Archive for February, 2016
Hawaii reports 244 dengue cases
Wednesday, February 3rd, 2016Aedes aegypti and Aedes albopictus mosquitoes can transmit the viruses that cause dengue fever.
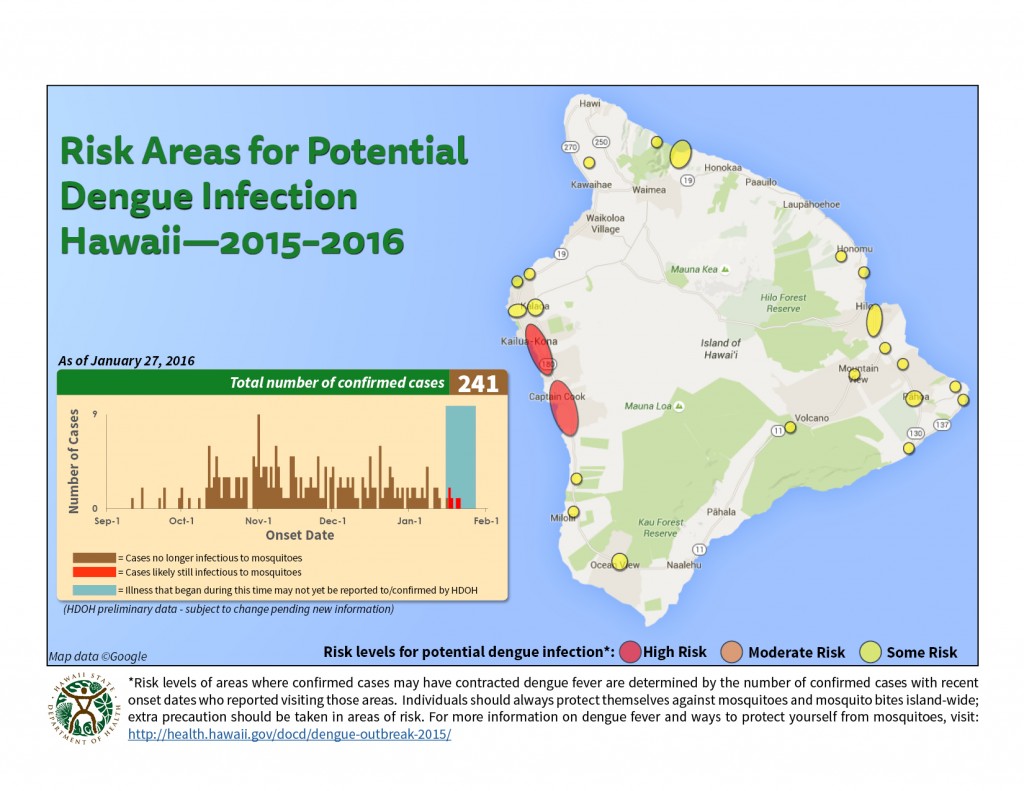
The Hawaii Department of Health (HDOH) is investigating a cluster of locally-acquired cases of dengue fever on Hawaii Island (the Big Island). Dengue is not endemic to Hawaii. However, it is intermittently imported from endemic areas by infected travelers. This is the first cluster of locally-acquired dengue fever since the 2011 outbreak on Oahu. The Big Island and the rest of Hawaii remain safe destinations for visitors and residents.
As of February 2, 2016*:
Since the last update, HDOH has identified 2 new cases of dengue fever. Currently, as many as 3 of the confirmed cases to date are potentially infectious to mosquitoes. All others are no longer infectious.
| Potentially infectious individuals |
3 | Illness onset 1/23/16 to 1/26/16 |
| Cases no longer infectious |
243 | Illness onset 9/11/15 to 1/21/16 |
| Past and present confirmed cases (Cumulative TOTAL) |
246 | |
Of the confirmed cases, 222 are Hawaii Island residents and 24 are visitors.
201 cases have been adults; 45 have been children (<18 years of age). Onset of illness has ranged between 9/11/15 – 1/25/16.
As of today, a total of 1071 reported potential cases have been excluded based on test results and/or not meeting case criteria.
For Hawaii Island Dengue Fever Unified Command Updates, click HERE. (Updated January 20, 2016)
HDOH continues to routinely monitor for cases of imported dengue infection on ALL islands and will continue to have Vector Control perform mosquito site assessments and abatement as needed. Since the beginning of our current investigation on Hawaii island, thirteen imported dengue fever cases have been confirmed (seven on Oahu, three on Maui, two on Hawaii, 1 visitor), and one imported chikungunya case (on Hawaii) has been confirmed. These cases are not associated with the Hawaii island investigation.
Saudi Arabia notified WHO of 5 additional cases of MERS-CoV
Wednesday, February 3rd, 2016Between 22 and 27 January 2016, the National IHR Focal Point for the Kingdom of Saudi Arabia notified WHO of 5 additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection.
Details of the cases
- A 47-year-old male from Al-Kharj city developed symptoms on 24 January and, on 26 January, was admitted to hospital. The patient, who has comorbidities, tested positive for MERS-CoV on 27 January. Currently, he is in stable condition in a negative pressure isolation room on a ward. The patient has a history of frequent contact with camels and consumption of their raw milk. He has no history of exposure to other known risk factors in the 14 days prior to the onset of symptoms.
- A 21-year-old, non-national male from Alkumrah city was identified through contact tracing while asymptomatic. The patient, who has no comorbidities, tested positive for MERS-CoV on 23 January. Currently, he is still asymptomatic and in home isolation. The patient has a history of contact with MERS-CoV positive camels. He has no history of exposure to other known risk factors in the 14 days prior to detection.
- A 45-year-old, non-national male from Alkumrah city was identified through contact tracing while asymptomatic. The patient, who has no comorbidities, tested positive for MERS-CoV on 23 January. Currently, he is still asymptomatic and in home isolation. The patient has a history of contact with MERS-CoV positive camels. He has no history of exposure to other known risk factors in the 14 days prior to detection.
- An 85-year-old male from Muthnab city developed symptoms on 11 January and, on 19 January, was admitted to hospital. The patient, who has comorbidities, tested positive for MERS-CoV on 21 January. Currently, he is in stable condition in a negative pressure isolation room on a ward. The patient has a history of contact with his relatives who have a history of contact with camels. He has no history of exposure to other known risk factors in the 14 days prior to the onset of symptoms.
- A 58-year-old male from Jeddah city developed symptoms on 12 January and, on 19 January, was admitted to hospital. The patient, who has comorbidities, tested positive for MERS-CoV on 21 January. Currently, he is in stable condition in a negative pressure isolation room on a ward. The patient has a history of frequent contact with camels and consumption of their raw milk. He has no history of exposure to other known risk factors in the 14 days prior to the onset of symptoms.
Contact tracing of household and healthcare contacts is ongoing for these cases.
Globally, since September 2012, WHO has been notified of 1,638 laboratory-confirmed cases of infection with MERS-CoV, including at least 587 related deaths.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV early because like other respiratory infections, the early symptoms of MERS-CoV are non-specific. Therefore, health-care workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures.
Until more is understood about MERS-CoV, people with diabetes, renal failure, chronic lung disease, and immunocompromised persons are considered to be at high risk of severe disease from MERS‐CoV infection. Therefore, these people should avoid close contact with animals, particularly camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, or eating meat that has not been properly cooked.
WHO remains vigilant and is monitoring the situation. Given the lack of evidence of sustained human-to-human transmission in the community, WHO does not recommend travel or trade restrictions with regard to this event. Raising awareness about MERS-CoV among travellers to and from affected countries is good public health practice.
A 22-year-old man has contracted the Zika virus in Thailand (a fever, a rash and redness of the eyes and he had not travelled abroad)
Wednesday, February 3rd, 2016‘……Dr Amnuay Gajeena, director-general of the Disease Control Department of the Public Health Ministry said …….”It’s not a new disease in Thailand… we had the first confirmed case in 2012. Since then we have an average of not more than five cases yearly,”…….’

Honduras declares a state of national emergency, saying it has recorded 3,649 suspected cases of Zika virus infections in less than 3 months.
Wednesday, February 3rd, 2016Sanofi Pasteur announced Feb. 2 that it has launched a vaccine research and development project targeting the prevention of Zika virus infection and disease.
Wednesday, February 3rd, 2016Sanofi Pasteur leads the vaccine field for viruses in the same family as Zika virus (ZIKV), with licensed vaccines against Yellow Fever, Japanese Encephalitis and, most recently, Dengue.
The first case of Zika virus disease involving a Dallas County resident who had sexual contact with someone who acquired the Zika infection while traveling abroad.
Wednesday, February 3rd, 2016DSHS Reports First Locally Acquired Zika Case

News Release
Feb. 2, 2016
The Texas Department of State Health Services today reported the first case of Zika virus disease contracted in Texas, involving a Dallas County resident who had sexual contact with someone who acquired the Zika infection while traveling abroad. Case details are being evaluated, but the possibility of sexual transmission from an infected person to a non-infected person is likely in this case.
DSHS has seven other Texas cases of Zika virus disease, all related to foreign travel to areas where Zika is currently being transmitted. Zika virus is transmitted to people primarily through the bite of an infected mosquito, though there also have been reports of transmission through sexual contact. The disease can cause fever, rash, muscle and joint aches and red eyes but also has been linked to the birth defect microcephaly and other poor birth outcomes in some women infected during their pregnancy.
“We’re working closely with our partners to gather more information about the virus and this transmission in Dallas and to determine whether any additional public health interventions are needed,” said Dr. John Hellerstedt, DSHS commissioner.
Texas alerted health care providers in January to be aware of and consider Zika virus as they see patients and is pursuing the ability to test for Zika at the state laboratory in Austin. Testing currently occurs at the Centers for Disease Control and Prevention.
Movies: In 2014, CDC estimated that in the USA alone, exposure to on-screen smoking would recruit more than 6 million new, young smokers from among American children in 2014, of which 2 million would ultimately die from tobacco-induced diseases.
Wednesday, February 3rd, 2016Films showing smoking scenes should be rated to protect children from tobacco addiction
1 FEBRUARY 2016 | GENEVA – WHO is calling on governments to rate movies that portray tobacco use in a bid to prevent children and adolescents from starting to smoke cigarettes and use other forms of tobacco.
Movies showing use of tobacco products have enticed millions of young people worldwide to start smoking, according to the new WHO “Smoke-free movies: from evidence to action”, the third edition since its launch in 2009.
“With ever tighter restrictions on tobacco advertising, film remains one of the last channels exposing millions of adolescents to smoking imagery without restrictions,” says Dr Douglas Bettcher, WHO’s Director for the Department of Prevention of Noncommunicable Diseases.
Taking concrete steps, including rating films with tobacco scenes and displaying tobacco warnings before films with tobacco, can stop children around the world from being introduced to tobacco products and subsequent tobacco-related addiction, disability and death.
“Smoking in films can be a strong form of promotion for tobacco products,” adds Dr Bettcher. “The 180 Parties to the WHO Framework Convention on Tobacco Control (WHO FCTC) are obliged by international law to ban tobacco advertising, promotion and sponsorship.”
Movies hook millions of young people on tobacco
Studies in the United States of America have shown that on-screen smoking accounts for 37% of all new adolescent smokers. In 2014, the US Centers for Disease Control and Prevention estimated that in the United States alone, exposure to on-screen smoking would recruit more than 6 million new, young smokers from among American children in 2014, of which 2 million would ultimately die from tobacco-induced diseases.
“With ever tighter restrictions on tobacco advertising, film remains one of the last channels exposing millions of adolescents to smoking imagery without restrictions.”
Dr Douglas Bettcher, WHO’s Director for the Department of Prevention of Noncommunicable Diseases
In 2014, smoking was found in 44% of all Hollywood films, and 36% of films rated for young people. Almost two thirds (59%) of top-grossing films featured tobacco imagery between 2002 and 2014. That same year, the US Surgeon General reported that adult ratings of future films with smoking would reduce smoking rates among young people in the USA by nearly one-fifth and avert 1 million tobacco-related deaths among today’s children and adolescents.
Many films produced outside of the United States also contain smoking scenes. Surveys have shown that tobacco imagery was found in top-grossing films produced in six European countries (Germany, Iceland, Italy, Poland, the Netherlands and the United Kingdom), and two Latin American countries (Argentina and Mexico). Nine in 10 movies from Iceland and Argentina contain smoking, including films rated for young people, the report states.
The WHO Smoke-Free Movie report, in line with the guidelines of article 13 of the WHO FCTC, recommends policy measures including:
- requiring age classification ratings for films with tobacco imagery to reduce overall exposure of youth to tobacco imagery in films;
- certifying in movie credits that film producers receive nothing of value from anyone in exchange for using or displaying tobacco products in a film;
- ending display of tobacco brands in films; and
- requiring strong anti-smoking advertisements to be shown before films containing tobacco imagery in all distribution channels (cinemas, televisions, online, etc).
In addition, the report also recommends making media productions that promote smoking ineligible for public subsidies.
Dr Armando Peruga, programme manager of WHO’s Tobacco-Free Initiative, says countries around the world have taken steps to limit tobacco imagery in films. “China has ordered that ‘excessive’ smoking scenes should not be shown in films. India has implemented new rules on tobacco imagery and brand display in domestic and imported films and TV programmes. But more can and must be done,” Dr Peruga adds.
CDC adds 4 destinations to interim travel guidance related to Zika virus: American Samoa, Costa Rica, Curacao, and Nicaragua
Tuesday, February 2nd, 2016
CDC is working with other public health officials to monitor for ongoing Zika virus transmission. Today, CDC added the following destinations to the Zika virus travel alerts: American Samoa, Costa Rica, Curacao, and Nicaragua. CDC has issued a travel alert (Level 2-Practice Enhanced Precautions) for people traveling to regions and certain countries where Zika virus transmission is ongoing. For a full list of affected countries/regions: http://www.cdc.gov/zika/geo/index.html. Specific areas where Zika virus transmission is ongoing are often difficult to determine and are likely to continue to change over time.
As more information becomes available, CDC travel alerts will be updated. Travelers to areas where cases of Zika virus infection have been recently confirmed are at risk of being infected with the Zika virus. Mosquitoes that spread Zika are aggressive daytime biters, prefer to bite people, and live indoors and outdoors near people. There is no vaccine or medicine available for Zika virus. The best way to avoid Zika virus infection is to prevent mosquito bites.
Some travelers to areas with ongoing Zika virus transmission will become infected while traveling but will not become sick until they return home. Some people who are infected do not have any symptoms. Symptoms include fever, rash, joint pain, and red eyes. Other commonly reported symptoms include muscle pain and headache. The illness is usually mild with symptoms lasting from several days to a week. Severe disease requiring hospitalization is uncommon and case fatality is low. Travelers to these areas should monitor for symptoms or illness upon return. If they become ill, they should tell their healthcare professional where they have traveled and when.
Until more is known, CDC continues to recommend that pregnant women and women trying to become pregnant take the following precautions:
- Pregnant women should consider postponing travel to the areas where Zika virus transmission is ongoing. Pregnant women who must travel to one of these areas should talk to their doctor or other healthcare professional first and strictly follow steps to avoid mosquito bites during the trip.
- Women trying to become pregnant should consult with their healthcare professional before traveling to these areas and strictly follow steps to prevent mosquito bites during the trip.
Guillain-Barré syndrome (GBS) has been reported in patients with probable Zika virus infection in French Polynesia and Brazil. Because we do not know if Zika virus infection causes GBS, research efforts are underway to examine if there is a potential link between Zika and GBS.
###
WHO statement on the first meeting of the International Health Regulations (2005) (IHR 2005) Emergency Committee on Zika virus and observed increase in neurological disorders and neonatal malformations
Tuesday, February 2nd, 2016The first meeting of the Emergency Committee (EC) convened by the Director-General under the International Health Regulations (2005) (IHR 2005) regarding clusters of microcephaly cases and other neurologic disorders in some areas affected by Zika virus was held by teleconference on 1 February 2016, from 13:10 to 16:55 Central European Time.
The WHO Secretariat briefed the Committee on the clusters of microcephaly and Guillain-Barré Syndrome (GBS) that have been temporally associated with Zika virus transmission in some settings. The Committee was provided with additional data on the current understanding of the history of Zika virus, its spread, clinical presentation and epidemiology.
The following States Parties provided information on a potential association between microcephaly and/or neurological disorders and Zika virus disease: Brazil, France, United States of America, and El Salvador.
The Committee advised that the recent cluster of microcephaly cases and other neurologic disorders reported in Brazil, following a similar cluster in French Polynesia in 2014, constitutes a Public Health Emergency of International Concern (PHEIC).
The Committee provided the following advice to the Director-General for her consideration to address the PHEIC (clusters of microcephaly and neurologic disorders) and their possible association with Zika virus, in accordance with IHR (2005).
Microcephaly and neurologic disorders
- Surveillance for microcephaly and GBS should be standardized and enhanced, particularly in areas of known Zika virus transmission and areas at risk of such transmission.
- Research into the etiology of new clusters of microcephaly and neurologic disorders should be intensified to determine whether there is a causative link to Zika virus and/or other factors or co-factors.
As these clusters have occurred in areas newly infected with Zika virus, and in keeping with good public health practice and the absence of another explanation for these clusters, the Committee highlights the importance of aggressive measures to reduce infection with Zika virus, particularly among pregnant women and women of childbearing age.
As a precautionary measure, the Committee made the following additional recommendations:
Zika virus transmission
- Surveillance for Zika virus infection should be enhanced, with the dissemination of standard case definitions and diagnostics to at-risk areas.
- The development of new diagnostics for Zika virus infection should be prioritized to facilitate surveillance and control measures.
- Risk communications should be enhanced in countries with Zika virus transmission to address population concerns, enhance community engagement, improve reporting, and ensure application of vector control and personal protective measures.
- Vector control measures and appropriate personal protective measures should be aggressively promoted and implemented to reduce the risk of exposure to Zika virus.
- Attention should be given to ensuring women of childbearing age and particularly pregnant women have the necessary information and materials to reduce risk of exposure.
- Pregnant women who have been exposed to Zika virus should be counselled and followed for birth outcomes based on the best available information and national practice and policies.
Longer-term measures
- Appropriate research and development efforts should be intensified for Zika virus vaccines, therapeutics and diagnostics.
- In areas of known Zika virus transmission health services should be prepared for potential increases in neurological syndromes and/or congenital malformations.
Travel measures
- There should be no restrictions on travel or trade with countries, areas and/or territories with Zika virus transmission.
- Travellers to areas with Zika virus transmission should be provided with up to date advice on potential risks and appropriate measures to reduce the possibility of exposure to mosquito bites.
- Standard WHO recommendations regarding disinsection of aircraft and airports should be implemented.
Data sharing
- National authorities should ensure the rapid and timely reporting and sharing of information of public health importance relevant to this PHEIC.
- Clinical, virologic and epidemiologic data related to the increased rates of microcephaly and/or GBS, and Zika virus transmission, should be rapidly shared with WHO to facilitate international understanding of the these events, to guide international support for control efforts, and to prioritize further research and product development.
Based on this advice the Director-General declared a Public Health Emergency of International Concern (PHEIC) on 1 February 2016. The Director-General endorsed the Committee’s advice and issued them as Temporary Recommendations under IHR (2005). The Director-General thanked the Committee Members and Advisors for their advice.
List of Members of, and Advisers to, the International Health Regulations (2005) Emergency Committee on Zika virus and observed increase in neurological disorders and neonatal malformations
1 February 2016
CHAIR
Professor David L. Heymann
Professor of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom of Great Britain and Northern Ireland
MEMBERS
Dr Fernando Althabe
Director, Department of Maternal and Child Health Research, Institute of Clinical and Health Policy Effectiveness, Buenos Aires, Argentina
Dr Kalpana Baruah
Joint Director, National Vector Borne Disease Control Programme, Ministry of Health and Family Welfare, Government of India, New Delhi, India
Dr Silvia Bino
Associate Professor of Infectious Diseases; Head, Control of Infectious Diseases Department, Institute of Public Health, Tirana, Albania
Professor David O. Freedman
Professor of Medicine and Epidemiology, University of Alabama at Birmingham, United States of America
Dr Abraham Hodgson
Director, Research and Development Division, Ghana Health Service, Accra, Ghana
Dr Nyoman Kandun
Program Director, Field Epidemiology Training Program, Ministry of Health, Jakarta, Indonesia
Dr Ghazala Mahmud
Former Dean, Quaid i Azam Post Graduate Medical College, Pakistan Institute of Medical Sciences; Dean, Faculty of Medicine, Quaid i Azam University, Islamabad, Pakistan
Dr K.U. Menon
Senior Consultant, Ministry of Communications and Information, Singapore
Dr Amadou Sall
Director of the WHO Collaborating Centre for Arboviruses and Viral Haemorrhagic Fevers, Institut Pasteur de Dakar, Senegal
Dr Jennifer Staples
Medical Epidemiologist, Arboviral Disease Branch, Division of Vector-borne Diseases, Centers for Disease Control and Prevention, Atlanta, United States of America
Dr Pedro Fernando da Costa Vasconcelos
Head, Department of Arbovirology and Haemorrhagic Fevers; Director, National Reference Laboratory for Arboviruses; Director, National Institute for Viral Haemorrhagic Fevers, Ananindeua, Brazil
ADVISERS
Dr Férechté Encha-Razavi
Associate Professor, University of Paris-Déscartes, and Senior Consultant, Centres Pluridisciplinaires de Diagnostic Prénatal, Necker-Sick Children’s Hospital, Paris, France
Dr Anthony Evans
Aviation Medicine Consultant, International Civil Aviation Organization, Montreal, Canada
Dr Dirk Glaesser
Director, Sustainable Development of Tourism Programme, World Tourism Organization, Madrid, Spain
Professor Duane J. Gubler
Professor and Founding Director, Signature Research Program in Emerging Infectious Diseases, Duke-Nus Graduate Medical School, Singapore
Dr Leonard Mboera
Chief Research Scientist and the Director of Information Technology and Communication, National Institute for Medical Research, Dar es Salaam,Tanzania
Dr James Meegan
National Institute of Allergy and Infectious Diseases, National Institutes of Health, Office of Global Research, Bethesda, United States of America
Dr Maria Mercedes Muñoz
Coordinator, Public Health Surveillance Group, Department of Epidemiology and Demography, Ministry of Health and Welfare, Bogota, Colombia
Dr Rafael Obregón
Chief, Communication for Development Section, United Nations Children’s Fund, New York, United States of America