Archive for February, 2016
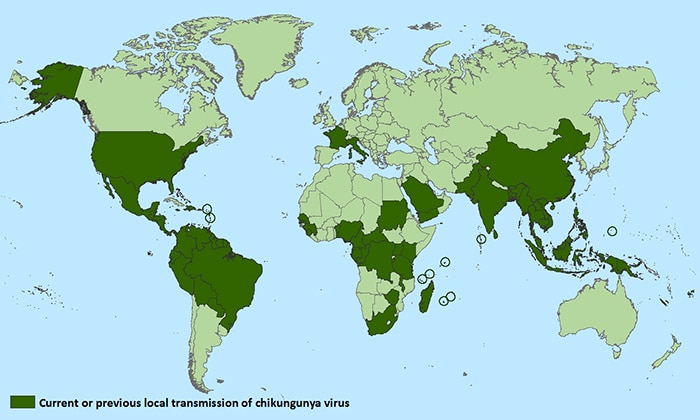
PAHO added 8,279 new chikungunya cases to its list, bringing the 2016 outbreak total to 14,700 confirmed and suspected cases. The new infections bring the overall outbreak total to 1,860,082 chikungunya cases.
Wednesday, February 17th, 2016Syria: 4 hospitals bombed in a single day with at least 50 people (including children) were killed in all of the attacks
Tuesday, February 16th, 2016
** Physicians for Human Rights, an organization that has been tracking attacks on health care workers and infrastructure amid the Syrian conflict, says that 697 health care workers have been killed in 336 attacks on medical sites, the vast majority carried out by the Syrian government and its allies.
** European Medical Corps
Tuesday, February 16th, 2016
| European Commission – Fact Sheet |
EU launches new European Medical Corps to respond faster to emergencies
Brussels, 15 February 2016
The European Union has set up a European Medical Corps (EMC) through which teams and equipment from the EU Member States can be rapidly deployed.
1. What is the European Medical Corps?
The European Union has set up a European Medical Corps (EMC) through which teams and equipment from the EU Member States can be rapidly deployed to provide medical assistance and public health expertise in response to emergencies inside and outside the EU.
The Medical Corps is part of the existing European Emergency Response Capacity (also known as Voluntary Pool), established under the EU Civil Protection Mechanism.
2. Why was the European Medical Corps set up?
A key difficulty during the response to the Ebola virus outbreak was to quickly deploy medical staff and deal with logistical and management challenges. This led Germany and France in late 2014 to propose a “White Helmets” initiative, which laid the foundation of the European Medical Corps.
The European Medical Corps will be Europe’s contribution to the Global Health Emergency Workforce being set up under the helm of the World Health Organization (WHO). The European Medical Corps will significantly increase the availability of doctors and medical equipment in response to emergencies, and will also allow for better planning and preparations for response to emergencies.
3. What kinds of equipment will the European Medical Corps include?
The European Medical Corps will include emergency medical and public health teams, mobile biosafety laboratories, medical evacuation capacities, medical assessment and coordination experts and logistical support teams. These teams could be mobilised for any type of emergency with health consequences, at short notice, when needed.
4. Which EU Member States are taking part?
Currently, as of 15 February, nine Member States have already offered teams and equipment to the European Medical Corps (BE, LU, ES, DE, CZ, FR, NL, FI, SE).
Any country participating in the EU Civil Protection Mechanism can make medical teams and assets available to the European Medical Corps.
5. How can Member States commit to the European Medical Corps?
To be part of the European Medical Corps, teams need to undergo a certification process to ensure they meet strict quality criteria and are trained to work in an international response operation.
In order to meet the criteria, they can benefit from EU financial support.
This support can include:
- 100% financing from the EU budget: adaptation grants for upgrading the teams to an enhanced status of readiness, quality and availability are available
- Up to 100% or 100% financing from the EU budget for activities related to the certification of teams, including training, exercises and workshops.
Teams may be developed at national or regional level by public authorities or other organisations. Their commitment to the European Medical Corps can only be done by the relevant Member States authorities.
Following a successful certification process, the medical response capacity is registered in the European Medical Corps, and it becomes available for deployment in EU emergency response operations.
Once certified and part of the European Medical Corps teams can benefit for up to 85% for transport grants for deployments of the teams to emergencies
6. How does the European Medical Corps operate during an emergency?
Following a successful certification process, the medical response capacity is registered in the European Medical Corps, and it becomes available for deployment in EU emergency response operations.
The deployment of the medical teams is coordinated by the European Commission’s Emergency Response Coordination Centre (ERCC), the operational hub of the EU Civil Protection Mechanism. Member States retain the final decision on deployment and can opt out of a mission if necessary.
In the field, teams will be coordinated through the overall coordination platform set up for the situation in question, be it under the leadership of an affected state or under the UN coordination system.
Once a response capacity is registered in the European Medical Corps, it is expected to be available for coordinated EU missions. Having these teams and experts registered in the European Medical Corps will increase the predictability of EU assistance and will allow for better planning and preparation beforehand.
Hawaii mobilizes to prevent mosquito borne illnesses
Tuesday, February 16th, 2016Governor’s Office News Release: State mobilizes to prevent mosquito borne illnesses
HONOLULU – Gov. David Ige signed an emergency proclamation Friday, as a preventive measure against mosquito borne illnesses that include dengue fever and Zika. This follows the recent decision by the Centers for Disease Control and Prevention (CDC) to open its emergency operations center at Level 1 to prepare for and mitigate the Zika risk.
“There have been no locally acquired Zika cases in the U.S. or Hawai‘i, and we’d like to keep it that way. This is about getting in front of the situation across the state. I will be coordinating planning efforts with the Hawai‘i Emergency Management Agency, all county mayors and Civil Defense coordinators,” said Gov. Ige.
On Hawai‘i Island, dengue fever cases continue to be fewer and farther between. However, the battle is not over and state continues to focus resources to break the cycle of dengue fever infection and transmission.
The emergency proclamation will give the state access to the Major Disaster Fund, the option of waiving certain laws and regulations to expedite the outbreak response if and when needed, as well as pave the way for federal assistance should the state exhaust its resources.
The state previously released the State Health Department from a 5 percent budget restriction ($250,000) to fund costs incurred while responding to the onset of the dengue outbreak.
The state is also releasing the Health Department from another 5 percent restriction ($250,000) to fund eight vector control positions, one entomologist and one communications position.
The emergency proclamation can be found here.
###
Media Contacts:
Jodi Leong
Deputy Communications Director/Press Secretary
Office of the Governor
Office: 808-586-0043
Mobile: 808-798-3929
jodi.c.leong@hawaii.gov
Cindy McMillan
Communications Director
Office of the Governor
Office: 808-586-0012
Mobile: 808-265-7974
cindy.mcmillan@hawaii.gov
Zika virus disease: Interim case definition by HO
Tuesday, February 16th, 2016Zika virus disease
These interim case definitions have been developed for the purpose of providing global standardization for classification and reporting of Zika virus cases. WHO guidance for the surveillance of Zika virus disease is currently being developed.
WHO will periodically review these interim case definitions and update them as new information becomes available.
Suspected case
A person presenting with rash and/or fever and at least one of the following signs or symptoms:
- arthralgia; or
- arthritis; or
- conjunctivitis (non-purulent/hyperaemic).
Probable case
A suspected case with presence of IgM antibody against Zika virus1 and an epidemiological link2
Confirmed case
A person with laboratory confirmation of recent Zika virus infection:
- presence of Zika virus RNA or antigen in serum or other samples (e.g. saliva, tissues, urine, whole blood); or
- IgM antibody against Zika virus positive and PRNT90 for Zika virus with titre ≥20 and Zika virus PRNT90 titre ratio ≥ 4 compared to other flaviviruses; and exclusion of other flaviviruses
Notes
1 With no evidence of infection with other flaviviruses
2 Contact with a confirmed case, or a history of residing in or travelling to an area with local transmission of Zika virus within two weeks prior to onset of symptoms.
WHO has started posting weekly situation updates on outbreaks of Zika virus
Tuesday, February 16th, 2016Vietnam: The Ministry of Health February 13 announced that over 2,200 cases of emergency cases of alcohol poison have been hospitalized during Tet holidays across the country.
Tuesday, February 16th, 2016China notified WHO of 28 additional laboratory-confirmed cases of H7N9 virus, including five deaths.
Monday, February 15th, 2016
Human infection with avian influenza A(H7N9) virus – China
On 5 February 2016, the National Health and Family Planning Commission (NHFPC) of China notified WHO of 28 additional laboratory-confirmed cases of human infection with avian influenza A (H7N9) virus, including five deaths.
Onset dates ranged from 21 December 2015 to 25 January 2016. Cases ranged in age from 14 to 91 years, with a median age of 58 years. Of these 28 cases, 18 (64%) were male. The majority (25 cases, 89%) reported exposure to live poultry or live poultry markets; the exposure history of three cases is unknown or no clear exposure to poultry. No clusters were reported. Cases were reported from six provinces and municipalities: Zhejiang (13), Jiangsu (5), Guangdong (4), Fujian (3), Shanghai (2) and Hunan (1). See attachment for individual case information.
Detailed information concerning these cases can be found in a separate document (see related links).
Public health response
The Chinese Government has taken the following surveillance and control measures:
- strengthening outbreak surveillance and situation analysis;
- reinforcing all efforts on medical treatment; and
- conducting risk communication with the public and dissemination of information.
WHO risk assessment
WHO is assessing the epidemiological situation and conducting further risk assessment based on the latest information. Based on the information received thus far, the overall public health risk from avian influenza A(H7N9) viruses has not changed.
If the pattern of human cases follows the trends seen in previous years, the number of human cases may rise over the coming months. Further sporadic cases of human infection with avian influenza A(H7N9) virus are expected in affected and possibly in the neighboring areas. Should human cases from affected areas travel internationally, their infection may be detected in another country during travels or after arrival. If this were to occur, community level spread is considered unlikely as the virus has not demonstrated the ability to transmit easily among humans.
WHO advice
WHO advises that travellers to countries with known outbreaks of avian influenza should avoid poultry farms, contact with animals in live bird markets, entering areas where poultry may be slaughtered, or contact with any surfaces that appear to be contaminated with faeces from poultry or other animals. Travellers should also wash their hands often with soap and water. Travellers should follow good food safety and good food hygiene practices.
WHO does not advise special screening at points of entry with regard to this event, nor does it currently recommend any travel or trade restrictions. As always, a diagnosis of infection with an avian influenza virus should be considered in individuals who develop severe acute respiratory symptoms while travelling or soon after returning from an area where avian influenza is a concern.
WHO encourages countries to continue strengthening influenza surveillance, including surveillance for severe acute respiratory infections (SARI) and to carefully review any unusual patterns, in order to ensure reporting of human infections under the IHR (2005), and continue national health preparedness actions.
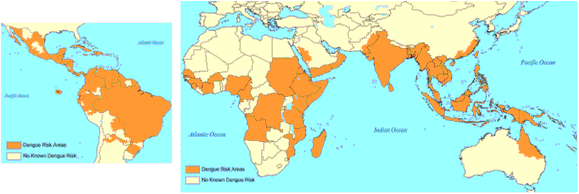
** Dengue’s global burden: The dengue incidence has increased six-fold from 1990 to 2013
Monday, February 15th, 2016“…..We estimated an average of 9221 dengue deaths per year between 1990 and 2013, increasing from a low of 8277 (95% uncertainty estimate 5353–10 649) in 1992, to a peak of 11 302 (6790–13 722) in 2010. This yielded a total of 576 900 (330 000–701 200) years of life lost to premature mortality attributable to dengue in 2013. The incidence of dengue increased greatly between 1990 and 2013, with the number of cases more than doubling every decade, from 8·3 million (3·3 million–17·2 million) apparent cases in 1990, to 58·4 million (23·6 million–121·9 million) apparent cases in 2013. When accounting for disability from moderate and severe acute dengue, and post-dengue chronic fatigue, 566 000 (186 000–1 415 000) years lived with disability were attributable to dengue in 2013. Considering fatal and non-fatal outcomes together, dengue was responsible for 1·14 million (0·73 million–1·98 million) disability-adjusted life-years in 2013…..the true symptomatic incidence of dengue probably falls within the commonly cited range of 50 million to 100 million cases per year. ”
** Many of the fatal dengue cases in 2013 occurred in Southeast Asia (5,376 deaths) and South Asia (2,132 deaths).
** Death rates in tropical and central Latin America and the Caribbean increased from 1990 to 2013
** Most dengue-related deaths (7,018) in 2013 occurred in individuals belonging to the lower middle-class income group.
** The researchers acknowledge that their models resulted in estimates of mortality incidence that are significantly lower than the World Health Organization’s estimate of 10,000 to 20,000 deaths caused by dengue each year.
Reviewing the epidemiology of MERS-CoV in Saudi Arabia from 2012 when the first MERS-CoV was confirmed up to July 2015.
Monday, February 15th, 2016International Journal of Infectious Diseases
“…..In this series, we described the risk factors and outcomes of 939 cases of MERS coronavirus in the last 3 years. The majority of the affected patients were in age of 40 years and above 65 (70%). From those 657 patients, 377 (57.3%) died….Our findings confirm the association of severe MERS coronavirus illness in patient who has pre-existent health morbidity….. ”