Archive for September, 2016
Minnesota health officials have confirmed 3 new cases of Legionnaires’ disease linked to the ongoing Hopkins outbreak, bringing the total number to 20, including one death.
Friday, September 30th, 2016
Fast Facts
- Legionella can cause Legionnaires’ disease or Pontiac fever, collectively known as legionellosis.
- The bacterium was named after an outbreak in 1976, when many people who went to a Philadelphia convention of the American Legion got sick with pneumonia (lung infection).
- About 5,000 cases of Legionnaires’ disease are now reported each year in the United States. [1]
- About one out of every 10 people who get sick from Legionnaires’ disease will die. [2]
- People can get Legionnaires’ disease or Pontiac fever when they breathe in a mist (small droplets of water in the air) that has been contaminated with Legionella.
- In general, Legionnaires’ disease is not spread from one person to another. However, this may be possible in rare cases. [2]
- Legionella is found naturally in fresh water environments, like lakes and streams, but can become a health concern in human-made water systems.
- Keeping Legionella out of water systems in buildings is key to preventing infection.
Guatemala has become the 4th country in the Americas and the world to be declared free of onchocerciasis (river blindness)
Friday, September 30th, 2016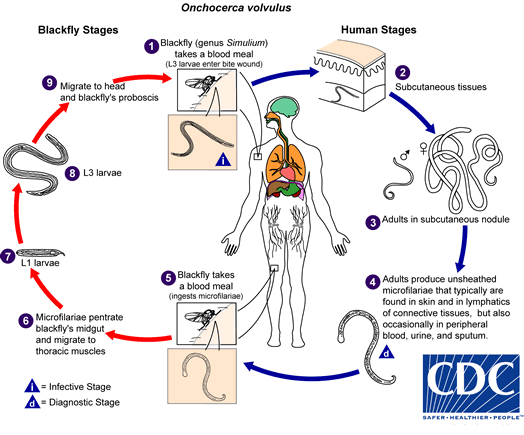
During a blood meal, an infected blackfly (genus Simulium) introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound  . In subcutaneous tissues the larvae
. In subcutaneous tissues the larvae  develop into adult filariae, which commonly reside in nodules in subcutaneous connective tissues
develop into adult filariae, which commonly reside in nodules in subcutaneous connective tissues  . Adults can live in the nodules for approximately 15 years. Some nodules may contain numerous male and female worms. Females measure 33 to 50 cm in length and 270 to 400 μm in diameter, while males measure 19 to 42 mm by 130 to 210 μm. In the subcutaneous nodules, the female worms are capable of producing microfilariae for approximately 9 years. The microfilariae, measuring 220 to 360 µm by 5 to 9 µm and unsheathed, have a life span that may reach 2 years. They are occasionally found in peripheral blood, urine, and sputum but are typically found in the skin and in the lymphatics of connective tissues
. Adults can live in the nodules for approximately 15 years. Some nodules may contain numerous male and female worms. Females measure 33 to 50 cm in length and 270 to 400 μm in diameter, while males measure 19 to 42 mm by 130 to 210 μm. In the subcutaneous nodules, the female worms are capable of producing microfilariae for approximately 9 years. The microfilariae, measuring 220 to 360 µm by 5 to 9 µm and unsheathed, have a life span that may reach 2 years. They are occasionally found in peripheral blood, urine, and sputum but are typically found in the skin and in the lymphatics of connective tissues  . A blackfly ingests the microfilariae during a blood meal
. A blackfly ingests the microfilariae during a blood meal  . After ingestion, the microfilariae migrate from the blackfly’s midgut through the hemocoel to the thoracic muscles
. After ingestion, the microfilariae migrate from the blackfly’s midgut through the hemocoel to the thoracic muscles  . There the microfilariae develop into first-stage larvae
. There the microfilariae develop into first-stage larvae  and subsequently into third-stage infective larvae
and subsequently into third-stage infective larvae  . The third-stage infective larvae migrate to the blackfly’s proboscis
. The third-stage infective larvae migrate to the blackfly’s proboscis  and can infect another human when the fly takes a blood meal
and can infect another human when the fly takes a blood meal  .
.

What is onchocerciasis?
Onchocerciasis is an infection caused by the parasitic worm Onchocerca volvulus, spread by the bite of an infected Simulium blackfly. It is also called River Blindness because the fly that transmits infection breeds in rapidly flowing streams and the infection can cause blindness. Persons with heavy infections will usually have one or more of three conditions: skin rash (usually itchy), eye disease, or nodules under the skin. The World Health Organization’s (WHO) expert committee on onchocerciasis estimates that at least 25 million people are infected and 123 million people live in areas that put them at risk of infection. About 300,000 people are blind because of the parasite and another 800,000 have visual impairment. Nearly 99% of infected persons live in Africa; the remainder lives in Yemen and six countries in the Americas. Onchocerciasis is commonly treated with an oral medicine called ivermectin.
In what parts of the world am I more likely to get onchocerciasis?
Onchocerciasis is locally transmitted in 30 countries of Africa and in Yemen in the Middle East. Local transmission occurred in 13 focal areas in 6 countries in the Americas (Mexico, Guatemala, Ecuador, Colombia, Venezuela, and Brazil), but transmission has now stopped in 11 of these focal areas. Transmission continues in one focal area in Venezuela and one in Brazil. Onchocerciasis in casual travelers is rare; the infection is transmitted in remote rural areas and, unlike malaria, contracting onchocerciasis often requires more than one infectious bite. Thus, risk of infection is greater in adventure travelers, missionaries, and Peace Corps and other long-term volunteers who are likely to have more intense or sustained exposure to blackfly bites. Given the low rate of transmission in the Americas, the likelihood is very low that any travelers in this region (even missionaries and long-term volunteers) would ever get infected.
How is onchocerciasis spread?
The disease spreads by the bite of an infectious blackfly. When a blackfly bites a person who has onchocerciasis, microscopic worm larvae (called microfilariae) in the infected person’s skin enter and infect the blackfly. The larvae develop over 2 weeks in the fly to a stage that is infectious to humans. An infectious blackfly will typically drop larvae when biting a person. The larvae then penetrate the skin to infect the person. Because the worms reproduce only in humans but need to complete some of their development inside the blackfly, the intensity of human infection (number of worms in an individual) is related to the number of infectious bites sustained by an individual. Blindness is usually seen in the setting of longstanding and intense infection.
Back To Top(http://www.cdc.gov/parasites/onchocerciasis/gen_info/faqs.html)
Who is most at risk for onchocerciasis?
Those most at risk are people who live in areas where the parasite is spread followed by adventure travelers, missionaries, and Peace Corps volunteers who are exposed for long periods of time (generally more than 3 months) to blackfly bites in areas where the parasite exists. The disease is most intensely transmitted in remote rural African agricultural villages which are located near rapidly flowing streams.
What is the impact of onchocerciasis?
Onchocerciasis is the second leading infectious cause of blindness and can cause debilitating and disfiguring skin disease. However, the worldwide burden of onchocerciasis has been considerably reduced as the result of very successful disease control programs led by the World Health Organization (WHO). These programs are based on control of the blackfly population and/or mass administration to affected communities of an oral drug called ivermectin (Mectizan™), that is donated by Merck & Co., Inc. As a result of these programs, millions of people are at greatly reduced risk of debilitating itching, disfigurement, and blindness caused by onchocerciasis. Unfortunately, many people still do not have access to prevention and treatment measures.
What are the clinical manifestations of onchocerciasis?
Infected persons may be without symptoms. Those with symptoms will usually have one or more of the three manifestations: skin rash (usually itchy), eye disease, and nodules under the skin. The most serious manifestation consists of lesions in the eye that can lead to visual impairment and blindness.
Back To Top(http://www.cdc.gov/parasites/onchocerciasis/gen_info/faqs.html)
How soon after infection will I have symptoms of onchocerciasis?
It can take up to one year for the larvae (also called microfilariae) to develop into an adult inside the human body and between 10 and 20 months before larvae can be found in the skin. Each adult female worm, which can live from 10–15 years, can produce millions of new larvae during her lifetime. As it is the larvae that cause most of the symptoms of onchocerciasis, most people feel well until after the adults start producing large numbers of new larvae.
What should I do if I think I may have onchocerciasis?
If you think you might have onchocerciasis, see your health care provider who may order skin biopsies (“snips”) or blood tests looking for antibodies to the parasite. However, examination of skin snips does not always show the parasites and positive blood tests do not necessarily indicate that you are still infected with O. volvulus.
What is the treatment for onchocerciasis?
There are treatments, such as ivermectin, available to kill the larvae in your body and thus prevent the symptoms of the disease, such as skin rash and blindness. Promising treatments, such as doxycycline, to kill the adult worms are currently being studied. You should discuss your treatment options with your health care provider.
Back To Top(http://www.cdc.gov/parasites/onchocerciasis/gen_info/faqs.html)
How can I prevent onchocerciasis?
Blackflies bite during the day. The best prevention is avoiding being bitten by infected blackflies by using insecticides that contain N,N-Diethyl-meta-toluamide (DEET) on exposed skin, wearing long sleeve shirts and pants, and wearing permethrin treated clothing.
Can I take medication to prevent onchocerciasis?
No, there is neither a vaccine nor recommended drug available to prevent onchocerciasis.
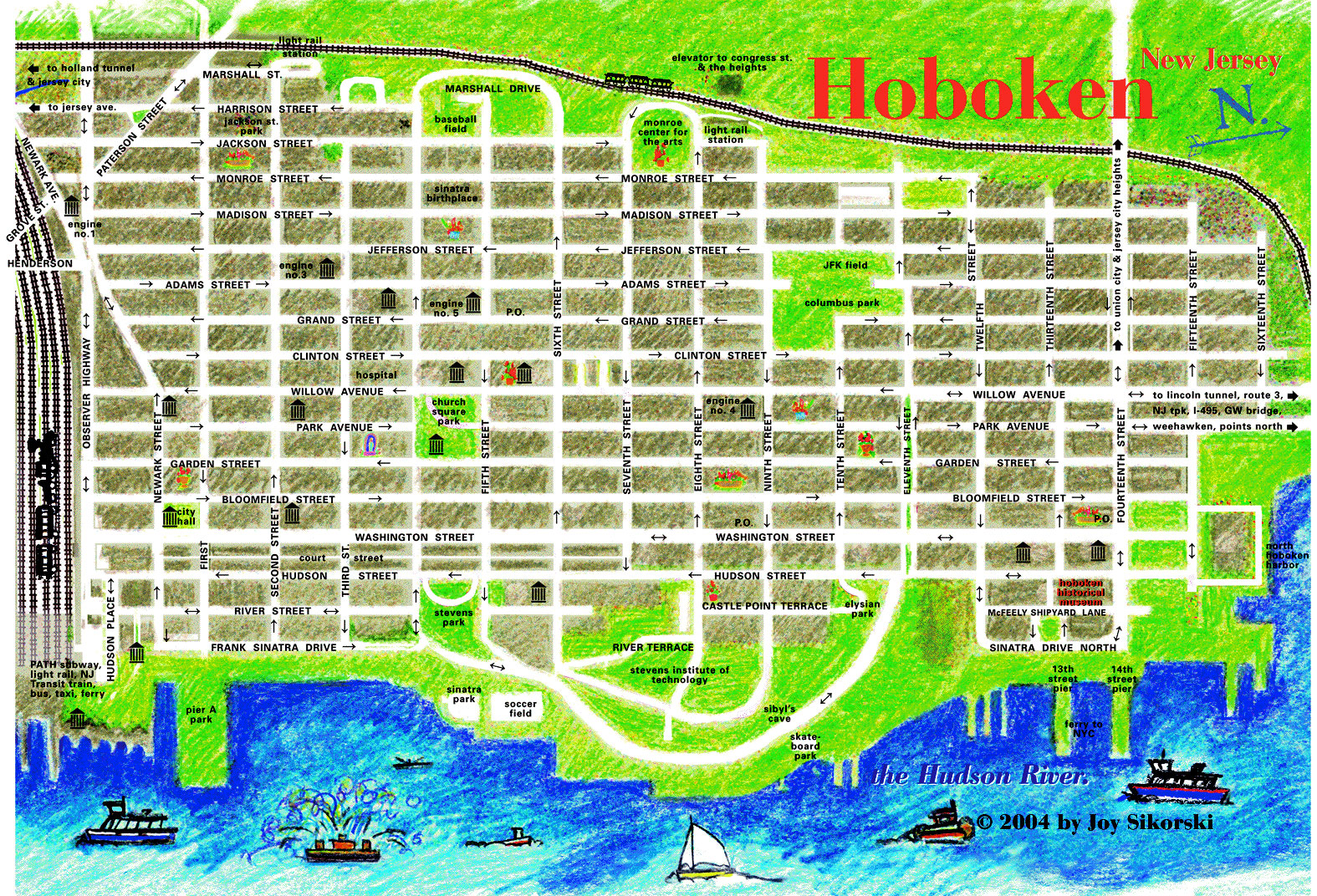
A New Jersey Transit train crashed into the Hoboken station Thursday morning causing massive damage and dozens of injuries
Thursday, September 29th, 2016Sudan: Credible evidence of the use of chemical weapons to kill and maim hundreds of civilians including children in Darfur revealed.
Thursday, September 29th, 2016“….Using satellite imagery, more than 200 in-depth interviews with survivors and expert analysis of dozens of appalling images showing babies and young children with terrible injuries, the investigation indicates that at least 30 likely chemical attacks have taken place in the Jebel Marra area of Darfur since January 2016. The most recent was on 9 September 2016. The scale and brutality of these attacks is hard to put into words. The images and videos we have seen in the course of our research are truly shocking; in one a young child is screaming with pain before dying; many photos show young children covered in lesions and blisters. Some were unable to breath and vomiting blood,” said Tirana Hassan, Amnesty International’s Director of Crisis Research…..”
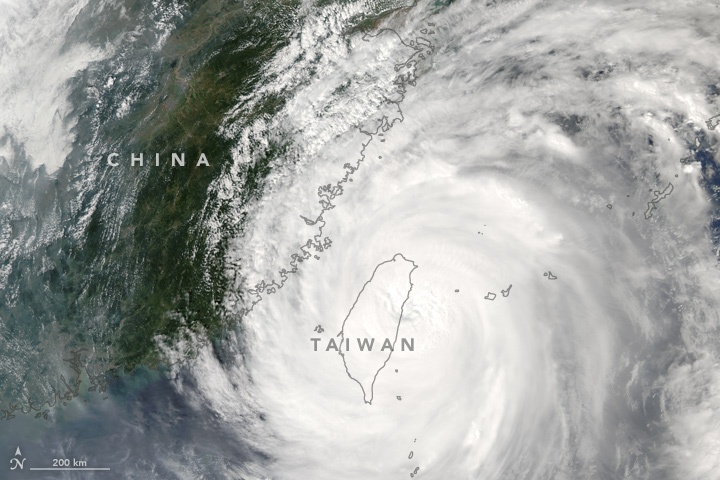
In the aftermath of Megi: Chinese rescuers pull 15 alive from landslide, but 32 still missing
Thursday, September 29th, 2016Typhoon Megi: At least 32 people are missing in China’s Zhejiang province after heavy rains triggered 2 landslides.
Thursday, September 29th, 2016September 28 is World Rabies Day.
Wednesday, September 28th, 2016Take a Bite Out of Rabies!
In the United States and most of the American continent, dying of rabies is rare thanks to successful animal control and vaccination programs. But around the world, rabies kills more than 59,000 people every year—that is nearly one death every nine minutes. Most affected are countries in Africa and Asia, and almost half of the victims are children under the age of 15.
The good news is that rabies can be prevented through vaccination, both in our animals and in people. On World Rabies Day, as we celebrate our progress, we must also renew our commitment to eliminate human rabies deaths.
Get the facts on rabies prevention and control, and become an advocate for rabies elimination. Find events in your area to participate in World Rabies Day activities.

The U.S. has been successful in eliminating canine rabies. Take steps to prevent rabies in your pets!

Children in Haiti bring their puppies to the rabies vaccination clinic. Learn more about what CDC is doing to control rabies in Haiti(http://www.cdc.gov/worldrabiesday/), which has the highest rates of rabies infection in the Americas.

Be sure to take your cats and dogs to the veterinarian each year.

Raccoons, bats, skunks and foxes often get rabies and should be avoided.

In U.S., bats often spread rabies to other animals, but also to people.
The Challenge of Rabies
The group of viruses that cause rabies are present on every continent except Antarctica. Rabies viruses are deadly and can kill anyone who gets them. Every year, an estimated 40,000 people in the U.S. receive a series of shots known as post-exposure prophylaxis (PEP) after contact with a possibly rabid animal. The U.S. public health cost associated with rabies is estimated to be as high as $500 million annually.
People usually get rabies when they are bitten by an animal that has the virus. In the U.S., the animals that most often get rabies are wild animals such as raccoons, skunks, bats, and foxes. A particular kind of rabies virus, called canine rabies that spreads from dog to dog, is the cause of 98% of human deaths worldwide. While the U.S. successfully eliminated the canine rabies virus, we still need to keep our dogs and cats vaccinated to prevent this kind of virus from coming back, and to protect our pets from rabies viruses they could get from wildlife.
However, canine rabies is not controlled in many regions of the world and continues to threaten the health of people and animals in these areas. Scientists estimate there are about 500 million dogs in the world. In many countries, most dogs are unvaccinated and allowed to roam freely. When these dogs get rabies, they often pass the virus to their owners, family members, and neighbors. Vaccination of dogs is the best way to prevent human deaths.
CDC disease detectives and scientists work around the world to help start programs for better control of rabies. The most effective way to prevent the disease in people is to vaccinate the dogs. Scientists have shown that once 70% of dogs are vaccinated, rabies can be successfully controlled in that area and human deaths can be prevented. People everywhere will directly benefit from these efforts.
What You Can Do to Protect Yourself and Others from Rabies
Whether you are a pet owner, a parent, an outdoor adventurer or a backyard explorer, there are steps you can take to keep yourself and your family free from rabies throughout the year.
1. Take Pets to a Veterinarian for Their Rabies Shot
Pets, like dogs, cats, and ferrets, need to see a veterinarian regularly. A veterinarian can make sure your pets are up to date on their rabies shot, which can protect them from getting rabies. All dogs and cats should be vaccinated around four months of age, and then again one year later. After these two shots, your veterinarian will develop a vaccination plan that is best for your pet and complies with local laws. This is important, since animals that have not received a rabies shot and are in contact with potentially rabid wild animals may need to be quarantined for six months or euthanized.
Talk to your veterinarian about spaying or neutering your pet. This helps cut down on the number of unwanted and stray animals, which often do not have their rabies shot and are in close contact with wild animals.
2. Keep Away From Wildlife and Unfamiliar Animals
In the United States, more than 90% of all animal rabies cases reported to CDC each year occur in wild animals. The main animals that get rabies are raccoons, bats, skunks and foxes.
One of the best ways to protect yourself and your family is to avoid contact with wild animals. Do not feed or handle them, even if they seem friendly.
You should also avoid dogs and cats that are unfamiliar to you and your family. These animals may be in contact with wildlife and can also spread rabies to humans.
If you see an animal acting strangely, report it to animal control or your local health department. Some things to look for are:
- General sickness
- Problems swallowing
- Lots of drool or saliva
- An animal that appears more tame than you would expect
- An animal that bites at everything
- An animal that’s having trouble moving or may even be paralyzed
Sometimes, people may come across a dead animal. Never pick up or touch dead animals. The rabies virus may still be present in the saliva or nervous tissue, especially if they have only been dead for a short time. If you see a dead animal, call animal control to take care of the animal’s body.
3. Keep Your Pets Indoors or Supervised
No matter where you live, rabies can threaten your family’s health. Fortunately, there are things you can do around the home to help reduce the risk of getting rabies.
- Keep your pets indoors. When you let your dog or cat go outside, it’s best to have a fenced-in yard and make sure someone is there to watch it and keep it safe. Use a leash when walking your dog.
- Do not feed or put water for your pets outside and keep garbage securely covered. These items may attract wild animals or stray animals to your yard.
- Teach children never to handle wild animals or unfamiliar domestic animals.
While most wild animals are found primarily outdoors, bats can sometimes fly into buildings. This includes your home and even the room where you sleep. Every year indoor-only cats develop rabies because of bats in the home. It is important to keep all cats up to date on rabies vaccination, even if they never leave your home. Learn what to do when you find a bat in your home(http://www.cdc.gov/rabies/bats/contact/capture.html). There are also steps you can take to “bat-proof” your home(http://www.cdc.gov/rabies/bats/index.html)