Archive for December, 2015
Lashkar-e-Jhangvi, a banned Sunni extremist group, claimed responsibility for the attack in which at least 22 people were killed and 50 wounded when a bomb tore through a Pakistani marketplace
Monday, December 14th, 2015Russia: At least 23 people have been killed and dozens left injured in a fire at a neurological hospital in the village of Alferovka
Sunday, December 13th, 201551 saved.
A bomb explosion in a market Sunday killed 12 and injured over 30 others in Pakistan near the Afghan border
Sunday, December 13th, 2015NASA: Fires Put a Carbon Monoxide Cloud over Indonesia
Sunday, December 13th, 2015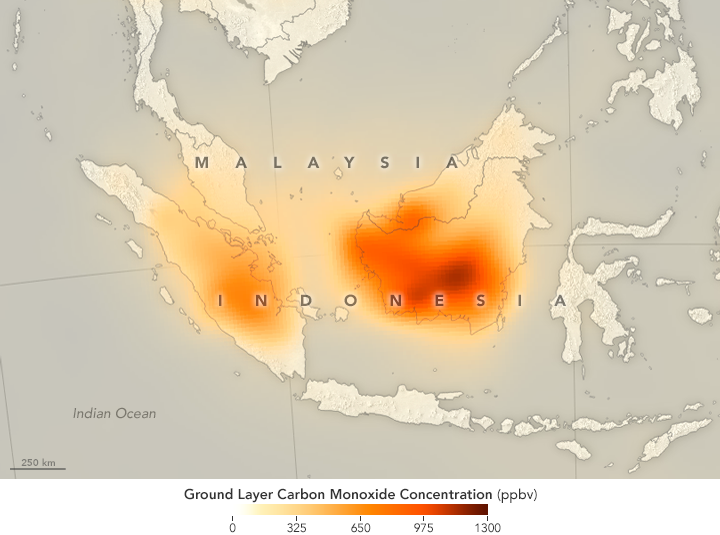
In September and October 2015, tens of thousands of fires sent clouds of toxic gas and particulate matter into the air over Indonesia. Despite the moist climate of tropical Asia, fire is not unusual during those months. For the past few decades, people have used fire to clear land for farming and to burn away leftover crop debris. What was unusual in 2015 was how many fires burned and how many escaped their handlers and went uncontrolled for weeks and even months.
To study the fires, scientists in Indonesia and around the world have been using many different tools—from sensors on the ground to data collected by satellites. The goal is to better understand why the fires became so severe, how they are affecting human health and the atmosphere, and what can be done to prepare for similar surges in fire activity in the future.
While some NASA satellite instruments captured natural-color images of the smoky pall, others focused on gases that are invisible to human eyes. For instance, the Measurement of Pollution in the Troposphere (MOPITT) sensor on Terra can detect carbon monoxide, an odorless, colorless, and poisonous gas. As shown by the map above, the concentration of carbon monoxide near the surface was remarkably high in September 2015 over Sumatra and Kalimantan.
“The 2015 Indonesian fires produced some of the highest concentrations of carbon monoxide that we have ever seen with MOPITT,” said Helen Worden, a scientist at the National Center for Atmospheric Research. Average carbon monoxide concentrations over Indonesia are usually about 100 parts per billion. In some parts of Borneo in 2015, MOPITT measured carbon monoxide concentrations at the surface up to nearly 1,300 parts per billion.
While all types of wildfires emit carbon monoxide as part of he combustion process, the fires in Indonesia released large amounts of the gas because in many cases the fuel burning was peat, a soil-like mixture of partly decayed plant material that builds up in wetlands, swamps, and partly submerged landscapes.
Read more about studies of Indonesia’s fire season in our new feature: Seeing Through the Smoky Pall.
NASA Earth Observatory map by Joshua Stevens and Jesse Allen, using data from the MOPITT Teams at the National Center for Atmospheric Research and the University of Toronto. Caption by Adam Voiland.
- Instrument(s):
- Terra – MOPITT
How many really died during Hajj three months ago?
Saturday, December 12th, 2015
** 2,411 killed was based on what the AP described as its updated compilation from state news reports and official remarks from 36 of the more than 180 countries where pilgrims had traveled from.
** The Saudis claim that 769 pilgrims died in the stampede.
Lyon, France – December 9, 2015 – Sanofi Pasteur, the vaccines division of Sanofi, announced today that the Mexican authorities have granted marketing authorization to Dengvaxia®, making it the first vaccine to be licensed in the world for the prevention of dengue.
Friday, December 11th, 2015Lyon, France – December 9, 2015 – “Sanofi Pasteur, the vaccines division of Sanofi, announced today that the Mexican authorities have granted marketing authorization to Dengvaxia®, making it the first vaccine to be licensed in the world for the prevention of dengue.
The Federal Commission for the Protection against Sanitary Risks (COFEPRIS) has approved Dengvaxia®, tetravalent dengue vaccine, for the prevention of disease caused by all four dengue virus serotypes in preadolescents, adolescents and adults, 9 to 45 years of age living in endemic areas…..
The COFEPRIS approval of Dengvaxia® is based on results from an extensive clinical development program involving over 40,000 people of different ages, geographic and epidemiological settings, and ethnic and socio-economic backgrounds living in 15 countries. Dengue-endemic regions of Mexico participated in all three phases of the clinical development program for the vaccine…..Disease impact modelling results indicate if you vaccinate 20% of the population in the 10 endemic countries that participated in the Phase III efficacy studies for Dengvaxia, in the ages 9 and above indication, you could potentially reduce your dengue burden by 50% in five years. Such a significant disease reduction in this large at-risk population would result in a smaller pool of infected individuals in a given country and, therefore, fewer mosquitoes capable of transmitting the disease, potentially leading to an overall lowering of transmission risk for all…….”
Milestone international conference to target global elimination of dog-mediated human rabies
Friday, December 11th, 2015WHO hosts milestone international conference to target global elimination of dog-mediated human rabies
Global Elimination of Dog-mediated Human Rabies – The Time is Now

30 November 2015 | Geneva –– Rabies kills tens of thousands of people every year. Yet we have the means and the strategic knowledge to prevent dog-mediated human rabies. This will be the key message of an international conference to be hosted by WHO, the World Organisation for Animal Health (OIE) and the Food and Agriculture Organization of the United Nations (FAO), with the support of the Global Alliance for Rabies Control (GARC), at WHO headquarters in Geneva, Switzerland, on 10–11 December 2015.
The first event of its kind, the conference will be instrumental in securing the required support to advance the goal of global elimination of rabies by 2030.
“This meeting will be crucial to setting the stage for intersectoral collaboration and to achieving the global elimination of this preventable disease,” says Dr Bernadette Abela-Ridder, Team Leader, Neglected Zoonotic Diseases, WHO.
Rabies disproportionately affects rural and socio-economically disadvantaged communities of Africa and Asia, where awareness of the disease, access to dog vaccination programmes and appropriate post-bite treatment are limited or non-existent. Lack of rabies awareness and resources make the difference between life and death: rabies is fatal if not treated before symptoms appear.
Proof-of-concept projects demonstrate that rabies control strategies are effective and feasible. More than 95% of human rabies cases result from the bite of a rabid dog. Human rabies cases can be eliminated at source by vaccinating dogs and raising public awareness about dog bite prevention. These measures should be complemented by providing access to correct bite wound management and post-exposure prophylaxis when required.
“We’ve shown that mass vaccination of dogs can eliminate canine rabies,” says Dr Kevin Le Roux, Rabies Programme Manager, KwaZulu-Natal, South Africa. “We have demonstrated success, which has spurred interest in neighbouring countries. Stimulus packages consisting of vaccines and vaccination campaign equipment, coupled with training, allow countries to kick-start a programme. The result is a significant drop in human deaths. Investments for these stimulus packages are needed to roll out elimination programmes in affected communities and countries.”
Drawing on the results of successful WHO proof-of-concept rabies control programmes implemented using a One Health approach, the conference will rally countries and the wider support networks to assume the challenge of investing in global rabies elimination.
The international conference will make the case that elimination of rabies is feasible. It will include next steps on making dog and human vaccines and rabies immunoglobulins more accessible to catalyse progress. An estimated 300 participants will attend, including members of national health ministries and veterinary services, experts from the veterinary and human health sectors, international organizations, policy-makers, nongovernmental organizations, donors, national rabies coordinators and the private sector. All have a role to play in achieving the shared goal of global rabies elimination. The Time is Now!
New global framework to eliminate rabies
Friday, December 11th, 2015
Geneva, 10 December 2015 – A new framework to eliminate human rabies and save tens of thousands of lives each year has been launched today by the World Health Organization (WHO), the World Organisation for Animal Health (OIE), the Food and Agriculture Organization of the United Nations (FAO) and the Global Alliance for the Control of Rabies (GARC).
The framework calls for three key actions – making human vaccines and antibodies affordable, ensuring people who get bitten receive prompt treatment, and mass dog vaccinations to tackle the disease at its source.
“Rabies is 100% preventable through vaccination and timely immunization after exposure, but access to post bite treatment is expensive and is not affordable in many Asian and African countries. If we follow this more comprehensive approach, we can consign rabies to the history books,” says WHO Director-General Dr Margaret Chan.
Tens of thousands of people die from rabies each year and, worldwide, 4 out of every 10 people bitten by suspected rabid dogs are children aged under 15 years. One person dies every 10 minutes, with the greatest burden in Asia and Africa.
The cost of human vaccines to protect from rabies is, however, beyond the reach of many of those who may need it. And treatment for people who are bitten can cost US$ 40–50, representing an average of 40 days of wages in some of the affected countries. Recognizing that human vaccination is currently not always affordable, the new framework emphasizes prevention through vaccinating dogs – whose bites cause 99% of all human rabies cases. A dog vaccine costs less than US$1.
“Vaccinating 70% of dogs regularly in zones where rabies is present can reduce human cases to zero. Eliminating canine rabies through dog vaccination is the most cost-effective and only long-term solution,” states OIE Director General Dr Bernard Vallat. “Human deaths can be prevented when mass dog vaccination is combined with responsible pet ownership and stray dog population management, both complying with OIE intergovernmental standards, as well as with bite treatment, as recommended by WHO.”
Whilst vaccinating dogs will be key in the new approach, the elimination of rabies – and saving the lives of those who are bitten – will not be possible without more widely-available human vaccines.
Currently, about 80% of people exposed to rabies live in poor, rural areas of Africa and Asia with no access to prompt treatment should they be bitten. Bringing treatment closer to victims and providing wider access to affordable vaccines and potent rabies immunoglobulins, which neutralize the rabies virus before it can get a hold in the body, are vital to achieving zero rabies deaths.
Bringing down the cost of human rabies vaccines and treatments will require strong international collaboration to make quality-assured vaccines and rabies immunoglobulin available to health centres in regions where rabies is endemic.
As of 2015, WHO and the OIE Vaccine Bank have delivered more than 15 million doses of canine rabies vaccines in many countries.
Global elimination of human rabies – The time is now!
On 10 and 11 December 2015, experts, donors, and veterinary and public health officials will adopt a plan of action that is expected to deliver prompt post-exposure prophylaxis for all in rabies endemic areas as well as a framework for scaling up sustained, large-scale dog vaccination. This milestone international conference will also discuss a push for coordinated activities targeting dog and human populations by adapting proven control strategies.
Another important component is harnessing support for community awareness and engagement to facilitate and strengthen data collection, bite incidence reporting and demand for post-exposure prophylaxis. Educating children on how to avoid being bitten is also vital.
The conference “Global elimination of dog-mediated human rabies – The time is now” is jointly organized by WHO and the OIE, in collaboration with FAO with the support of GARC.
For media inquiries, please contact:
Christian Lindmeier
WHO Department of Communications
Telephone: +41 79 500 65 52+41 79 500 65 52
Mobile: +41 7 94 45 31 64+41 7 94 45 31 64
Email: lindmeierch@who.int
Dr Catherine Bertrand-Ferrandis
Head of Communication
World Organisation for Animal Health
Mobile: +33 6 16 46 28 90+33 6 16 46 28 90
Email : c.bertrand-ferrandis@oie.int