Archive for the ‘Naegleria fowleri’ Category
California, 2018: A Case of Fatal Naegleria fowleri Meningoencephalitis
Monday, September 16th, 2019Vugia DJ, Richardson J, Tarro T, et al. Notes from the Field: Fatal Naegleria fowleri Meningoencephalitis After Swimming in Hot Spring Water — California, 2018. MMWR Morb Mortal Wkly Rep 2019;68:793–794. DOI: http://dx.doi.org/10.15585/mmwr.mm6836a3external icon
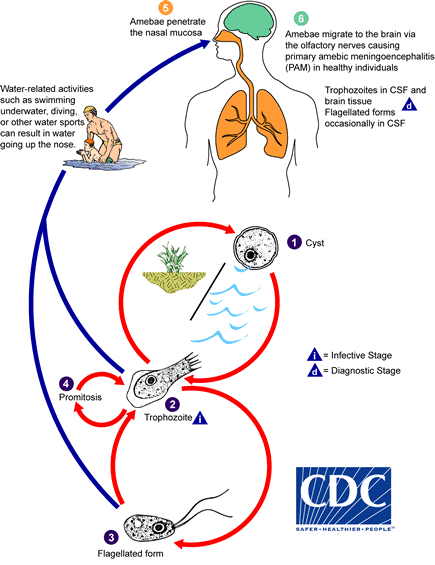
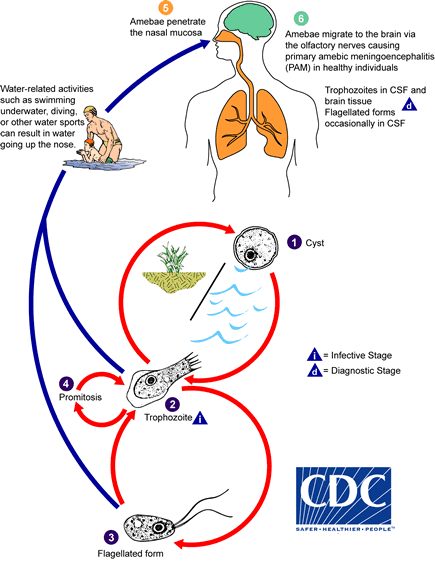
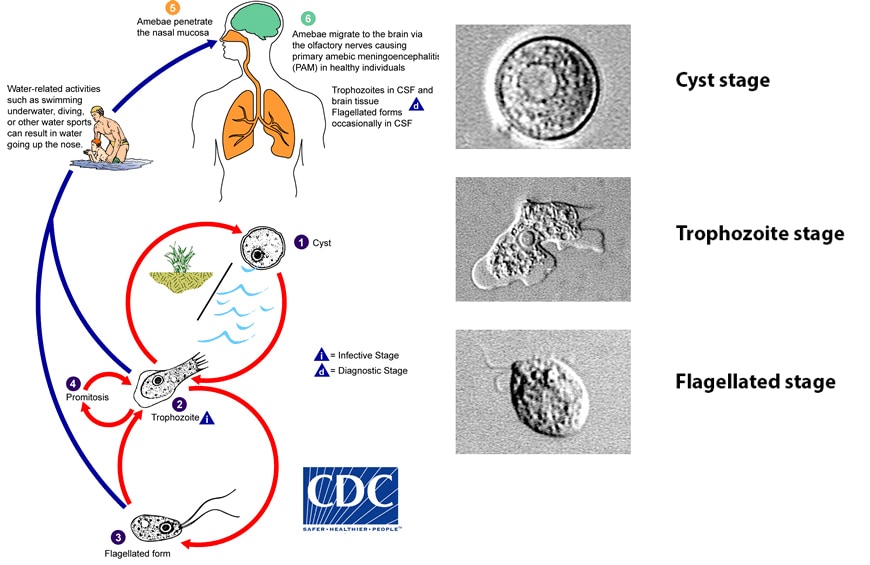
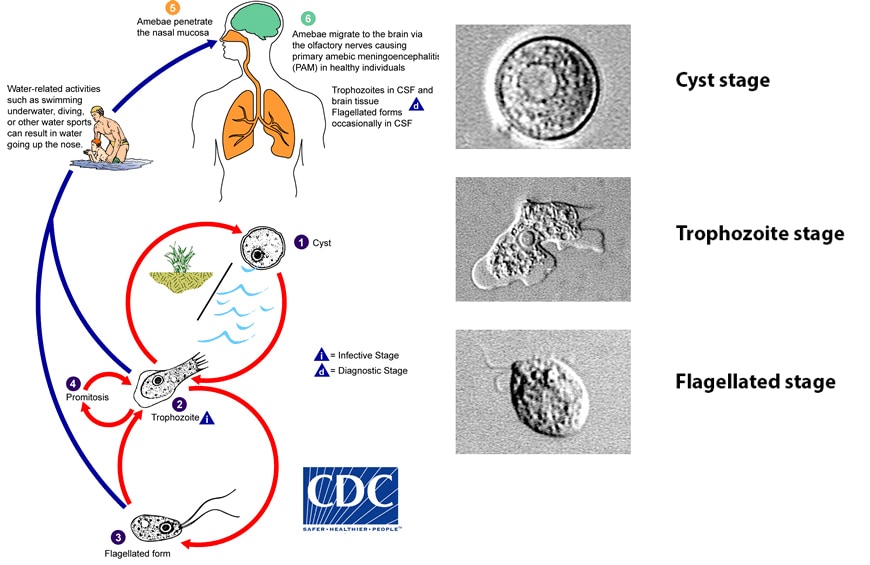
“In October 2018, a previously healthy boy was admitted to an intensive care unit at a southern California hospital after experiencing 2 days of headache, vomiting, and fever and 1 day of altered mental status. He was initially treated empirically for bacterial and viral meningitis and subsequently displayed decreased level of consciousness and experienced respiratory failure, requiring intubation and mechanical ventilation. Computed tomography scan of the brain showed diffuse cerebral edema. A wet mount of cerebrospinal fluid obtained by lumbar puncture revealed amebic organisms consistent with Naegleria species, and a treatment regimen for Naegleria was added, including miltefosine (1), which is now commercially available.* The infectious disease clinician notified CDC, which then notified state and local public health. Polymerase chain reaction testing of a cerebrospinal fluid specimen at the Mayo Clinic on hospital day 2 identified N. fowleri, a free-living ameba found in warm fresh water that causes primary amebic meningoencephalitis (PAM). The patient’s condition continued to worsen, and he died on hospital day 3...…”

Pakistan: 12 people have so far died in 2019 in Karachi due to Naegleria fowleri
Tuesday, August 27th, 2019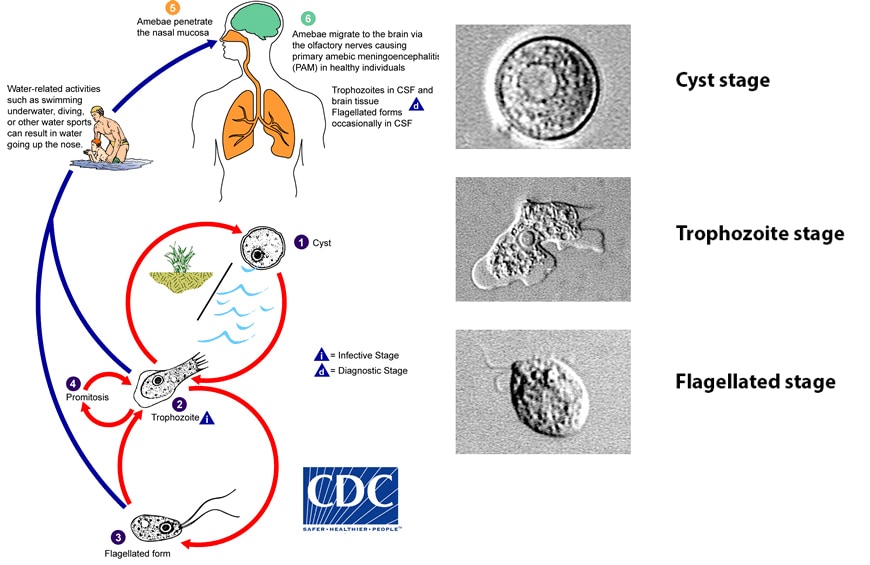
A 34-year old man was infected with Naegleria fowleri is struggling for life at a private hospital in Karachi, Pakistan.
Wednesday, May 22nd, 2019“……Health department officials said Shoaib Ahmed Siddiqui, a resident of the Liaquatabad area, started having a headache and a low-grade fever a couple of days back and, despite taking medicine, his condition deteriorated. He was taken to the emergency of Aga Khan Hospital on Thursday where he was put on life support after his condition worsened and lab tests confirmed he was infected with Naegleria fowleri……”

A 21-year old student died last week of primary amoebic meningoencephalitis (PAM) at the Jinnah Postgraduate Medical Centre (JPMC).
Tuesday, April 23rd, 2019‘…..“A 21-year old student from Orangi Town, Anas Aslam, was brought to JPMC with high-grade fever and other complaints. Doctors suspected meningitis and the patient was shifted to ICU on deterioration in his health. He died yesterday [Friday] due to complications of the disease,” JPMC Executive Director Dr Seemin Jamali told The News on Saturday.
Dr Jamali said they had sent the cerebrospinal fluid (CSF) for analysis and the laboratory report confirmed that the young patient was infected with the lethal Naegleria fowleri infection…….’

CDC recommendations to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas during the period of September 2017 – March 2018.
Wednesday, October 25th, 2017Advice for Providers Treating Patients in or Recently Returned from Hurricane-Affected Areas, Including Puerto Rico and US Virgin Islands
Distributed via the CDC Health Alert Network
October 24, 2017, 1330 ET (1:30 PM ET)
CDCHAN-00408
Summary
The Centers for Disease Control and Prevention (CDC) is working with federal, state, territorial, and local agencies and global health partners in response to recent hurricanes. CDC is aware of media reports and anecdotal accounts of various infectious diseases in hurricane-affected areas, including Puerto Rico and the US Virgin Islands (USVI). Because of compromised drinking water and decreased access to safe water, food, and shelter, the conditions for outbreaks of infectious diseases exist.
The purpose of this HAN advisory is to remind clinicians assessing patients currently in or recently returned from hurricane-affected areas to be vigilant in looking for certain infectious diseases, including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. Additionally, this Advisory provides guidance to state and territorial health departments on enhanced disease reporting.
Background
Hurricanes Irma and Maria made landfall in Puerto Rico and USVI in September 2017, causing widespread flooding and devastation. Natural hazards associated with the storms continue to affect many areas. Infectious disease outbreaks of diarrheal and respiratory illnesses can occur when access to safe water and sewage systems are disrupted and personal hygiene is difficult to maintain. Additionally, vector borne diseases can occur due to increased mosquito breeding in standing water; both Puerto Rico and USVI are at risk for outbreaks of dengue, Zika, and chikungunya.
Health care providers and public health practitioners should be aware that post-hurricane environmental conditions may pose an increased risk for the spread of infectious diseases among patients in or recently returned from hurricane-affected areas; including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. The period of heightened risk may last through March 2018, based on current predictions of full restoration of power and safe water systems in Puerto Rico and USVI.
In addition, providers in health care facilities that have experienced water damage or contaminated water systems should be aware of the potential for increased risk of infections in those facilities due to invasive fungi, nontuberculous Mycobacterium species, Legionella species, and other Gram-negative bacteria associated with water (e.g., Pseudomonas), especially among critically ill or immunocompromised patients.
Cholera has not occurred in Puerto Rico or USVI in many decades and is not expected to occur post-hurricane.
Recommendations
These recommendations apply to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas (e.g., within the past 4 weeks), during the period of September 2017 – March 2018.
- Health care providers and public health practitioners in hurricane-affected areas should look for community and healthcare-associated infectious diseases.
- Health care providers in the continental US are encouraged to ask patients about recent travel (e.g., within the past 4 weeks) to hurricane-affected areas.
- All healthcare providers should consider less common infectious disease etiologies in patients presenting with evidence of acute respiratory illness, gastroenteritis, renal or hepatic failure, wound infection, or other febrile illness. Some particularly important infectious diseases to consider include leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza.
- In the context of limited laboratory resources in hurricane-affected areas, health care providers should contact their territorial or state health department if they need assistance with ordering specific diagnostic tests.
- For certain conditions, such as leptospirosis, empiric therapy should be considered pending results of diagnostic tests— treatment for leptospirosis is most effective when initiated early in the disease process. Providers can contact their territorial or state health department or CDC for consultation.
- Local health care providers are strongly encouraged to report patients for whom there is a high level of suspicion for leptospirosis, dengue, hepatitis A, typhoid, and vibriosis to their local health authorities, while awaiting laboratory confirmation.
- Confirmed cases of leptospirosis, dengue, hepatitis A, typhoid fever, and vibriosis should be immediately reported to the territorial or state health department to facilitate public health investigation and, as appropriate, mitigate the risk of local transmission. While some of these conditions are not listed as reportable conditions in all states, they are conditions of public health importance and should be reported.
For More Information
- General health information about hurricanes and other tropical storms: https://www.cdc.gov/disasters/hurricanes/index.html
- Information about Hurricane Maria: https://www.cdc.gov/disasters/hurricanes/hurricane_maria.html
- Information for Travelers:
- Travel notice for Hurricanes Irma and Maria in the Caribbean: https://wwwnc.cdc.gov/travel/notices/alert/hurricane-irma-in-the-caribbean
- Health advice for travelers to Puerto Rico: https://wwwnc.cdc.gov/travel/destinations/traveler/none/puerto-rico?s_cid=ncezid-dgmq-travel-single-001
- Health advice for travelers to the U.S. Virgin Islands: https://wwwnc.cdc.gov/travel/destinations/traveler/none/usvirgin-islands?s_cid=ncezid-dgmq-travel-leftnav-traveler
- Resources from CDC Health Information for International Travel 2018 (the Yellow Book):
- Post-travel Evaluation: https://wwwnc.cdc.gov/travel/yellowbook/2018/post-travel-evaluation/general-approach-to-the-returned-traveler
- Information about infectious diseases after a disaster: https://www.cdc.gov/disasters/disease/infectious.html
- Dengue: https://www.cdc.gov/dengue/index.html
- Hepatitis A: https://www.cdc.gov/hepatitis/HAV/index.htm
- Leptospirosis: https://www.cdc.gov/leptospirosis/
- Typhoid fever: https://www.cdc.gov/typhoid-fever/index.html
- Vibriosis: https://www.cdc.gov/vibrio/index.html
- Information about other infectious diseases of concern:
- Conjunctivitis: https://www.cdc.gov/conjunctivitis/
- Influenza: https://www.cdc.gov/flu/index.htm
- Scabies: https://www.cdc.gov/parasites/scabies/index.html
- Tetanus and wound management: https://www.cdc.gov/disasters/emergwoundhcp.html
- Tetanus in Areas Affected by a Hurricane: Guidelines for Clinicians https://emergency.cdc.gov/coca/cocanow/2017/2017sept12.asp
Naegleria fowleri, the brain-eating amoeba, has claimed another life in Karachi: a young man of around 29 years of age;
Sunday, July 9th, 2017“…..Ruling out the possibility of swimming, he said the patient had spent four separate nights of Ramazan at a lawn for prayers. The doctor suspected that he might have contracted the infection during ablution before the prayers……They said that whenever the brain-eating amoeba found suitable environmental conditions and temperatures, it multiplied and infected the people who ingested the water through their nostrils. “Our research has shown that Naegleria fowleri colonies are present in the water tanks that were not cleaned for months and years,” said an AKUH expert and researcher.
“These microorganisms live in the layer of mud at the bottom of the water tanks, and when they find suitable environmental conditions, they start multiplying and targeting humans.”
The researcher said the best option to stay safe from N fowleri was to clean the overhead and underground tanks at houses, mosques and apartment buildings, and then to regularly chlorinate the water to kill the microorganisms.
“The water tanks at mosques should be cleaned on priority basis, as they are hardly cleaned and taken care of by the management of the mosques.” He said a large number of people made ablution on a daily basis at mosques and ingested the water through their nostrils, which could infect them with the amoeba……..”
Sindh health department has confirmed first Naegelria induced death of the year in Karachi
Wednesday, July 5th, 2017“…..Dr. Zafar Mehdi, however, claimed that needed measures were being adopted for naegleria prevention and control and that all possible sources in local context were being made for health safety of the public……”