Archive for the ‘Diphtheria’ Category
WHO: A diphtheria outbreak in Yemen has spread rapidly nationwide and infected more than 1,300 people and over 70 deaths
Tuesday, March 20th, 2018“…..The near three-year stalemated war has damaged Yemen’s infrastructure, crippled the health system and pushed it to the brink of famine…..”
Rohingya: From 3 November 2017 through 12 December 2017, a total of 804 suspected diphtheria cases including 15 deaths were reported among the displaced Rohingya population in Cox’s Bazar.
Thursday, December 14th, 2017Diphtheria – Cox’s Bazar in Bangladesh
From 3 November 2017 through 12 December 2017, a total of 804 suspected diphtheria cases including 15 deaths were reported among the displaced Rohingya population in Cox’s Bazar (Figure 1). The first suspected case was reported on 10 November 2017 by a clinic of Médecins Sans Frontières (MSF) in Cox’s Bazar.
Figure 1: Number of diphtheria cases among the displaced Rohingya population in Cox’s Bazar, Bangladesh reported by date of illness onset from 3 November 2017 through 12 December 20171
1Date of onset information is missing for 45 (5.6%) cases.
Source: Médecins Sans Frontières
Of the suspected cases, 73% are younger than 15 years of age and 60% females (the sex for one percent cases was not reported). Fourteen of 15 deaths reported among suspected diphtheria cases were children younger than 15 years of age. To date, no cases of diphtheria have been reported from local communities.
Public health response
Since August 2017, more than 646 000 people from neighbouring Myanmar have gathered in densely populated camps and temporary settlements with poor access to clean water, sanitation and health services. A multi-agency diphtheria task force, led by the Ministry of Health Family Welfare of Bangladesh, has been providing clinical and public health services to the displaced population. WHO has mobilized US$ 3 million from its Contingency Fund for Emergencies (CFE) to support essential health services in Bangladesh.
WHO is working with health authorities to provide tetanus diphtheria (Td) vaccines for children aged seven to 15 years, as well as pentavalent vaccines (diphtheria, pertussis, tetanus, Haemophilus influenzae type b, and hepatitis B) and pneumococcal conjugate vaccines (PCV) for children aged six weeks to six years. A list of essential medicines and required supplies to support the response is being finalized by WHO and partners.The Serum Institute of India has donated 300 000 doses of pentavalent vaccines for use in the response.
WHO risk assessment
The current outbreak in Cox’s Bazar is evolving rapidly. To date, all suspected cases have occurred among the displaced Rohingya population, who are living in temporary settlements with difficult and crowded conditions. The coverage of diphtheria toxoid containing vaccines among the displaced Rohingya population is difficult to estimate, although diphtheria outbreaks are an indication of low overall population vaccination coverage. Available vaccination data for Bangladesh indicates that the coverage of diphtheria toxoid containing vaccines is high. However, spillover into the local population cannot be ruled out. WHO considers the risk at the national level to be moderate and low at the regional and global levels.
WHO advice
WHO recommends timely clinical management of suspected diphtheria cases that is consistent with WHO guidelines consisting of diphtheria antitoxin, appropriate antibiotics and implementation of infection prevention and control measures. High-risk populations such as young children, close contacts of diphtheria cases, and health workers should be vaccinated on priority basis. A coordinated response and community engagement can reduce the risk of further transmission and help to control the outbreak.
For more information on diphtheria, please see the link below:
Rohingya: Diphtheria is spreading fast in Cox’s Bazar, Bangladesh
Thursday, December 7th, 2017
6 December 2017 | Geneva – Diphtheria is rapidly spreading among Rohingya refugees in Cox’s Bazar, Bangladesh, WHO warned today.
More than 110 suspected cases, including 6 deaths, have been clinically diagnosed by health partners, including Médecins Sans Frontières (MSF) and the International Federation of the Red Cross (IFRC).
“These cases could be just the tip of the iceberg. This is an extremely vulnerable population with low vaccination coverage, living in conditions that could be a breeding ground for infectious diseases like cholera, measles, rubella, and diphtheria,” said Dr Navaratnasamy Paranietharan, WHO Representative to Bangladesh.
“This is why we have protected more than 700,000 people with the oral cholera vaccine, as well as more than 350,000 children with measles-rubella vaccine in a campaign that ended yesterday. Now we have to deal with diphtheria.”
Since August 2017, more than 624,000 people fleeing violence in neighbouring Myanmar have gathered in densely populated temporary settlements with poor access to clean water, sanitation and health services – and the numbers continue to swell.
WHO is working with the Bangladesh Ministry of Health and Family Welfare, UNICEF and partners to contain the spread of the highly infectious respiratory disease through effective treatment and adequate prevention.
Together, they are supporting patient diagnosis and treatment, ensuring adequate supplies of medicines, and preparing a vaccination campaign targeting all children up to 6 years with pentavalent (DPT-HepB-Hib) and pneumococcal vaccines, which protect against diphtheria and other diseases. Training is already underway for vaccinators.
WHO has procured an initial 1,000 vials of diphtheria antitoxins that are due to arrive in Bangladesh by the weekend. Combined with antibiotics, the antitoxins can save the lives of people already infected with diphtheria, by neutralizing the toxins produced by the deadly bacteria.

“We are working with partners to ensure that clinical guidance is available to health workers, and that there are enough beds and medicines for those who get sick. But the only way to control this outbreak is to protect people, particularly children, through vaccination,” said Dr Paranietharan.
WHO: Hundreds of thousands of Rohingya refugees who fled from Myanmar into Bangladesh are at risk from a possible outbreak of diphtheria
Wednesday, November 29th, 2017“…..The WHO describes diphtheria as a widespread, severe infectious disease that has the potential for epidemics, with a mortality rate of up to 10 percent…..”
Diphtheria once was a major cause of illness and death among children. The United States recorded 206,000 cases of diphtheria in 1921, resulting in 15,520 deaths. Starting in the 1920s, diphtheria rates dropped quickly due to the widespread use of vaccines. Between 2004 and 2015, 2 cases of diphtheria were recorded in the United States. However, the disease continues to cause illness globally. In 2014, 7,321 cases of diphtheria were reported worldwide to the World Health Organization, but many more cases likely go unreported.
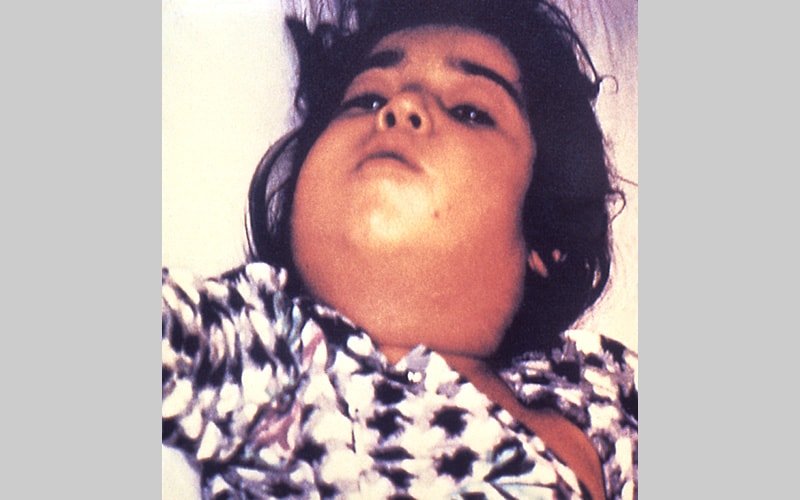
The case-fatality rate for diphtheria has changed very little during the last 50 years. The overall case-fatality rate for diphtheria is 5%–10%, with higher death rates (up to 20%) among persons younger than 5 and older than 40 years of age. Before there was treatment for diphtheria, the disease was fatal in up to half of cases.
Clinical Features
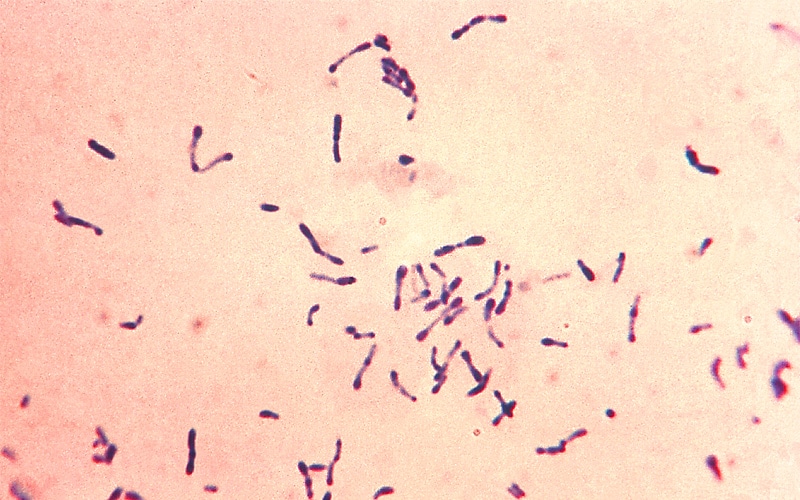
The incubation period of diphtheria is 2–5 days (range: 1–10 days). Diphtheria can involve almost any mucous membrane. For clinical purposes, it is convenient to classify diphtheria into a number of manifestations, depending on the site of disease:
- Respiratory diphtheria
- Nasal diphtheria
- Pharyngeal and tonsillar diphtheria
- Laryngeal diphtheria
- Cutaneous diphtheria
Clinician Resources
- Checklist for Assessing a Patient with Suspected Diphtheria[2 pages](https://www.cdc.gov/diphtheria/downloads/dip-cklist-diag.pdf)
- Diphtheria Investigation—Worksheet[2 pages](https://www.cdc.gov/diphtheria/downloads/dip-wksht.pdf)
- Information for Close Contacts of a Diphtheria Patient—Worksheet[2 pages](https://www.cdc.gov/diphtheria/downloads/close-contacts.pdf)
Medical Management
After the provisional clinical diagnosis is made and appropriate cultures are obtained, persons with suspected diphtheria should be given antitoxin and antibiotics in adequate dosage and placed in isolation. Respiratory support and airway maintenance should also be administered as needed.
Diphtheria Antitoxin
In the United States, diphtheria antitoxin can be obtained from CDC on request. Learn more about diphtheria antitoxin and how to request it(https://www.cdc.gov/diphtheria/dat.html).
Antibiotics
The recommended antibiotic treatment for diphtheria is erythromycin orally or by injection (40 mg/kg/day; maximum, 2 gm/day) for 14 days, or procaine penicillin G daily, intramuscularly (300,000 units every 12 hours for those weighing 10 kg or less, and 600,000 units every 12 hours for those weighing more than 10 kg) for 14 days. Oral penicillin V 250 mg 4 times daily is given instead of injections to persons who can swallow. The disease is usually not contagious 48 hours after antibiotics are instituted. Elimination of the organism should be documented by two consecutive negative cultures after therapy is completed.
Preventive Measures

For close contacts, especially household contacts, a diphtheria toxoid booster, appropriate for age, should be given. Contacts should also receive antibiotics—a 7- to 10-day course of oral erythromycin (40 mg/kg/day for children and 1 g/day for adults). For compliance reasons, if surveillance of contacts cannot be maintained, they should receive benzathine penicillin (600,000 units for persons younger than 6 years old and 1,200,000 units for those 6 years and older). Identified carriers in the community should also receive antibiotics. Contacts should be closely monitored and antitoxin given at the first sign(s) of illness.
Contacts of cutaneous diphtheria should be treated as described above; however, if the strain is shown to be nontoxigenic, investigation of contacts can be discontinued.
Challenges
Circulation of the bacteria appears to continue in some settings, even in populations with more than 80% childhood immunization rates. An asymptomatic carrier state can exist even among immune individuals.
Immunity wanes over time and a booster dose of vaccine should be administered every 10 years to maintain protective antibody levels. Large populations of older adults may be susceptible to diphtheria, in both developed as well as in developing countries.
In countries with low disease incidence, the diagnosis may not be considered by clinicians and laboratory scientists. Prior antibiotic treatment can prevent recovery of the organism. Because the disease is rarely seen in developed countries, most physicians will never have seen a case of diphtheria in their lifetime. There is limited epidemiologic, clinical, and laboratory expertise on diphtheria.
Surveillance
National surveillance is conducted through the National Notifiable Diseases Surveillance System. Cases are also identified by requests for diphtheria antitoxin (DAT); since 1997, DAT is available for U.S. healthcare professionals only through CDC.
WHO: Diphtheria has infected at least 120 people since early November, and this will only worsen if health facilities don’t get the fuel they need. At least one million children are at risk of contracting the disease if vaccines and medicine continue to be denied entry
Sunday, November 26th, 2017“…..Eight million people in Yemen will be without running water within days as fuel runs out due to the Saudi-led coalition blockade of the country’s northern ports…….
They will join the almost 16 million people in Yemen who already cannot get clean piped water, leaving more than four in five people without a steady supply of clean water…..”