or toys.
Your baby is safest sleeping on his or her back on a surface that is separate from others and does not have pillows, blankets, or toys.
Parents of Infants
A disaster can make it difficult to access necessary supplies and health care. Parents and caregivers of infants can take the following steps to help keep their families safe and healthy in the event of a disaster.
- If you have to evacuate, be prepared to leave quickly and have your emergency kit that includes infant care supplies, such as baby food and a portable crib, ready to go.
- If you breastfeed your baby, continue to do so. Clean water may not be available for mixing formula or washing bottles. If you have questions about exposure to harmful chemicals while breastfeeding, call MotherToBaby at 1-866-626-6847. To reach the nationwide poison control center, call 1-800-222-1222.
- If you are away from your home during a disaster, take these actions to help your baby sleep safely(https://www.cdc.gov/sids/Parents-Caregivers.htm#prevention) .
- As soon as it is safe to do so, get a postpartum checkup if you are due for a visit, even if it is not with your usual doctor. If you’re not ready to get pregnant, you can ask for several months’ supply of the pill, patch, or ring or consider using a birth control method(https://www.cdc.gov/reproductivehealth/contraception/index.htm) that will prevent pregnancy for several months.
- As soon as it is safe to do so, see a doctor or other healthcare provider for well-baby checkups or if you’re concerned about a health problem, even if it is not with your baby’s usual doctor.
- If you have your prescription medicines with you, take them as directed. If you don’t have your medicines with you, ask staff at the shelter for help getting them.
- If your baby is currently taking prescription or over-the-counter medicines, and you have them, continue giving them as directed.
- To help relieve emotional stress, talk to a healthcare provider, friend, or family member about your concerns and feelings.
More Information
- Emergency Preparedness and Response: Pregnant Women and Newborns(https://www.cdc.gov/reproductivehealth/emergency/index.html)
- Information for Pregnant Women
- Caring for Your Family in a Disaster
- Parents and Parents-to-be(https://www.cdc.gov/childrenindisasters/parents.html)
- For health professionals: Emergency Preparedness and Response: Online Training Course(https://www.cdc.gov/reproductivehealth/emergency/training-course/index.html)
- To locate family: FEMA’s National Emergency Family Registry and Locator System
Secretary Price Appoints Brenda Fitzgerald, M.D., as CDC Director and ATSDR Administrator
Saturday, July 8th, 2017
Secretary Price Appoints Brenda Fitzgerald, M.D., as CDC Director and ATSDR Administrator
Today, Health and Human Services Secretary Tom Price, M.D., named Brenda Fitzgerald, M.D., as the 17th Director of the Centers for Disease Control and Prevention (CDC) and Administrator of the Agency for Toxic Substances and Disease Registry (ATSDR).
“Today, I am extremely proud and excited to announce Dr. Brenda Fitzgerald as the new Director of the CDC,” said Secretary Price. “Having known Dr. Fitzgerald for many years, I know that she has a deep appreciation and understanding of medicine, public health, policy and leadership—all qualities that will prove vital as she leads the CDC in its work to protect America’s health 24/7. We look forward to working with Dr. Fitzgerald to achieve President Trump’s goal of strengthening public health surveillance and ensuring global health security at home and abroad. Congratulations to Dr. Fitzgerald and her family.”
Dr. Fitzgerald has been the commissioner of the Georgia Department of Public Health (DPH) and state health officer for the past six years. She replaces Dr. Anne Schuchat, who has been the acting CDC director and acting ATSDR administrator since January 20. Dr. Schuchat is returning to her role as CDC’s principal deputy director.
“Additionally, I’d like to extend my deep appreciation and thanks to Dr. Anne Schuchat for her exemplary service as acting director of the CDC,” said Secretary Price. “We thank Dr. Schuchat and her team for their dedication in our public health efforts to keep Americans safe and for their work to ensure a seamless transition. We look forward to continuing to work with Dr. Schuchat in her role as principal deputy director of CDC.”
Dr. Fitzgerald, a board-certified obstetrician-gynecologist, has practiced medicine for three decades. As Georgia DPH Commissioner, Dr. Fitzgerald oversaw various state public health programs and directed the state’s 18 public health districts and 159 county health departments. Prior to that, Dr. Fitzgerald held numerous leadership positions. She served on the board and as president of the Georgia OB-GYN Society and she worked as a health care policy advisor with House Speaker Newt Gingrich and Senator Paul Coverdell. She has served as a Senior Fellow and Chairman of the Board for the Georgia Public Policy Foundation.
Dr. Fitzgerald holds a Bachelor of Science degree in Microbiology from Georgia State University and a Doctor of Medicine degree from Emory University School of Medicine. She completed post-graduate training at the Emory-Grady Hospitals in Atlanta and held an assistant clinical professorship at Emory Medical Center. As a Major in the U.S. Air Force, Dr. Fitzgerald served at the Wurtsmith Air Force Strategic Air Command (SAC) Base in Michigan and at the Andrews Air Force Base in Washington, D.C.