Archive for August, 2016
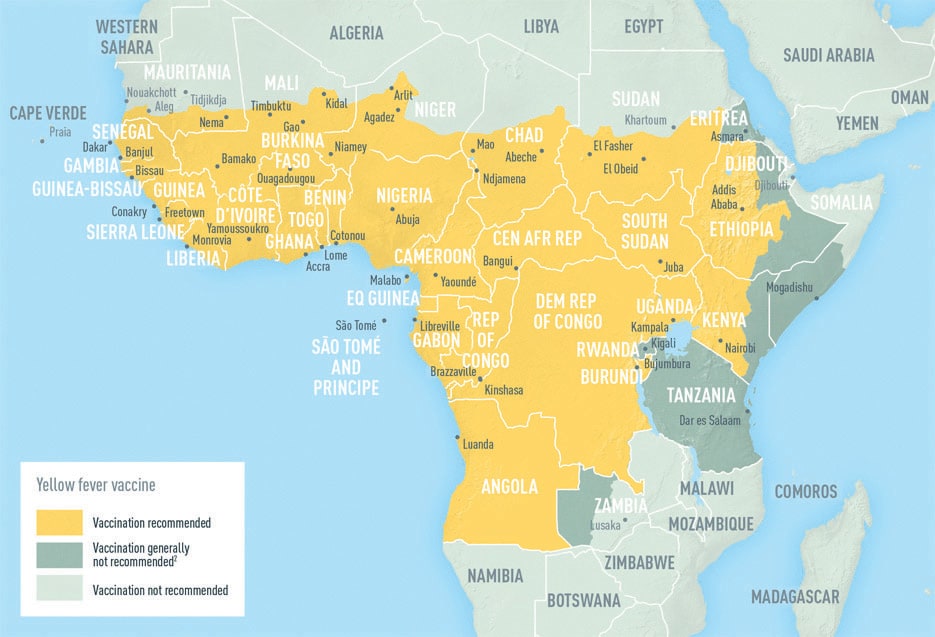
Since December 2015, Angola has reported 3,867 yellow fever cases, 879 of them confirmed & as of Aug 8 the DRC had reported 2,269 cases, 74 of them confirmed.
Sunday, August 14th, 2016Heavy rains drenched parts of SE Louisiana and southern Mississippi on Friday, causing dangerous floods that killed at least three people, cut off an entire town, shut down highways and prompted numerous rescues.
Saturday, August 13th, 2016Canada: Public Health Notice – Outbreak of Cyclospora under investigation
Saturday, August 13th, 2016Public Health Agency of Canada
Why you should take note?
The Public Health Agency of Canada is collaborating with provincial public health partners, the Canadian Food Inspection Agency, and Health Canada to investigate locally-acquired Cyclospora infections in four provinces. The source of the outbreak has not been identified. Imported fresh produce products are currently items of interest in the ongoing investigation. This Notice will be updated as new information becomes available.
Cyclospora is a microscopic single-celled parasite that is passed in people’s feces. If it comes in contact with food or water, it can infect the people who consume it. This causes an intestinal illness called cyclosporiasis.
Cyclospora is not common on food and is not in drinking water in Canada. The parasite is most common in some tropical and subtropical countries such as Peru, Cuba, India, Nepal, Mexico, Guatemala, Southeast Asia and Dominican Republic. In Canada, non-travel related illnesses due to Cyclospora occur more frequently in the spring and summer months. Illnesses among travellers can happen at any time of year.
Investigation Summary
In Canada, a total of 51 cases have been reported: in British Columbia (1), Alberta (2), Ontario (44), and Quebec (4). Individuals became sick between May and July 2016. The majority of cases are male (51%), with an average age of 49 years. One case was hospitalized. The investigation into the source of the outbreak is ongoing. To date, no multi-jurisdictional outbreaks of Cyclospora have been linked to produce grown in Canada.
Previous foodborne illness outbreaks of Cyclospora in Canada and US have been linked to various types of imported fresh produce, such as pre-packaged salad mix, basil, cilantro, raspberries, blackberries, mesclun lettuce and snow and snap peas.
Who is most at risk?
People living or traveling in tropical or subtropical regions of the world who eat fresh produce or drink untreated water may be at increased risk for infection because the parasite is found in some of these regions.
Most people recover fully, however, it may take several weeks before an ill person’s intestinal problems completely disappear.
What you should do to protect your health?
It can be hard to prevent cyclosporiasis. This is because washing produce does not always get rid of the Cyclospora parasite that causes the illness. You can reduce your risk by:
- cooking produce imported from countries where Cyclospora is found; and
- consuming fresh produce grown in countries where Cyclospora is not common, such as Canada, the United States, and European countries.
When travelling to a country where Cyclospora is found, you can reduce your risk by:
- avoiding food that has been washed in local drinking water;
- drinking water from a safe source; and
- eating cooked food or fruit that you can peel yourself.
Symptoms
People infected with Cyclospora can experience a wide range of symptoms. Some do not get sick at all, while others feel as though they have a bad case of stomach flu. Few people get seriously ill.
Most people develop the following symptoms within one week after being infected with Cyclospora:
- watery diarrhea
- abdominal bloating and gas
- fatigue (tiredness)
- stomach cramps
- loss of appetite
- weight loss
- mild fever
- nausea
When you eat or drink contaminated food or water, it may take 7 to 14 days for symptoms to appear. If left untreated, you may have the symptoms for a few days up to a few months. Most people have symptoms for 6 to 7 weeks. Sometimes, symptoms may go away and then return.
If you become ill, drink plenty of water or fluids to prevent dehydration from diarrhea. If you have signs of illness and have reason to believe you have cyclosporiasis, call your health care provider.
What the Government of Canada is doing
The Government of Canada is committed to food safety. The Public Health Agency of Canada leads human health investigations of outbreaks and is in regular contact with its federal and provincial partners to monitor and take collaborative steps to address outbreaks.
Health Canada provides food-related health risk assessments to determine if the presence of a certain substance or microorganism poses a health risk to consumers.
The Canadian Food Inspection Agency (CFIA) conducts food safety investigations into the possible food source of an outbreak.
The Government of Canada will continue to update Canadians if new information related to this investigation becomes available.
Additional Information
Media Contact
Public Health Agency of Canada
Media Relations
(613) 957-2983
Public Inquiries
Call toll-free: 1-866-225-0709
Email: info@hc-sc.gc.ca
WHO: Zika report around the world
Saturday, August 13th, 2016Summary
- As of 10 August 2016, 69 countries and territories (Fig. 1, Table 1) have reported evidence of mosquito-borne Zika virus transmission since 2007 (66 of these countries and territories have reported evidence of mosquito-borne Zika virus transmission since 2015):
- 52 countries and territories with a first reported outbreak from 2015 onwards (Table 1).
- Four countries are classified as having possible endemic transmission or have reported evidence of local mosquito-borne Zika infections in 2016.
- 13 countries and territories have reported evidence of local mosquito-borne Zika infections in or before 2015, but without documentation of cases in 2016, or with the outbreak terminated.

- The Cayman Islands, a British Overseas Territory in the Caribbean, is the latest territory to report locally-acquired mosquito borne Zika virus infection.
- Since February 2016, 11 countries have reported evidence of person-to-person transmission of Zika virus, probably via a sexual route (Table 2).
- As of 10 August 2016, 15 countries or territories have reported microcephaly and other central nervous system (CNS) malformations potentially associated with Zika virus infection or suggestive of congenital infection. Canada is the latest country to report a case of congenital malformation associated with a travel-related case of Zika virus infection. Four of the 15 total countries reported microcephaly cases born from mothers in countries with no endemic Zika virus transmission but who reported recent travel history to Zika-affected countries in the WHO Region of the Americas (Table 3).
- As of 10 August 2016, the United States Centers for Disease Control and Prevention (US-CDC) reported 15 live-born infants with birth defects and six pregnancy losses with birth defects with laboratory evidence of Zika virus infection.
- As of 10 August 2016, 16 countries and territories worldwide have reported an increased incidence of Guillain-Barré syndrome (GBS) and/or laboratory confirmation of a Zika virus infection among GBS cases (Table 4). Grenada is the latest country to report a case of GBS associated with a confirmed Zika virus infection.
- In Guinea-Bissau, on 29 June 2016, Institute Pasteur Dakar (IPD) laboratory technicians confirmed that three of 12 samples tested positive for Zika by PC-R. All 12 samples tested negative against IgM Zika. One additional sample from a recent case also tested positive for Zika virus infection. All four samples were sent to IPD on 1 July for gene sequencing and the results are pending. Results from the 22 additional samples collected from the Bijagos archipelago and sent to IPD are negative with ELISA and PCR testing. The same samples were also sent to Dakar for confirmation. A further total of 12 new samples were collected and results are still pending.
- Two cases of microcephaly have been reported in the Western region of Gabu in Guinea-Bissau. The family members of the two children with microcephaly have not travelled outside Guinea-Bissau. The investigations regarding these two cases are ongoing. Trainings for regional health staff on the Zika case definition and other areas are planned to help ensure that cases are detected efficiently and effectively.
- The joint mission by staff from the WHO Regional Office for Africa and from WHO headquarters to Guinea-Bissau has concluded and priority activities and gaps were identified as the following: additional financial resources to reinforce leadership and coordination mechanisms of the Emergency operations Centre (EOC); reinforcement of epidemiologic and entomologic surveillance systems; increasing laboratory capacity at three levels; strengthening of response to Zika cases in terms of detection, community involvement and risk communication; and continued monitoring of Zika virus and its complications.
- Zika virus test kits have been made available by the local authorities at the Central Public Health Laboratory in Rio de Janeiro in Brazil and symptomatic athletes, volunteers, visitors and residents are encouraged to get tested.
- WHO has developed advice and information on diverse topics in the context of Zika virus.
CDC: Zika Cases in the US as of August 10, 2016 (5 am EST)
Saturday, August 13th, 2016As of August 10, 2016 (5 am EST)
- Zika virus disease and Zika virus congenital infection are nationally notifiable conditions.
- This update from the CDC Arboviral Disease Branch includes provisional data reported to ArboNET for January 01, 2015 – August 10, 2016.
US States
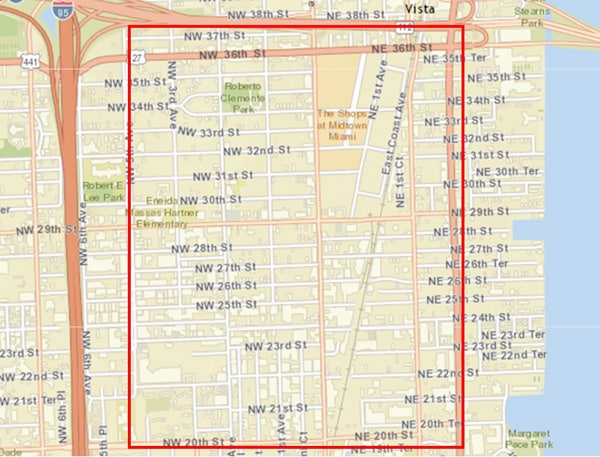
- Locally acquired mosquito-borne cases reported: 6
- Travel-associated cases reported: 1,955
- Laboratory acquired cases reported: 1
- Total: 1,962
- Sexually transmitted: 22
- Guillain-Barré syndrome: 6
US Territories
- Locally acquired cases reported: 6,587
- Travel-associated cases reported: 31
- Total: 6,618*
- Guillain-Barré syndrome: 20
*Sexually transmitted cases are not reported for areas with local mosquito-borne transmission of Zika virus because it is not possible to determine whether infection occurred due to mosquito-borne or sexual transmission
Social Media: Citizens of Nice took to Facebook to use its Safety Check feature to post that they were safe, and to make sure friends and family had checked in OK.
Saturday, August 13th, 2016“….This type of organic social media communication also happened after the Boston Marathon bombing: People near the explosions quickly posted Twitter messages identifying the location and specifics of events, as well as their own whereabouts and safety….”
FEMA app: https://www.fema.gov/mobile-app
Ubalert: http://www.ubalert.com/
The German government proposed a broad range of measures on Thursday to bolster security and combat terrorism
Friday, August 12th, 2016The proposals announced by the interior minister, Thomas de Maizière, call for:
- hiring more federal police officers;
- making it a crime to express sympathy for terrorism;
- greater sharing of intelligence data across Europe;
- closer watching of the “dark web,” the part of the internet that is invisible to ordinary users;
- stripping dual citizens of their German citizenship if they fight for extremist groups; and
- making it easier to deport foreigners deemed to be dangerous.