Archive for June, 2019
CDC: 62 people in 8 US states have fallen ill this year from Salmonella related to fresh papayas imported from Mexico
Sunday, June 30th, 2019“……The illnesses range from mid-January up to June 8, with the highest number occurring in April. Of those who’ve gotten sick, 23 have been hospitalized.
So far, no deaths are reported…..”
Sahel: Humanitarian Emergency
Saturday, June 29th, 2019“…..UN aid agencies and NGOs warned today that surging armed violence in the Sahel has propelled forced displacement and humanitarian emergency to unprecedented levels. They called for stepped-up support and greater efforts to address the causes of the region’s crises.
In the past year, around 1 million people had to flee their homes due to insecurity and violence. In Burkina Faso, Mali and western Niger displacement has increased five-fold, and the Lake Chad Basin is witnessing a new spike in displacement and attacks. Across the Sahel, 4.2 million people are uprooted…..”
HUMANITARIAN EMERGENCY AT UNPRECEDENTED LEVEL IN SAHEL
Dakar, 27 June 2019 – UN aid agencies and NGOs warned today that surging armed violence in the Sahel has propelled forced displacement and humanitarian emergency to unprecedented levels. They called for stepped-up support and greater efforts to address the causes of the region’s crises. In the past year, around 1 million people had to flee their homes due to insecurity and violence. In Burkina Faso, Mali and western Niger displacement has increased five-fold, and the Lake Chad Basin is witnessing a new spike in displacement and attacks. Across the Sahel, 4.2 million people are uprooted.
“The impact of the crisis, in one of the world’s most vulnerable regions, is dramatic. The extent and intensity of the attacks have left communities suffering untold devastation,” said Chris Nikoi, Regional Director of the World Food Programme. “Millions of people have yet to recover from last year’s food and nutrition crisis. With the lean season underway, we must provide quick and sustained help to save lives and avert a deeper crisis.”
The violence is disrupting livelihoods and deepening the impact of chronic vulnerabilities such as food insecurity, malnutrition and epidemics in affected communities in Burkina Faso, Cameroon (Far North), Chad, Mali, Niger and north-east Nigeria. More than 7 million people are struggling with food insecurity. Malnutrition is threatening the lives of 5 million children. Education has been significantly hit, with more than 4,000 schools closed or not functional and 900,000 pupils affected.
“With armed violence comes destitution and deprivation. We must safeguard the dignity of people affected by conflict and ensure their protection from threats, exploitation and abuse,” said Liz Ahua, the UN Refugee Agency (UNHCR) Regional Representative for West Africa. “Beyond the humanitarian response, the Sahel needs support to tackle the root causes of the recurrent crises besetting the region. Crucially, the Sahel needs more robust investment in public services, infrastructure and economic development to bring about lasting solutions for all its people.”
Although conflict and its devastating impact have plagued the Sahel for many years, insecurity has never spread so fast, in such vast areas and affected as many people. The risk of spill-over beyond the Sahel and into coastal countries is growing.
“Humanitarian access continues to be under threat. Insecurity and restrictions imposed during military operations hinder the delivery of aid. Faced with these difficulties, we must insist on humanitarian principles. We are there to stay and assist the affected communities wherever they are,” said Marianne Irion, Regional Director of the Norwegian Refugee Council.
“If we want to reverse the trend in the Sahel, the security-centric focus must change,” said Mamadou Diop, Regional Director of Action Contre la Faim. “We must ensure people’s access to basic services, especially in the conflict-affected areas, where needs are outpacing available resources. And we need flexible funding to build resilience and address the root causes of the crises.”
The humanitarian community has requested for US$ 2.4 billion to assist 15.3
Causes of severe pneumonia requiring hospital admission in children around the world
Saturday, June 29th, 2019“…….Between Aug 15, 2011, and Jan 30, 2014, we enrolled 4232 cases and 5119 community controls. The primary analysis group was comprised of 1769 (41·8% of 4232) cases without HIV infection and with positive chest x-rays and 5102 (99·7% of 5119) community controls without HIV infection.
Wheezing was present in 555 (31·7%) of 1752 cases (range by site 10·6–97·3%).
30-day case-fatality ratio was 6·4% (114 of 1769 cases).
Blood cultures were positive in 56 (3·2%) of 1749 cases, and Streptococcus pneumoniae was the most common bacteria isolated (19 [33·9%] of 56). Almost all cases (98·9%) and controls (98·0%) had at least one pathogen detected by PCR in the NP-OP specimen. The detection of respiratory syncytial virus (RSV), parainfluenza virus, human metapneumovirus, influenza virus, S pneumoniae, Haemophilus influenzae type b (Hib), H influenzae non-type b, and Pneumocystis jirovecii in NP-OP specimens was associated with case status.
The aetiology analysis estimated that viruses accounted for 61·4% (95% credible interval [CrI] 57·3–65·6) of causes, whereas bacteria accounted for 27·3% (23·3–31·6) and Mycobacterium tuberculosis for 5·9% (3·9–8·3).
Viruses were less common (54·5%, 95% CrI 47·4–61·5 vs 68·0%, 62·7–72·7) and bacteria more common (33·7%, 27·2–40·8 vs 22·8%, 18·3–27·6) in very severe pneumonia cases than in severe cases.
 RSV had the greatest aetiological fraction (31·1%, 95% CrI 28·4–34·2) of all pathogens. Human rhinovirus, human metapneumovirus A or B, human parainfluenza virus, S pneumoniae, M tuberculosis, and H influenzae each accounted for 5% or more of the aetiological distribution. We observed differences in aetiological fraction by age for Bordetella pertussis, parainfluenza types 1 and 3, parechovirus–enterovirus, P jirovecii, RSV, rhinovirus, Staphylococcus aureus, and S pneumoniae, and differences by severity for RSV, S aureus, S pneumoniae, and parainfluenza type 3. The leading ten pathogens of each site accounted for 79% or more of the site’s aetiological fraction…..”
RSV had the greatest aetiological fraction (31·1%, 95% CrI 28·4–34·2) of all pathogens. Human rhinovirus, human metapneumovirus A or B, human parainfluenza virus, S pneumoniae, M tuberculosis, and H influenzae each accounted for 5% or more of the aetiological distribution. We observed differences in aetiological fraction by age for Bordetella pertussis, parainfluenza types 1 and 3, parechovirus–enterovirus, P jirovecii, RSV, rhinovirus, Staphylococcus aureus, and S pneumoniae, and differences by severity for RSV, S aureus, S pneumoniae, and parainfluenza type 3. The leading ten pathogens of each site accounted for 79% or more of the site’s aetiological fraction…..”
Health concerns for this summer’s travelers.
Saturday, June 29th, 2019-
Worldwide: Measles
-
Japan: Rubella
-
Brazil: Yellow Fever
-
Indonesia: Polio
-
Israel: Leptospirosis
- Europe And India: Heat
Eliminating trachoma
Friday, June 28th, 2019Eliminating trachoma: WHO announces sustained progress with hundreds of millions of people no longer at risk of infection
27 June 2019 | Maputo | Geneva — The number of people at risk of trachoma – the world’s leading infectious cause of blindness – has fallen from 1.5 billion in 2002 to just over 142 million in 2019, a reduction of 91%, the World Health Organization (WHO) has reported.

ew data presented today at the 22nd meeting of the WHO Alliance for the Global Elimination of Trachoma by 2020 (GET2020) also show that the number of people requiring surgery for trachomatous trichiasis – the late, blinding stage of trachoma – has dropped from 7.6 million in 2002 to 2.5 million in 2019, a reduction of 68%.
“Eliminating trachoma contributes to the ocular health and quality of life of the poorest, most disadvantaged people worldwide and thereby moves us a step closer to achieving universal health coverage,” said Dr Mwelecele Ntuli Malecela, Director, WHO Department of Control of Neglected Tropical Diseases. “Ridding the world of this painful, debilitating disease is being made possible through generous donations of the antibiotic azithromycin, sustained contributions from a network of dedicated funding agencies and partners, and the efforts of hundreds of thousands of front-line workers who work tirelessly to engage communities and deliver interventions.”
Trachoma remains endemic in 44 countries and has blinded or visually impaired around 1.9 million people worldwide. Mapping of trachoma has been completed to identify its distribution and target control measures through the SAFE strategy, namely: surgery for trichiasis, antibiotics to clear infection, and facial cleanliness and environmental improvement to reduce transmission. The disease is caused by infection with a bacterium.
“Eliminating trachoma has immediate benefit in preserving vision for people at risk. But work against trachoma has required the creation of innovative partnerships, which will help ensure that the most remote and marginalized people are not left behind as more comprehensive health services are strengthened,” said Mr Scott McPherson, Chair, International Coalition for Trachoma Control.
In 2018 alone, 146112 cases of trichiasis were managed and almost 90 million people were treated with antibiotics for trachoma in 782 districts worldwide.
Since 2011, eight countries have been validated by WHO as having eliminated trachoma as a public health problem.1 At least one country in every trachoma-endemic WHO Region has now achieved this milestone, demonstrating the effectiveness of the SAFE strategy in different settings.
“This is great progress, but we cannot afford to become complacent,” said Dr Anthony Solomon, Medical Officer in charge of WHO’s global trachoma elimination programme. “We should be able to relegate trachoma to the history books in the next few years, but we will only do so by redoubling our efforts now. The last few countries are likely to be the hardest”.
The significant reduction in the global prevalence of trachoma has resulted from increased political will in endemic countries, expansion of control measures and generation of high-quality data. The global programme has been supported by the world’s largest infectious disease mapping effort – the Global Trachoma Mapping Project (2012–2016) – and, since 2016, by Tropical Data, which has assisted health ministries to complete more than 1500 internationally-standardized, quality-assured and quality-controlled prevalence surveys.
GET2020
In 1996, WHO launched GET2020, and with other partners in the Alliance, supports country implementation of the SAFE strategy and strengthening of national capacity for epidemiological assessment, monitoring, surveillance, project evaluation and resource mobilization.
Elimination of trachoma is inexpensive, simple and highly cost–effective, yielding a high rate of net economic return.
Note to editors
Trachoma is a disease of the eye caused by infection with the bacterium Chlamydia trachomatis. Transmission occurs through contact with infective discharges from the
eyes and nose, particularly in young children who harbour the main reservoir of infection. It is also spread by flies which have been in contact with the eyes and noses of infected people.
The immune system can clear a single episode of infection, but in endemic communities the organism is frequently reacquired. After years of repeated infection, the inside of the eyelid can become so severely scarred (trachomatous conjunctival scarring) that it turns inwards and causes the eyelashes to rub against the eyeball (trachomatous trichiasis), resulting in constant pain and light intolerance. This and other alterations of the eye can lead to scarring of the cornea. Left untreated, this condition leads to the formation of irreversible opacities, with resulting visual impairment or blindness.
——————————-
1Cambodia, Ghana, Islamic Republic of Iran, Lao People’s Democratic Republic, Mexico, Morocco, Nepal and Oman.
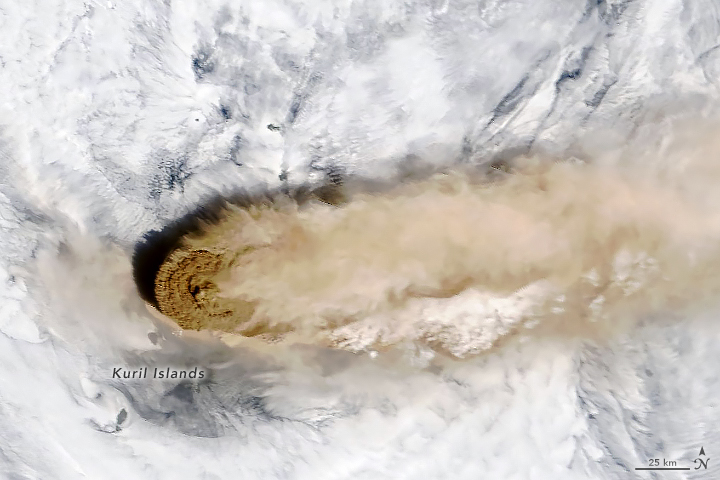
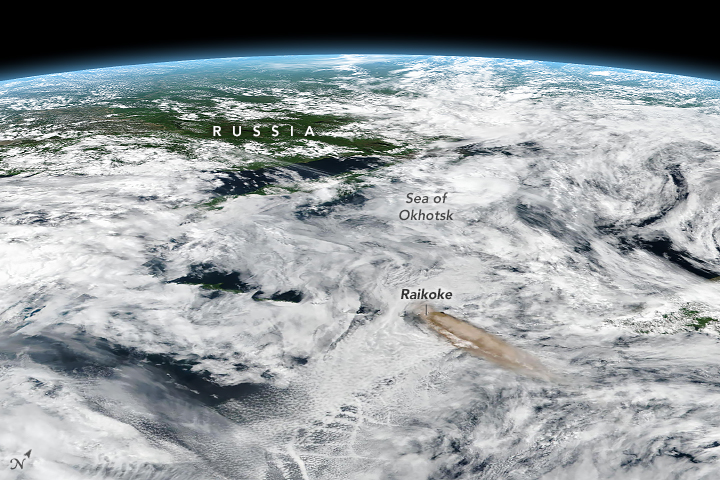
Raikoke Volcano on the Kuril Islands rarely erupts. The small, oval-shaped island most recently exploded in 1924 and in 1778. The dormant period ended around 4:00 a.m. local time on June 22, 2019
Thursday, June 27th, 2019A thick plume of volcanic ash rises above the dense cloud cover in this close-up #Himawari8 view of the #Raikoke volcano's eruption. This was the volcano's first eruption since 1924. More imagery: https://t.co/wIF4txQIDW pic.twitter.com/vZExba5QDZ
— NOAA Satellites (@NOAASatellites) June 24, 2019
Unlike some of its perpetually active neighbors on the Kamchatka Peninsula, Raikoke Volcano on the Kuril Islands rarely erupts. The small, oval-shaped island most recently exploded in 1924 and in 1778.
The dormant period ended around 4:00 a.m. local time on June 22, 2019, when a vast plume of ash and volcanic gases shot up from its 700-meter-wide crater. Several satellites—as well as astronauts on the International Space Station—observed as a thick plume rose and then streamed east as it was pulled into the circulation of a storm in the North Pacific.
On the morning of June 22, astronauts shot a photograph (above) of the volcanic plume rising in a narrow column and then spreading out in a part of the plume known as the umbrella region. That is the area where the density of the plume and the surrounding air equalize and the plume stops rising. The ring of clouds at the base of the column appears to be water vapor.
“What a spectacular image. It reminds me of the classic Sarychev Peak astronaut photograph of an eruption in the Kuriles from about ten years ago,” said Simon Carn, a volcanologist at Michigan Tech. “The ring of white puffy clouds at the base of the column might be a sign of ambient air being drawn into the column and the condensation of water vapor. Or it could be a rising plume from interaction between magma and seawater because Raikoke is a small island and flows likely entered the water.”
The Moderate Resolution Imaging Spectroradiometer (MODIS) on NASA’s Terra satellite acquired the second image on the morning of June 22. At the time, the most concentrated ash was on the western edge of the plume, above Raikoke. The third image, an oblique, composite view based on data from the Visible Infrared Imaging Radiometer Suite (VIIRS) on Suomi NPP, shows the plume a few hours later. After an initial surge of activity that included several distinct explosive pulses, activity subsided and strong winds spread the ash across the Pacific. By the next day, just a faint remnant of the ash remained visible to MODIS.
Since ash contains sharp fragments of rock and volcanic glass, it poses a serious hazard to aircraft. The Tokyo and Anchorage Volcanic Ash Advisory Centers have been tracking the plume closely and have issued several notes to aviators indicating that ash had reached an altitude of 13 kilometers (8 miles). Meanwhile, data from the CALIPSO satellite indicate that parts of the plume may have reached 17 kilometers (10 miles).
In addition to tracking ash, satellite sensors can also track the movements of volcanic gases. In this case, Raikoke produced a concentrated plume of sulfur dioxide (SO2) that separated from the ash and swirled throughout the North Pacific as the plume interacted with the storm.
“Radiosonde data from the region indicate a tropopause altitude of about 11 kilometers, so altitudes of 13 to 17 kilometers suggest that the eruption cloud is mostly in the stratosphere,” said Carn. “The persistence of large SO2 amounts over the last two days also indicates stratospheric injection.”
Volcanologists watch closely for plumes that reach the stratosphere because they tend to stay aloft for longer than those that remain within the troposphere. That is why plumes that reaches the stratosphere typically have the greatest effects on aviation and climate.
NASA Earth Observatory images by Joshua Stevens, using MODIS and VIIRS data from NASA EOSDIS/LANCE and GIBS/Worldview and the Suomi National Polar-orbiting Partnership. Astronaut photograph ISS059-E-119250 was acquired on June 22, 2019, with a Nikon D5 digital camera and is provided by the ISS Crew Earth Observations Facility and the Earth Science and Remote Sensing Unit, Johnson Space Center. The image was taken by a member of the Expedition 59 crew. The image has been cropped and enhanced to improve contrast, and lens artifacts have been removed. Story by Adam Voiland, with information from Erik Klemetti (Denison University), Simon Carn (Michigan Tech), and Andrew Prata (Barcelona Supercomputing Center).
DRC: Ebola outbreak total up to 2,277
Thursday, June 27th, 2019Kampala, 26 June 2019 – After assessing one of the high-risk districts for Ebola virus disease in western Uganda today, Dr Matshidiso Moeti, World Health Organization (WHO) Regional Director for Africa, commended the corps of health workers and Health Ministry officials for their sharpened preparedness to respond to an outbreak.
Dr Moeti toured the Kasese border area with the Minister of Health of Uganda, Dr Jane Ruth Aceng, who thanked WHO for the support the organization has provided both in preparing the country for Ebola and in responding to the recent confirmed cases.
“WHO has provided crucial support to Uganda in fighting Ebola,” said Dr Aceng. “I am glad to see how my teams on the ground have responded quickly and effectively.”
Prime Minister, Right Honourable Ruhakana Rugunda also expressed his commitment to the Ebola response during a meeting with Dr Moeti and senior governmental officials in Kampala.
Since 11 June, when Uganda declared the Ebola virus disease outbreak, there have been three confirmed cases, all of whom had travelled to the neighbouring Democratic Republic of the Congo (DRC). Uganda shares a nearly 900-kilometre long, often porous border with the DRC, where the disease has claimed more than 1 400 lives since August 2018.
More than 100 people who had contacts with the confirmed cases are being monitored. Since the outbreak was declared, 1063 high risk individuals have been vaccinated. This vaccination of contacts and contacts of contacts, known as ring vaccination, has showed good results in the DRC and other countries in West Africa. There are currently no new, confirmed cases of Ebola in Uganda.
“I commend Uganda for its quick response to the Ebola outbreak,” Dr Moeti said. “During my visit to the Kasese area, I spoke with health authorities who told me how the training they had received in detecting the disease meant they were on high alert for patients with any signs of infection. They were able to move swiftly when the first Ebola cases arrived in their health facility and to restrict possible exposure to relatively few health workers.”
During her two-day visit, Dr Moeti travelled to Bwera Hospital, near the border with the DRC where two of the three people who had the infection had died. A further three suspected cases are being treated at the hospital. Due to its investment into preparedness, the hospital can now obtain presumptive results to tests for the Ebola Zaire strain within two hours.
With support from WHO and partners, Uganda has trained more than 16 000 community leaders and volunteers in remote border areas to spot the symptoms, provide medical attention to potential patients and to alert the authorities. The local teams serve as the eyes and ears of the district and national emergency systems that cover surveillance, infection prevention and control, patient care, cross-border activities and coordination with communities.
“People are aware of the problem, how to protect themselves and where to report for action and support,” Dr Moeti pointed out.
Cross-border surveillance and collaboration between Uganda and DRC health authorities facilitated the early detection and response in Kasese where the cases were confirmed. Rapid reporting by DRC counterparts led to the easy tracing of the cases by Ugandan health authorities.
Since the first outbreak in the DRC in 2018, Uganda has trained more than 9 000 of its health workers to spot the signs of Ebola and vaccinated nearly 5 000 of them against the disease.
“The cost of preparedness is cheaper than response,” Dr Moeti added at the conclusion of her visit, adding donors and partners in her praise of the extensive preparedness activities. “It is the contribution of donors that has enabled us to help countries prepare and, as we have seen in Uganda, prevent the tragedy of an outbreak escalating to unimaginable numbers.”
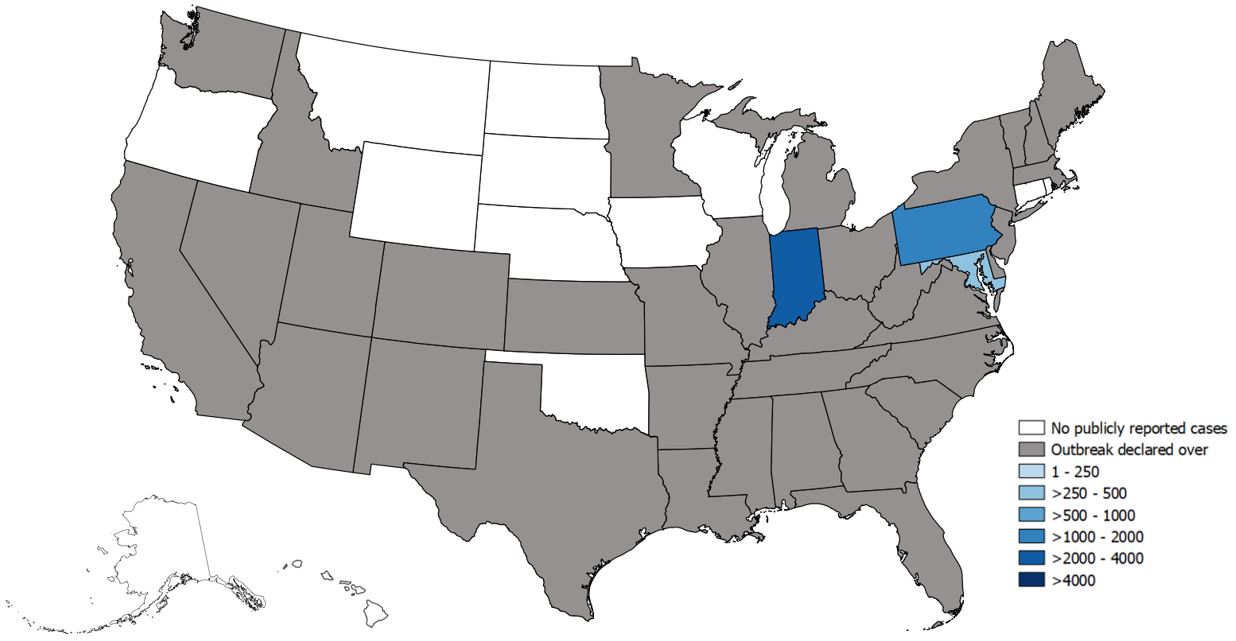
Widespread outbreaks of hepatitis A across the United States
Thursday, June 27th, 2019Since March 2017, CDC’s Division of Viral Hepatitis (DVH) has been assisting multiple state and local health departments with hepatitis A outbreaks, spread through person-to-person contact.
The hepatitis A vaccine is the best way to prevent HAV infection
- The following groups are at highest risk for acquiring HAV infection or developing serious complications from HAV infection in these outbreaks and should be offered the hepatitis A vaccine in order to prevent or control an outbreak:
- People who use drugs (injection or non-injection)
- People experiencing unstable housing or homelessness
- Men who have sex with men (MSM)
- People who are currently or were recently incarcerated
- People with chronic liver disease, including cirrhosis, hepatitis B, or hepatitis C
- One dose of single-antigen hepatitis A vaccine has been shown to control outbreaks of hepatitis A and provides up to 95% seroprotection in healthy individuals for up to 11 years.1,2
- Pre-vaccination serologic testing is not required to administer hepatitis A vaccine. Vaccinations should not be postponed if vaccination history cannot be obtained or records are unavailable.
CDC has provided outbreak-specific considerations for hepatitis A vaccine administration.
State-Reported Hepatitis A Outbreak Cases as of June 21, 2019