“WHO commends the Government of Guinea and its people on the significant achievement of ending its Ebola outbreak. We must render homage to the Government and people of Guinea who, in adversity, have shown extraordinary leadership in fighting the epidemic,” says Dr Mohamed Belhocine, WHO Representative in Guinea. “WHO and its partners will continue to support Guinea during the next 90 days of heightened surveillance and in its early efforts to restart and strengthen essential health services throughout 2016.”
A milestone for the Ebola outbreak
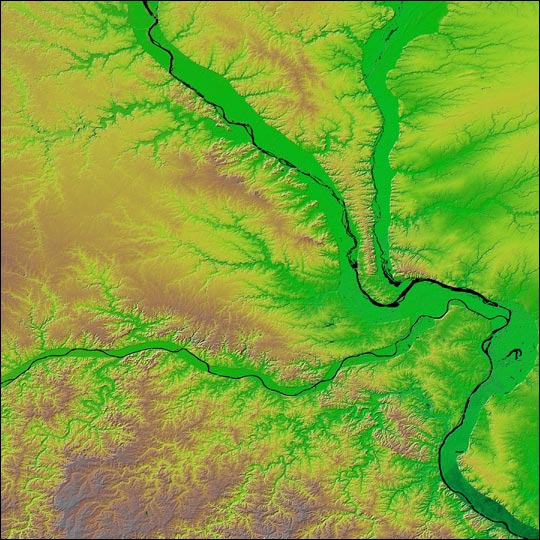
The end of Ebola transmission in Guinea marks an important milestone in the Ebola outbreak in West Africa. The original chain of transmission started two years ago in Gueckedou, Guinea in late December 2013 and drove the outbreak which spread to neighbouring Liberia and Sierra Leone and, ultimately, by land and air travel to seven other countries.
“This is the first time that all three countries – Guinea, Liberia and Sierra Leone – have stopped the original chains of transmission that were responsible for starting this devastating outbreak two years ago,” says Dr Matshidiso Moeti, WHO Regional Director for Africa. “I commend the governments, communities and partners for their determination in confronting this epidemic to get to this milestone. As we work towards building resilient health care systems, we need to stay vigilant to ensure that we rapidly stop any new flares that may come up in 2016.”
In addition to the original chain of transmission, there have been 10 new small Ebola outbreaks (or ‘flares’) between March and November 2015. These appear to have been due to the re-emergence of a persistent virus from the survivor population.
Among the challenges survivors have faced is that after recovering from Ebola virus disease and clearing the virus from their bloodstream, the virus may persist in the semen of some male survivors for as long as 9-12 months.
WHO and its partners are working with the Governments of Liberia, Sierra Leone and Guinea to help ensure that survivors have access to medical and psychosocial care, screening for persistent virus, as well as counselling and education to help them reintegrate into family and community life, reduce stigma and minimize the risk of Ebola virus transmission.
Sustained support to Guinea, Liberia and Sierra Leone
“The coming months will be absolutely critical,” says Dr Bruce Aylward, Special Representative of the Director-General for the Ebola Response, WHO. “This is the period when the countries need to be sure that they are fully prepared to prevent, detect and respond to any new cases.
“The time-limited persistence of virus in survivors which may give rise to new Ebola flares in 2016 makes it imperative that partners continue to support these countries. WHO will maintain surveillance and outbreak response teams in the three countries through 2016.”
At the same time, 2016 will see the three most-affected countries implementing a full health sector recovery agenda to restart and strengthen key public health programmes, especially maternal and child health, while continuing to maintain the capacity to detect, prevent and respond to any flare-up of Ebola.