Archive for the ‘Tuberculosis’ Category
Prevalence of Tuberculosis in Children After Natural Disasters: The Philippines
Monday, September 23rd, 2019Murray, K. O., Castillo-Carandang, N. T., Mandalakas, A. M., Cruz, A. T., Leining, L. M., & Gatchalian, S. R. (2019). Prevalence of Tuberculosis in Children After Natural Disasters, Bohol, Philippines. Emerging Infectious Diseases, 25(10), 1884-1892. https://dx.doi.org/10.3201/eid2510.190619.
“In 2013, a severe earthquake and typhoon affected Bohol, Philippines. To assess the postdisaster risk for emergence of Mycobacterium tuberculosis infection in children, we conducted a cross-sectional multistage cluster study to estimate the prevalence of tuberculin skin test (TST) positivity and tuberculosis (TB) in children from 200 villages in heavily affected and less affected disaster areas. Of the 5,476 children we enrolled, 355 were TST-positive (weighted prevalence 6.4%); 16 children had active TB. Fourteen (7%) villages had >20% TST-positive prevalence. Although prevalence did not differ significantly between heavily affected and less affected areas, living in a shelter with >25 persons approached significance. TST positivity was independently associated with older age, prior TB treatment, known contact with a person with TB, and living on a geographically isolated island. We found a high TST-positive prevalence, suggesting that national programs should consider the differential vulnerability of children and the role of geographically isolated communities in TB emergence.”
https://youtu.be/9112brXCOVc
World TB Day — March 24, 2019.
Saturday, March 23rd, 2019World TB Day — March 24, 2019. MMWR Morb Mortal Wkly Rep 2019;68:257. DOI: http://dx.doi.org/10.15585/mmwr.mm6811a1.
“…..In 2018, a provisional total of 9,029 TB cases were reported in the United States (incidence = 2.8 cases per 100,000 persons) (1), a decline from the 9,094 cases reported in 2017 and the lowest number of cases on record in the United States since reporting began in 1953. Increased diagnosis and treatment of latent TB infection remains essential to eliminating TB in the United States.
Worldwide, an estimated 10 million cases of TB were reported in 2017, a decline of 1.8% from 2016. Approximately 1.57 million persons died from TB in 2017, a 3.9% decrease from 2016….”
WHO: Drug-resistant TB a ‘public health crisis’
Monday, October 1st, 2018The report (WHO Global TB Report 2018 ) also highlights the continuing crisis of multidrug-resistant TB (MDR-TB).
- 558,000 people in 2017 developed TB that was resistant to rifampicin, the most effective first-line TB drug;
- 82% of these cases were MDR-TB
- 8.5% were extensively drug-resistant TB (XDR-TB).
- Nearly half of the world’s MDR-TB cases are in India (24%), China (13%), and Russia (10%).
https://youtu.be/9112brXCOVc
World leaders meeting today at the United Nations (UN) General Assembly have committed to ensure that 40 million people with tuberculosis (TB) receive the care they need by end 2022.
Thursday, September 27th, 2018World leaders meeting today at the United Nations (UN) General Assembly have committed to ensure that 40 million people with tuberculosis (TB) receive the care they need by end 2022. They also agreed to provide 30 million people with preventive treatment to protect them from developing TB.
“Today is a landmark in the long war on TB,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization. “These are bold promises – to keep them partnership is vital. WHO is committed to working with every country, every partner and every community to get the job done.”
Heads of state and government attending this first-ever UN High-level meeting on TB agreed to mobilize US$ 13 billion a year by 2022 to implement TB prevention and care, and US$ 2 billion for research. They committed to take firm action against drug-resistant forms of the disease; build accountability and to prioritize human rights issues such as the stigma that still prevails around TB in many parts of the world.
They acknowledged that the current rate of progress was endangering prospects of meeting global targets to end TB. Today, TB remains the world’s deadliest infectious disease: it killed 1.6 million people in 2017, including 300 000 people with HIV. In the same year, 10 million people fell ill with TB.
“The political declaration proposed for this meeting sets a roadmap for accelerated action to end TB in line with the vision and targets for 2030,” said H.E. Ms Maria Fernanda Espinosa Garcés, President of the 73rd Session of the UN General Assembly. “We have before us the opportunity for a clear win – a chance to save the lives of millions, to preserve billions in resources, to demonstrate the success of the Sustainable Development Goals, and to reaffirm the utility, efficacy and necessity of multilateralism and the UN System. Let us not miss this opportunity.”
The political declaration is the culmination of recent leadership commitments at global and regional level – including the 2017 Moscow Declaration to End TB – to drive universal access, sufficient and sustainable financing, intensified research and innovation, and accountability across all sectors.
WHO: The number of new tuberculosis (TB) cases continued to decline in 2017, but we must do better
Friday, September 21st, 2018WHO Global TB Report 2018 : Document
TB is an old disease that was once a death sentence. Effective drug treatments first became available in the 1940s, and in combination with social and economic development they allowed countries in western Europe, North America and some other parts of the world to reduce their burden of TB disease to very low levels.13 For most countries, however, the “end” of TB as an epidemic and major public health problem remains an aspiration rather than a reality. The UN high-level meeting on TB on 26 September 2018, with attendance of heads of state and other eminent people, provides a platform to step up the commitments and actions needed to end the global TB epidemic, by the SDG deadline of 2030.
“…..The 2018 edition of the WHO’s annual TB report estimates that 10 million people developed the disease in 2017, including 5.8 million men, 3.2 million women, and 1 million children. That’s down from 10.4 million in 2016. Globally, the TB incidence rate is falling by roughly 2% a year, with annual reductions of 5% and 4% in Europe and Africa, respectively.
But the report says the global incidence rate needs to be falling by 4-5% every year to meet the first milestone of the End TB strategy—a 20% reduction by 2020 (compared with 2015). The strategy aims to cut TB incidence by 80% by 2030…..”
NIH Statement on World Tuberculosis Day 2018
Saturday, March 24th, 2018Friday, March 23, 201
Statement of Christine F. Sizemore, Ph.D., Richard Hafner, M.D., and Anthony S. Fauci, M.D.
Mtb is transmitted through the air and primarily affects the lungs. TB is the leading killer among infectious diseases and among the top 10 causes of death worldwide. The World Health Organization (WHO) estimates that in 2016, TB claimed the lives of 1.7 million people, including 250,000 children, and 10.4 million people were newly infected with Mtb. TB is the primary cause of death for individuals co-infected with HIV. According to the WHO, more than 2 billion people globally are “latently” infected with TB, meaning they carry the bacteria but are currently without symptoms, which would include cough, fever, weight loss and night sweats. People with latent TB infection cannot actively transmit TB bacteria to another person. Up to 13 million people in the United States are estimated to have latent TB infection, according to the U.S. Centers for Disease Control and Prevention. Overall, people with latent TB infection have a 5 to 15 percent lifetime risk of developing active TB disease. This risk increases for people with compromised immune systems, such as those living with HIV, people receiving immunosuppressive therapy (such as individuals being treated for cancer), as well as diabetics, smokers and the malnourished.
WHO’s End TB Strategy envisions an end to TB by 2035. To accomplish this, incremental improvements in understanding the disease and in the tools used to identify, treat, and prevent it will not be sufficient. Rather, accelerated efforts and transformative advances are needed. Recent engagement includes NIAID participation in the first “WHO Global Ministerial Conference on Ending TB in the Sustainable Development Era: A Multisectoral Response” in Moscow. At this November 2017 meeting, the urgent need for a more intensive biomedical research approach to controlling and ultimately eliminating TB was clearly articulated. Specifically, we need a more intensive interdisciplinary systems biology approach (using cutting-edge methods, large data sets, and modeling to understand complex biological systems) to improve our understanding of how Mtb infection causes disease. Additionally, we must work toward improved diagnostics that can detect Mtb in a variety of clinical specimens in addition to sputum. Also, rapid, accurate, and inexpensive “point-of-care” tests to distinguish between drug-sensitive and drug-resistant Mtb must be developed. NIAID investments in research contributed substantially to the WHO-endorsed GeneXpert MTB/rifampicin resistance diagnostic currently in use, and the Institute continues to support the development of next-generation TB diagnostics.
Today’s treatment regimens for TB require too many drugs, often with toxic side effects, that must be taken for six months or longer. With the increasing incidence of multidrug resistant TB (MDR-TB), these regimens often become very lengthy (up to 20 months), more complex, costly, and more prone to failure. Extensively drug-resistant TB (XDR-TB) is even more difficult to treat, and for some patients, no effective treatment regimens exist. Despite the urgent need for new and improved TB treatments, there is a paucity of new drugs in the clinical development pipeline. To address this deficit, NIAID-supported investigators have engaged in cross-disciplinary, international collaborations designed to spur basic science and early-stage TB drug discovery. Additionally, NIAID has used its HIV/AIDS clinical trials networks to enhance TB clinical research by conducting key studies of potential TB treatment strategies. For example, a NIAID-led study found that a one-month antibiotic regimen to prevent active TB disease in people with latent TB infection was as safe and effective as the standard 9-month course in people living with HIV. Additionally, the NIAID-funded HIV/AIDS clinical trials networks have conducted studies of improved regimens for MDR-TB therapeutics geared to treat both HIV-infected and uninfected adults and children.
A broadly effective preventive TB vaccine could avert millions of new Mtb infections; however, critical knowledge gaps have made developing such a vaccine a difficult challenge. The current Bacille Calmette-Guerin (BCG) vaccine, developed in 1921, offers protection against disseminated TB disease and death in children, but this protection does not reliably extend into adulthood. A recent study suggests that revaccination with the vaccine could potentially prevent Mtb infections in high-risk adolescents. To reliably protect against the transmissible pulmonary form of the disease in adults, a new, more effective intervention strategy is needed. NIAID supports basic, preclinical and clinical research to find and develop new, innovative vaccines to prevent TB infection and disease.
The WHO estimates that 53 million lives were saved between 2000 and 2016 through improved TB diagnosis and treatment. Through an intensified research agenda, a sustained commitment to supporting and conducting TB research, and a renewed effort to work with other agencies and organizations, NIAID is dedicated to helping eliminate this disease and improving and saving the lives of people with TB. In September 2018, the United Nations General Assembly will conduct a high-level meeting on TB—representing an important step forward by governments and other partners from around the world in the fight against TB. On this World TB Day, we stand with global leaders in response to the bold call of action to make history and end TB.
Anthony S. Fauci, M.D., is Director of the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health in Bethesda, Maryland. Richard Hafner, M.D., is chief of the TB Clinical Research Branch in NIAID’s Division of AIDS; Christine F. Sizemore, Ph.D., is chief of the Tuberculosis and other Mycobacterial Diseases Section in the NIAID Division of Microbiology and Infectious Diseases.
NIAID conducts and supports research — at NIH, throughout the United States, and worldwide — to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website.
March 24: World TB Day
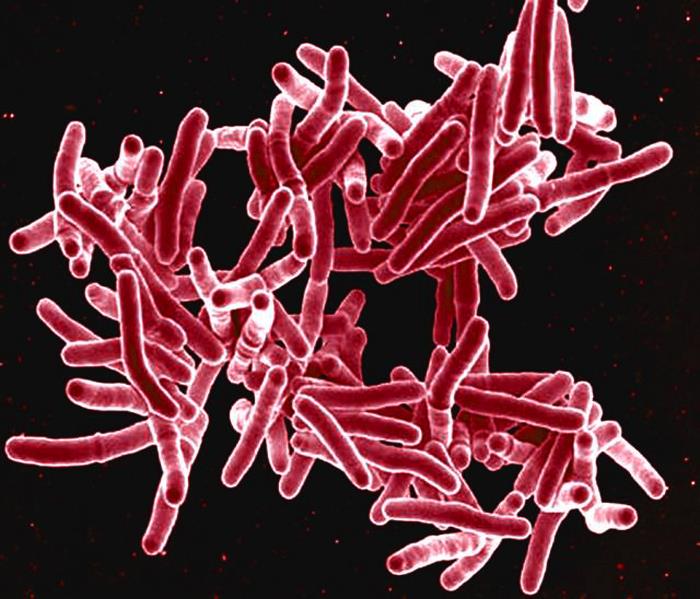
Saturday, March 24th, 2018Each year, we recognize World TB Day on March 24. This annual event commemorates the date in 1882 when Dr. Robert Koch announced his discovery of Mycobacterium tuberculosis, the bacillus that causes tuberculosis (TB).
Although TB is preventable and curable, many people in the United States still suffer from this disease. Anyone can get TB, and our current efforts to find and treat latent TB infection and TB disease are not sufficient. Misdiagnosis of TB still exists and health care professionals often do not “think TB.”
The U.S. theme for World TB Day 2018 is “Wanted: Leaders for a TB Free United States. We can make history. End TB.” CDC and its domestic and international partners, including the National TB Controllers Association, Stop TB USA, and the global Stop TB Partnership are working together to eliminate this deadly disease. But we need your help.
Be sure to check back for more information and resources as we get closer to World TB Day. You can also follow us on Twitter @CDC_TB and Facebook @CDCTB and sign up for email updates through GovDelivery.
Join CDC’s World TB Day Thunderclap, and share the End TB message March 23rd at 2:00 p.m. EDT/11:00 a.m. PDT, spreading an idea through Facebook, Twitter, and Tumblr that cannot be ignored. We need 100 supporters for the Thunderclap to take effect, so please visit http://thndr.me/5APDuS before March 23 to sign up and learn more.
Get Involved in the Fight to End TB:

World TB Day Resources
Download and share World TB Day graphics, messages, social media tools, and more

U.S. TB Champions
Learn how you and your organization can participate in CDC’s TB Elimination Champions project.

World TB Day Activities
Tell us about your community’s World TB Day activities, and see how others are observing.
The incidence of TB among adolescents and young adults around the world
Friday, February 23rd, 2018CDC recommendations to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas during the period of September 2017 – March 2018.
Wednesday, October 25th, 2017Advice for Providers Treating Patients in or Recently Returned from Hurricane-Affected Areas, Including Puerto Rico and US Virgin Islands
Distributed via the CDC Health Alert Network
October 24, 2017, 1330 ET (1:30 PM ET)
CDCHAN-00408
Summary
The Centers for Disease Control and Prevention (CDC) is working with federal, state, territorial, and local agencies and global health partners in response to recent hurricanes. CDC is aware of media reports and anecdotal accounts of various infectious diseases in hurricane-affected areas, including Puerto Rico and the US Virgin Islands (USVI). Because of compromised drinking water and decreased access to safe water, food, and shelter, the conditions for outbreaks of infectious diseases exist.
The purpose of this HAN advisory is to remind clinicians assessing patients currently in or recently returned from hurricane-affected areas to be vigilant in looking for certain infectious diseases, including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. Additionally, this Advisory provides guidance to state and territorial health departments on enhanced disease reporting.
Background
Hurricanes Irma and Maria made landfall in Puerto Rico and USVI in September 2017, causing widespread flooding and devastation. Natural hazards associated with the storms continue to affect many areas. Infectious disease outbreaks of diarrheal and respiratory illnesses can occur when access to safe water and sewage systems are disrupted and personal hygiene is difficult to maintain. Additionally, vector borne diseases can occur due to increased mosquito breeding in standing water; both Puerto Rico and USVI are at risk for outbreaks of dengue, Zika, and chikungunya.
Health care providers and public health practitioners should be aware that post-hurricane environmental conditions may pose an increased risk for the spread of infectious diseases among patients in or recently returned from hurricane-affected areas; including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. The period of heightened risk may last through March 2018, based on current predictions of full restoration of power and safe water systems in Puerto Rico and USVI.
In addition, providers in health care facilities that have experienced water damage or contaminated water systems should be aware of the potential for increased risk of infections in those facilities due to invasive fungi, nontuberculous Mycobacterium species, Legionella species, and other Gram-negative bacteria associated with water (e.g., Pseudomonas), especially among critically ill or immunocompromised patients.
Cholera has not occurred in Puerto Rico or USVI in many decades and is not expected to occur post-hurricane.
Recommendations
These recommendations apply to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas (e.g., within the past 4 weeks), during the period of September 2017 – March 2018.
- Health care providers and public health practitioners in hurricane-affected areas should look for community and healthcare-associated infectious diseases.
- Health care providers in the continental US are encouraged to ask patients about recent travel (e.g., within the past 4 weeks) to hurricane-affected areas.
- All healthcare providers should consider less common infectious disease etiologies in patients presenting with evidence of acute respiratory illness, gastroenteritis, renal or hepatic failure, wound infection, or other febrile illness. Some particularly important infectious diseases to consider include leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza.
- In the context of limited laboratory resources in hurricane-affected areas, health care providers should contact their territorial or state health department if they need assistance with ordering specific diagnostic tests.
- For certain conditions, such as leptospirosis, empiric therapy should be considered pending results of diagnostic tests— treatment for leptospirosis is most effective when initiated early in the disease process. Providers can contact their territorial or state health department or CDC for consultation.
- Local health care providers are strongly encouraged to report patients for whom there is a high level of suspicion for leptospirosis, dengue, hepatitis A, typhoid, and vibriosis to their local health authorities, while awaiting laboratory confirmation.
- Confirmed cases of leptospirosis, dengue, hepatitis A, typhoid fever, and vibriosis should be immediately reported to the territorial or state health department to facilitate public health investigation and, as appropriate, mitigate the risk of local transmission. While some of these conditions are not listed as reportable conditions in all states, they are conditions of public health importance and should be reported.
For More Information
- General health information about hurricanes and other tropical storms: https://www.cdc.gov/disasters/hurricanes/index.html
- Information about Hurricane Maria: https://www.cdc.gov/disasters/hurricanes/hurricane_maria.html
- Information for Travelers:
- Travel notice for Hurricanes Irma and Maria in the Caribbean: https://wwwnc.cdc.gov/travel/notices/alert/hurricane-irma-in-the-caribbean
- Health advice for travelers to Puerto Rico: https://wwwnc.cdc.gov/travel/destinations/traveler/none/puerto-rico?s_cid=ncezid-dgmq-travel-single-001
- Health advice for travelers to the U.S. Virgin Islands: https://wwwnc.cdc.gov/travel/destinations/traveler/none/usvirgin-islands?s_cid=ncezid-dgmq-travel-leftnav-traveler
- Resources from CDC Health Information for International Travel 2018 (the Yellow Book):
- Post-travel Evaluation: https://wwwnc.cdc.gov/travel/yellowbook/2018/post-travel-evaluation/general-approach-to-the-returned-traveler
- Information about infectious diseases after a disaster: https://www.cdc.gov/disasters/disease/infectious.html
- Dengue: https://www.cdc.gov/dengue/index.html
- Hepatitis A: https://www.cdc.gov/hepatitis/HAV/index.htm
- Leptospirosis: https://www.cdc.gov/leptospirosis/
- Typhoid fever: https://www.cdc.gov/typhoid-fever/index.html
- Vibriosis: https://www.cdc.gov/vibrio/index.html
- Information about other infectious diseases of concern:
- Conjunctivitis: https://www.cdc.gov/conjunctivitis/
- Influenza: https://www.cdc.gov/flu/index.htm
- Scabies: https://www.cdc.gov/parasites/scabies/index.html
- Tetanus and wound management: https://www.cdc.gov/disasters/emergwoundhcp.html
- Tetanus in Areas Affected by a Hurricane: Guidelines for Clinicians https://emergency.cdc.gov/coca/cocanow/2017/2017sept12.asp




 CDC: “…
CDC: “…
