19 November 2018
The World malaria report, published annually, provides a comprehensive update on global and regional malaria data and trends. The latest report, released on 19 November 2018, tracks investments in malaria programmes and research as well as progress across all intervention areas: prevention, diagnosis, treatment and surveillance. It also includes dedicated chapters on malaria elimination and on key threats in the fight against malaria. The report is based on information received from national malaria control programmes and other partners in endemic countries; most of the data presented is from 2017.
Global and regional malaria burden, in numbers
Malaria cases
In 2017, an estimated 219 million cases of malaria occurred worldwide (95% confidence interval [CI]: 203–262 million), compared with 239 million cases in 2010 (95% CI: 219–285 million) and 217 million cases in 2016 (95% CI: 200–259 million).
Although there were an estimated 20 million fewer malaria cases in 2017 than in 2010, data for the period 2015–2017 highlight that no significant progress in reducing global malaria cases was made in this timeframe.
Most malaria cases in 2017 were in the WHO African Region (200 million or 92%), followed by the WHO South-East Asia Region with 5% of the cases and the WHO Eastern Mediterranean Region with 2%.
Fifteen countries in sub-Saharan Africa and India carried almost 80% of the global malaria burden. Five countries accounted for nearly half of all malaria cases worldwide: Nigeria (25%), Democratic Republic of the Congo (11%), Mozambique (5%), India (4%) and Uganda (4%).
The 10 highest burden countries in Africa reported increases in cases of malaria in 2017 compared with 2016. Of these, Nigeria, Madagascar and the Democratic Republic of the Congo had the highest estimated increases, all greater than half a million cases. In contrast, India reported 3 million fewer cases in the same period, a 24% decrease compared with 2016.
Rwanda has noted a reduction in its malaria burden, with 430 000 fewer cases in 2017 than in 2016, and Ethiopia and Pakistan estimated decreases of more than 240 000 cases over the same period.
The incidence rate of malaria declined globally between 2010 and 2017, from 72 to 59 cases per 1000 population at risk. Although this represents an 18% reduction over the period, the number of cases per 1000 population at risk has stood at 59 for the past 3 years.
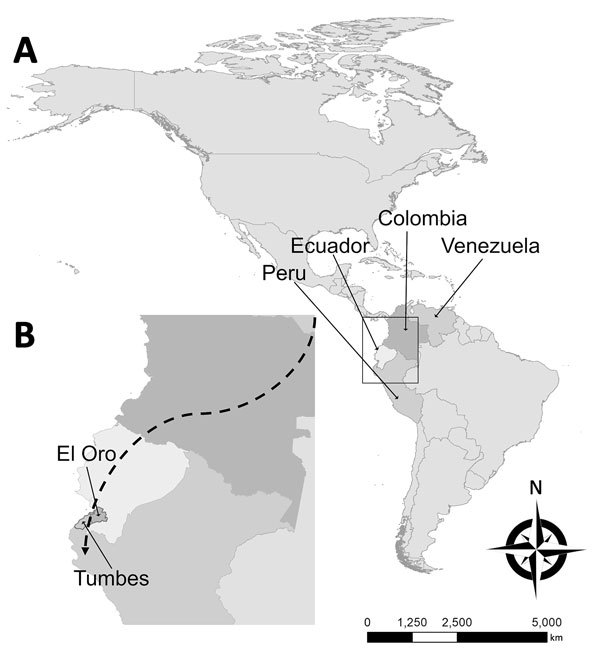
The WHO South-East Asia Region continued to see its incidence rate fall – from 17 cases of the disease per 1000 population at risk in 2010 to 7 in 2017 (a 59% decrease). All other WHO regions recorded either little progress or an increase in incidence rate. The WHO Region of the Americas recorded a rise, largely due to increases in malaria transmission in Brazil, Nicaragua and Venezuela (Bolivarian Republic of). In the WHO African Region, the malaria incidence rate remained at 219 cases per 1000 population at risk for the second year in a row.
Plasmodium falciparum is the most prevalent malaria parasite in the WHO African Region, accounting for 99.7% of estimated malaria cases in 2017, as well as in the WHO regions of South-East Asia (62.8%), the Eastern Mediterranean (69%) and the Western Pacific (71.9%). P. vivax is the predominant parasite in the WHO Region of the Americas, representing 74.1% of malaria cases.
Malaria deaths
In 2017, there were an estimated 435 000 deaths from malaria globally, compared with 451 000 estimated deaths in 2016, and 607 000 in 2010.
Children aged under 5 years are the most vulnerable group affected by malaria. In 2017, they accounted for 61% (266 000) of all malaria deaths worldwide.
The WHO African Region accounted for 93% of all malaria deaths in 2017. Although the WHO African Region was home to the highest number of malaria deaths in 2017, it also accounted for 88% of the 172 000 fewer global malaria deaths reported in 2017 compared with 2010.
Nearly 80% of global malaria deaths in 2017 were concentrated in 17 countries in the WHO African Region and India; 7 of these countries accounted for 53% of all global malaria deaths: Nigeria (19%), Democratic Republic of the Congo (11%), Burkina Faso (6%), United Republic of Tanzania (5%), Sierra Leone (4%), Niger (4%) and India (4%).
All WHO regions except the WHO Region of the Americas recorded reductions in mortality in 2017 compared with 2010. The largest declines occurred in the WHO regions of South- East Asia (54%), Africa (40%) and the Eastern Mediterranean (10%). Despite these gains, the malaria mortality reduction rate has also slowed since 2015, reflecting the estimated trends in malaria case incidence.
Malaria-related anaemia
This year’s report includes a section on malaria-related anaemia, a condition that, left untreated, can result in death, especially among vulnerable populations such as pregnant women and children aged under 5 years.
Anaemia was once a key indicator of progress in malaria control, and its prevalence was used to evaluate the efficacy of interventions. Recent years have seen a decline in awareness of the burden of malaria-associated anaemia
Despite its importance as a direct and indirect consequence of malaria, the prevalence of anaemia among populations vulnerable to the disease has not been reported consistently as a metric of malaria transmission and burden.
Data from household surveys conducted in 16 high-burden African countries between 2015 and 2017 show that, among children aged under 5 years, the prevalence of any anaemia was 61%, mild anaemia 25%, moderate anaemia 33% and severe anaemia 3%. Of children who tested positive for malaria, the prevalence of any anaemia was 79%, mild anaemia 21%, moderate anaemia 50% and severe anaemia 8%.
Investments in malaria programmes and research
Malaria control and elimination investments
In 2017, an estimated US$ 3.1 billion was invested in malaria control and elimination efforts globally by governments of malaria endemic countries and international partners – an amount slighter higher than the figure reported for 2016.
Nearly three quarters (US$ 2.2 billion) of investments in 2017 were spent in the WHO African Region, followed by the WHO regions of South-East Asia (US$ 300 million), the Americas (US$ 200 million), and the Eastern Mediterranean and the Western Pacific (US$ 100 million each).
In 2017, US$ 1.4 billion was invested in low-income countries, US$ 1.2 billion in lower-middle income countries and US$ 300 million in upper-middle-income countries. International funding represented the major source of funding in low-income and lower-middle-income countries, at 87% and 70%, respectively.
Governments of endemic countries contributed 28% of total funding (US$ 900 million) in 2017, a figure unchanged from 2016. Two thirds of domestically sourced funds were invested in malaria control activities carried out by national malaria programmes (NMPs), with the remaining share estimated as the cost of patient care.
As in previous years, the United States of America (USA) was the largest international source of malaria financing, providing US$ 1.2 billion (39%) in 2017. Country members of the Development Assistance Committee together accounted for US$ 700 million (21%). The United Kingdom of Great Britain and Northern Ireland contributed around US$ 300 million (9%) while the Bill & Melinda Gates Foundation provided US$ 100 million (2%).
Of the US$ 3.1 billion invested in 2017, US$ 1.3 billion was channelled through the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Investment outlook
Although funding for malaria has remained relatively stable since 2010, the level of investment in 2017 is far from what is required to reach the first 2 milestones of the GTS; that is, a reduction of at least 40% in malaria case incidence and mortality rates globally by 2020, compared with 2015 levels.
To reach the GTS 2030 targets, it is estimated that annual malaria funding will need to increase to at least US$ 6.6 billion per year by 2020.
Stepping up investments in malaria research and development is key to achieving the GTS targets. In 2016, US$ 588 million was spent in this area, representing 85% of the estimated annual need for research and development.
Although research and development funding for malaria vaccines and drugs declined in 2016 compared with 2015, investments in vector control products almost doubled, from US$ 33 million to US$ 61 million.
Deliveries of malaria commodities
Insecticide-treated mosquito nets
Between 2015 and 2017, a total of 624 million insecticide-treated mosquito nets (ITNs), mainly long-lasting insecticidal nets (LLINs), were reported by manufacturers as having been delivered globally. This represents a substantial increase over the previous period 2012–2014, when 465 million ITNs were delivered globally.
An estimated 552 million ITNs were distributed by NMPs globally, with most (459 million or 83%) being delivered in sub-Saharan Africa over the period 2015–2017.
Globally, 85% of ITNs were distributed through free mass distribution campaigns, 8% in antenatal care facilities and 4% as part of immunization programmes.
Rapid diagnostic tests
An estimated 276 million rapid diagnostic tests (RDTs) were sold globally in 2017.
In 2017, 245 million RDTs were distributed by NMPs. Most RDTs (66%) were tests that detected P. falciparum only and were supplied to sub-Saharan Africa.
In sub-Saharan Africa, RDTs are becoming increasingly the most used method to test for malaria diagnosis among suspected malaria patients in public health facilities. In 2017, an estimated 75% of malaria tests were conducted using RDTs, up from 40% in 2010.
Artemisinin-based combination therapy
An estimated 2.74 billion treatment courses of artemisinin-based combination therapy (ACT) were procured by countries over the period 2010–2017. An estimated 62% of these procurements were reported to have been made for the public sector.
During the period 2010–2017, 1.45 billion ACT treatment courses were delivered by NMPs, of which 1.42 billion (98%) were in the WHO African Region.
With increases in diagnostic testing in recent years, ACT treatment courses are becoming more targeted towards patients who tested positive for malaria. This is demonstrated by a substantially reduced ratio of ACTs to tests (0.8 in 2017 compared with 2.5 in 2010). Nevertheless, this implies that an estimated 30% of patients who received ACTs were not tested for malaria.
Preventing malaria
Vector control
Half of people at risk of malaria in Africa are sleeping under an ITN: in 2017, 50% of the population was protected by this intervention, an increase from 29% in 2010. Furthermore, the percentage of the population with access to an ITN increased from 33% in 2010 to 56% in 2017. However, coverage has improved only marginally since 2015 and has been at a standstill since 2016.
Households with at least 1 ITN for every 2 people doubled to 40% between 2010 and 2017. However, this figure represents only a modest increase over the past 3 years, and remains far from the target of universal coverage.
Fewer people at risk of malaria are being protected by indoor residual spraying (IRS), a prevention method that involves spraying the inside walls of dwellings with insecticides. Globally, IRS protection declined from a peak of 5% in 2010 to 3% in 2017, with decreases seen across all WHO regions.
In the WHO African Region, IRS coverage dropped from 80 million people at risk in 2010, to a low point of 51 million in 2016 before rising to 64 million in 2017. In other WHO regions, the number of people protected with IRS in 2017 was 1.5 million in the Americas, 7.5 million in the Eastern Mediterranean, 41 million in South-East Asia, and 1.5 million in the Western Pacific.
The declines in IRS coverage are occurring as countries change or rotate insecticides (changing to more expensive chemicals), and as operational strategies change (e.g. decreasing at-risk populations in malaria elimination countries).
Preventive therapies
To protect women in areas of moderate and high malaria transmission in Africa, WHO recommends “intermittent preventive treatment in pregnancy” (IPTp) with the antimalarial drug sulfadoxine-pyrimethamine. Among 33 African countries that reported on IPTp coverage levels in 2017, an estimated 22% of eligible pregnant women received the recommended 3 or more doses of IPTp, compared with 17% in 2015 and 0% in 2010.
In 2017, 15.7 million children in 12 countries in Africa’s Sahel subregion were protected through seasonal malaria chemoprevention (SMC) programmes. However, about 13.6 million children who could have benefited from this intervention were not covered, mainly due to a lack of funding.
Diagnostic testing and treatment
Accessing care
Prompt diagnosis and treatment is the most effective way to prevent a mild case of malaria from developing into severe disease and death. Based on national household surveys completed in 19 countries in sub-Saharan Africa between 2015 and 2017, a median of 52% (interquartile range [IQR]: 44–62%) of children with a fever (febrile) were taken to a trained medical provider for care. This includes public sector hospitals and clinics, formal private sector health facilities and community health workers.
Although more febrile children were brought for care in the public health sector (median: 36%, IQR: 30–46%) than in the formal medical private sector (median: 8%, IQR: 5–10%), a high proportion of febrile children did not receive any medical attention (median: 40%, IQR: 28–45%). Poor access to health care providers or lack of awareness of malaria symptoms among caregivers are among the contributing factors.
The national surveys reveal disparities in access to health care based on household income and location: the percentage of febrile children brought for care was higher in wealthier households (median: 72%, IQR: 62–75%) compared with poorer households (median: 58%, IQR: 47–67%), and was higher among those living in urban areas (median: 69%, IQR: 59–76%) compared with rural areas (median: 60%, IQR: 51–71%).
Diagnosing malaria
According to 58 surveys conducted in 30 sub-Saharan African countries between 2010 and 2017, the percentage of children with a fever that received a diagnostic test in the public health sector has increased, hitting a median of 59% (IQR: 34–75%) over the period 2015– 2017, up from a median of 33% (IQR:18–44%) for 2010–2012.
Data collected from 56 surveys carried out in sub-Saharan Africa reveal that the percentage of febrile children attending public health facilities who received a malaria diagnostic test before antimalarial treatment has gone up from a median of 35% (IQR: 27–56%) in 2010–2012 to 74% (IQR: 51–81%) in 2015–2017. A similar increase has been recorded in the formal private health sector, from 41% (IQR: 17–67%) in 2010–2012 to 63% (IQR: 41–83%) in 2015–2017.
Treating malaria
Based on 19 household surveys conducted in sub-Saharan Africa between 2015 and 2017, the percentage of children aged under 5 years with a fever who received any antimalarial drug was 29% (IQR: 15–48%).
Children are more likely to be given ACTs – the most effective antimalarial drugs – if medical care is sought in the public sector compared with the private sector. Data from 18 national surveys conducted in sub-Saharan Africa show that for the period 2015–2017, an estimated 88% (IQR: 73–92%) of febrile children brought for treatment for malaria in the public health sector received ACTs, compared with 74% (IQR: 47–88%) in the formal medical private sector.
To bridge the treatment gap among children, WHO recommends the uptake of integrated community case management (iCCM). This approach promotes integrated management of common life-threatening conditions in children – malaria, pneumonia and diarrhoea – at health facility and community levels. In 2017, of 21 African countries with high malaria burden, 20 had iCCM policies in place, of which 12 had started implementing those policies.
Malaria surveillance systems
Effective surveillance of malaria cases and deaths is essential for identifying the areas or population groups that are most affected by malaria, and for targeting resources for maximum impact. A strong surveillance system requires high levels of access to care and case detection, and complete reporting of health information by all sectors, whether public or private.
In 2017, among 52 moderate to high-burden countries, reporting rates of malaria were 60% or more. In the WHO African Region, 36 out of 46 countries indicated that at least 80% of public health facilities had reported data on malaria through their national health information system.
Malaria elimination
Globally, the elimination net is widening, with more countries moving towards zero indigenous cases: in 2017, 46 countries reported fewer than 10 000 such cases, up from 44 countries in 2016 and 37 countries in 2010. The number of countries with less than 100 indigenous cases – a strong indicator that elimination is within reach – increased from 15 countries in 2010 to 24 countries in 2016 and 26 countries in 2017.
Paraguay was certified by WHO as malaria free in 2018, while Algeria, Argentina and Uzbekistan have made formal requests to WHO for certification. In 2017, China and El Salvador reported zero indigenous cases.
One of the key GTS milestones for 2020 is elimination of malaria in at least 10 countries that were malaria endemic in 2015. At the current rate of progress, it is likely that this milestone will be reached.
In 2016, WHO identified 21 countries with the potential to eliminate malaria by the year 2020. WHO is working with the governments in these countries – known as “E-2020 countries” – to support their elimination acceleration goals.
Although 11 E-2020 countries remain on track to achieve their elimination goals, 10 have reported increases in indigenous malaria cases in 2017 compared with 2016.
Challenges in getting the malaria response back on track
The challenges facing the global malaria response are many, and as highlighted in this year’s report, immediate barriers to achieving the fast-approaching GTS milestones for 2020 and 2025 are malaria’s continued rise in countries with the highest burden of the disease and inadequate international and domestic funding. At the same time, the continued emergence of parasite resistance to antimalarial medicines and mosquito resistance to insecticides pose threats to progress.
High-burden countries
In 2017, 11 countries accounted for approximately 70% of estimated malaria cases and deaths globally: 10 in sub-Saharan Africa and India. Among these countries, only India reported progress in reducing its malaria cases in 2017 compared to 2016.
To get the global malaria response back on track, a new country-driven approach – “High burden to high impact” – will be launched in Mozambique on 19 November 2018, alongside the release of the World malaria report 2018.
Catalyzed by WHO and the RBM Partnership to End Malaria, the approach is founded upon 4 pillars: galvanize national and global political attention to reduce malaria deaths; drive impact in country through the strategic use of information; establish best global guidance, policies and strategies suitable for all malaria endemic countries; and implement a coordinated country response.
Funding
In 24 out of 41 high-burden countries, which rely mainly on external funding for malaria programmes, the average level of funding available per person at risk declined in 2015–2017 compared to 2012–2014. This ranged from a 95% reduction in the Congo (highest) to a 1% decrease in Uganda (lowest) over the time points compared.
In the countries that experienced a 20% or more decrease in total funding per person at risk, international financing declined, at times combined with lower domestic investments.
Among the 41 high-burden countries, overall, funding per person at risk of malaria stood at US$ 2.32.
Drug resistance
ACTs have been integral to the recent success of global malaria control, and protecting their efficacy for the treatment of malaria is a global health priority.
Most studies conducted between 2010 and 2017 show that ACTs remain effective, with overall efficacy rates greater than 95% outside the Greater Mekong subregion (GMS). In Africa, artemisinin (partial) resistance has not been reported to date.
Although multidrug resistance, including artemisinin (partial) resistance and partner drug resistance, has been reported in 4 GMS countries, there has been a massive reduction in malaria cases and deaths in this subregion. Monitoring the efficacy of antimalarial drugs has resulted in prompt updating of malaria treatment policies in most GMS countries.
Insecticide resistance
The recently released WHO Global report on insecticide resistance in malaria vectors: 2010– 2016 showed that resistance to the four commonly used insecticide classes – pyrethroids, organochlorines, carbamates and organophosphates – is widespread in all major malaria vectors across the WHO regions of Africa, the Americas, South-East Asia, the Eastern Mediterranean and the Western Pacific.
Of the 80 malaria endemic countries that provided data for 2010–2017, resistance to at least 1 of the 4 insecticide classes in 1 malaria vector from 1 collection site was detected in 68 countries, an increase over 2016 due to improved reporting and 3 new countries reporting on resistance for the first time. In 57 countries, resistance to 2 or more insecticide classes was reported.
Resistance to pyrethroids – the only insecticide class currently used in ITNs – is widespread and was detected in at least 1 malaria vector in more than two thirds of the sites tested and was highest in the WHO regions of Africa and the Eastern Mediterranean.
Resistance to organochlorines was detected for at least 1 malaria vector in almost two thirds of the sites and was highest in the WHO South-East Asia Region. Resistance to carbamates and organophosphates was less prevalent and was detected in 33% and 27% of the tested sites, respectively. Prevalence was highest for carbamates in the WHO South-East Asia Region and for organophosphates in the WHO Western Pacific Region.
In view of the current situation, resistance monitoring and management plans are essential, in line with the WHO Global plan for insecticide resistance management in malaria vectors. To date, 40 countries have completed these plans.
ITNs continue to be an effective tool for malaria prevention, even in areas where mosquitoes have developed resistance to pyrethroids. This was evidenced in a large multicountry evaluation coordinated by WHO between 2011 and 2016 across study locations in 5 countries.