16 August 2017 – As millions of people in Somalia remain trapped in a devastating cycle of hunger and disease, WHO and health partners are working with national health authorities to save lives and reach the most vulnerable with essential health services.
More than 2 years of insufficient rainfall and poor harvests have led to drought, food insecurity and a real risk of famine. Malnutrition, mass displacement as a result of the drought, and lack of access to clean water and sanitation have created ideal conditions for infectious disease outbreaks.
“Somalia is facing one of the worst humanitarian crises in the world. Millions of people, already on the brink of famine, are now at risk of rapidly spreading infectious diseases like cholera and measles. Normally, these diseases are easy to treat and prevent, but they can turn deadly when people are living in overcrowded spaces and are too weak to fight off infection,” said Dr Ghulam Popal, WHO Representative in Somalia.
Drought has led to a lack of clean water and the largest cholera outbreak in the last 5 years, with more than 57 000 cases and 809 cumulative deaths reported as of 31 July 2017. Health partners, together with national health authorities, scaled up its efforts to respond to this event by setting up cholera treatment centers in affected districts and providing support in water and sanitation to prevent the spread of the disease. In March, WHO and partners conducted Somalia’s first national oral cholera vaccination campaign, and successfully reached over 450 000 vulnerable people. Due to ongoing efforts, the number of cholera cases in Somalia has declined, from 13 656 cases of acute watery diarrhoea/cholera in May 2017 to 11 228 cases in June 2017.
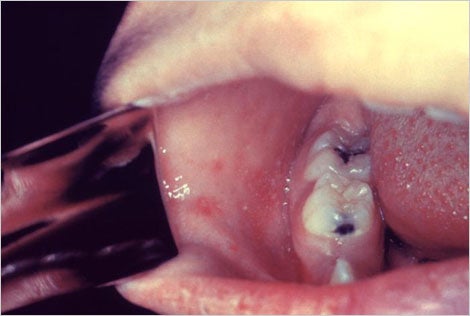
Somalia is also facing its worst measles outbreak in 4 years, with over 14 823 suspected cases reported in 2017 (as of 31 July), compared to 5000–10 000 cases per year since 2014. The situation is especially critical for millions of under-vaccinated, weak and hungry children who are more susceptible to contracting infectious diseases. More than 80% of those affected by the current outbreak are children under 10 year of age.
In early 2017, WHO and partners, in collaboration with national health authorities, vaccinated almost 600 000 children aged 6 months to 5 years for measles in hard-to-reach and hotspot areas across the country. Despite these efforts, the transmission of measles continues, compounded by the ongoing pre-famine situation, continued mass displacement, and undernourished children living in unhygienic conditions.
In order to contain the outbreak, a nationwide campaign is planned for November 2017 to stop transmission of the disease, targeting 4.2 million children. The campaign will also intensify efforts to strengthen routine immunization and reach unvaccinated children to boost their immunity. As shown by the response to the cholera outbreak, with the right interventions, health authorities are confident that similar success may be seen in controlling the measles outbreak.
US$ 14.4 million (a cost of US$ 3.36 per child) is required by WHO and health partners to conduct the measles vaccination campaign in November 2017, of which WHO required US$ 6.8 million. To date, no funding has been received.