Archive for February, 2017
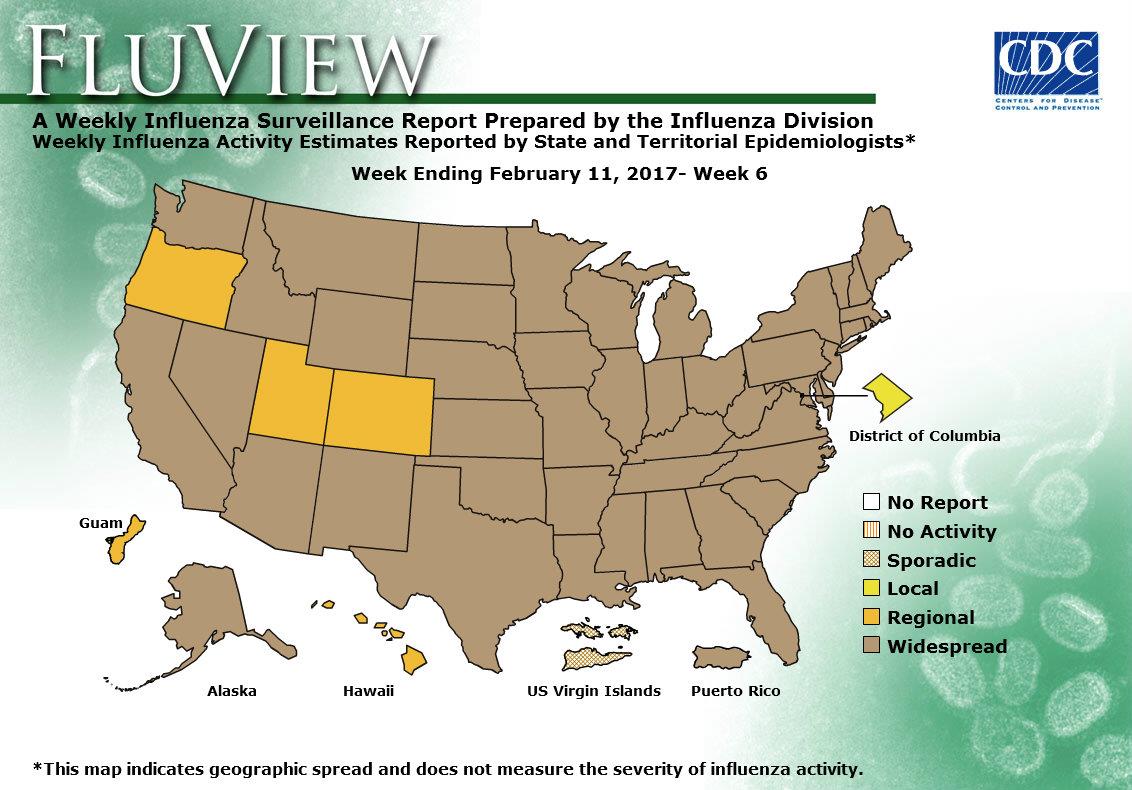
2016-2017 Influenza Season Week 6 ending February 11, 2017
Saturday, February 18th, 2017During week 6 (February 5-11, 2017), influenza activity increased in the United States.
- Viral Surveillance: The most frequently identified influenza virus subtype reported by public health laboratories during week 6 was influenza A (H3). The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased.
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was above the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Nine influenza-associated pediatric deaths were reported.
- Influenza-associated Hospitalizations:A cumulative rate for the season of 29.4 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) was 5.2%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above their region-specific baseline levels. New York City and 28 states experienced high ILI activity; Puerto Rico and seven states experienced moderate ILI activity; five states experienced low ILI activity; nine states experienced minimal ILI activity; and the District of Columbia had insufficient data.
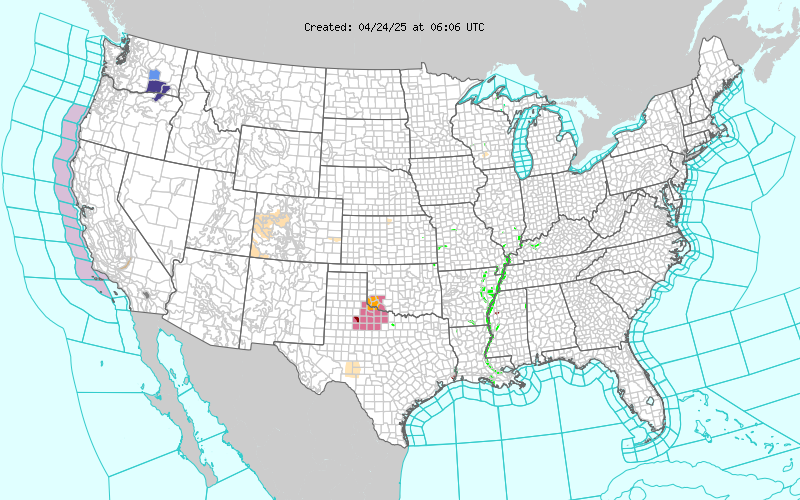
- Geographic Spread of Influenza: The geographic spread of influenza in Puerto Rico and 46 states was reported as widespread; Guam and four states reported regional activity; the District of Columbia reported local activity; and the U.S. Virgin Islands reported sporadic activity.
California: A “bombogenesis” or “weather bomb” – has killed 4 so far, and brought torrential rain and flash floods.
Saturday, February 18th, 2017CDC/FDA: The incidence of US disease outbreaks related to imported food has increased in recent years, with fish and produce most commonly implicated.
Saturday, February 18th, 2017Outbreaks of Disease Associated with Food Imported into the United States, 1996–2014
| EID | Gould L, Kline J, Monahan C, Vierk K. Outbreaks of Disease Associated with Food Imported into the United States, 1996–2014. Emerg Infect Dis. 2017;23(3):525-528. https://dx.doi.org/10.3201/eid2303.161462 |
|---|---|
| AMA | Gould L, Kline J, Monahan C, et al. Outbreaks of Disease Associated with Food Imported into the United States, 1996–2014. Emerging Infectious Diseases. 2017;23(3):525-528. doi:10.3201/eid2303.161462. |
| APA | Gould, L., Kline, J., Monahan, C., & Vierk, K. (2017). Outbreaks of Disease Associated with Food Imported into the United States, 1996–2014. Emerging Infectious Diseases, 23(3), 525-528. https://dx.doi.org/10.3201/eid2303.161462. |
Abstract
The proportion of US food that is imported is increasing; most seafood and half of fruits are imported. We identified a small but increasing number of foodborne disease outbreaks associated with imported foods, most commonly fish and produce. New outbreak investigation tools and federal regulatory authority are key to maintaining food safety.
Approximately 19% of food consumed in the United States is imported, including ≈97% of fish and shellfish, ≈50% of fresh fruits, and ≈20% of fresh vegetables (1). The proportion of food that is imported has increased steadily over the past 20 years because of changing consumer demand for a wider selection of food products and increasing demand for produce items year round (1).
The Centers for Disease Control and Prevention (CDC) defines a foodborne disease outbreak as the occurrence of >2 persons with a similar illness resulting from ingestion of a common food (2). Local, state, and territorial health departments report foodborne disease outbreaks to CDC through the Foodborne Disease Outbreak Surveillance System. The information collected for each outbreak includes etiology (confirmed or suspected on the basis of predefined criteria) (2), year, month, state, implicated food, and number of illnesses, hospitalizations, and deaths. Information is also collected on where implicated food originated. During 1973–1997, this information was reported anecdotally in the report’s comments section. During 1998–2008, “contaminated food imported into U.S.” was included as a location where food was prepared. Since 2009, the form has included a variable to indicate whether an implicated food was imported into the United States and the country of origin.
We reviewed outbreak reports to identify outbreaks associated with an imported food from the inception of the surveillance system in 1973 through 2014, the most recent year for which data were available. We obtained additional data for some outbreaks (e.g., country of origin) from the US Food and Drug Administration (FDA) and the US Department of Agriculture Food Safety and Inspection Service.
We categorized implicated foods by using the schema developed by the Interagency Food Safety Analytics Collaboration (3). We grouped countries using the United Nations Statistics Division classification (4). We conducted a descriptive analysis of the number of outbreaks over time, by food category, and by region of origin.
Figure
 Figure(https://wwwnc.cdc.gov/eid/article/23/3/16-1462-f1). Number of outbreaks caused by imported foods and total number of outbreaks with a food reported, United States, 1996–2014. Reporting practices changed over time; 1973–1997, imported foods anecdotally noted in report…
Figure(https://wwwnc.cdc.gov/eid/article/23/3/16-1462-f1). Number of outbreaks caused by imported foods and total number of outbreaks with a food reported, United States, 1996–2014. Reporting practices changed over time; 1973–1997, imported foods anecdotally noted in report…
During 1996–2014, a total of 195 outbreak investigations implicated an imported food, resulting in 10,685 illnesses, 1,017 hospitalizations, and 19 deaths. Outbreaks associated with imported foods represented an increasing proportion of all foodborne disease outbreaks where a food was implicated and reported (1% during 1996–2000 vs. 5% during 2009–2014). The number of outbreaks associated with an imported food increased from an average of 3 per year during 1996–2000 to an average of 18 per year during 2009–2014 (Figure).
The most common agents reported in outbreaks associated with imported foods were scombroid toxin and Salmonella; most illnesses were associated with Salmonella and Cyclospora (Table(https://wwwnc.cdc.gov/eid/article/23/3/16-1462-t1)). Aquatic animals were responsible for 55% of outbreaks and 11% of outbreak-associated illnesses. Produce was responsible for 33% of outbreaks and 84% of outbreak-associated illnesses. Outbreaks attributed to produce had a median of 40 illnesses compared with a median of 3 in outbreaks attributed to aquatic animals. All but 1 of the outbreaks caused by scombroid toxin was associated with fish. Most of the Salmonella outbreaks (77%) were associated with produce, including fruits (n = 14), seeded vegetables (n = 10), sprouts (n = 6), nuts and seeds (n = 5), spices (n = 4), and herbs (n = 1).
Information was available on the region of origin for 177 (91%) outbreaks. Latin America and the Caribbean was the most common region implicated, followed by Asia (Technical Appendix(https://wwwnc.cdc.gov/eid/article/23/3/16-1462-techapp1.xlsx)). Thirty-one countries were implicated; Mexico was most frequently implicated (42 outbreaks). Other countries associated with >10 outbreaks were Indonesia (n = 17) and Canada (n = 11). Fish and shellfish originated from all regions except Europe but were most commonly imported from Asia (65% of outbreaks associated with fish or shellfish). Produce originated from all regions but was most commonly imported from Latin America and the Caribbean (64% of outbreaks associated with produce). All but 1 outbreak associated with dairy products involved products imported from Latin America and the Caribbean.
Outbreaks in this analysis were reported from 31 states, most commonly California (n = 30), Florida (n = 25), and New York (n = 16). Forty-three outbreaks (22%) were multistate outbreaks.
The number of reported outbreaks associated with imported foods, although small, has increased as an absolute number and in proportion to the total number of outbreaks in which the implicated food was identified and reported. Although many types of imported foods were associated with outbreaks, fish and produce were most common. These findings are consistent with overall trends in food importation (5).
Many outbreaks, particularly outbreaks involving produce, were associated with foods imported from countries in Latin America and the Caribbean. Because of their proximity, these countries are major sources of perishable items such as fresh fruits and vegetables; Mexico is the source of about one quarter of the total value of fruit and nut imports and 45%–50% of vegetable imports, followed by Chile and Costa Rica. Similarly, our finding that many outbreaks were associated with fish from Asia is consistent with data on the sources of fish imports (6).
One quarter of the outbreaks were multistate, reflecting the wide distribution of many imported foods. Systems like PulseNet have helped to improve detection and investigation of multistate outbreaks, resulting in an increased number of multistate outbreaks (7,8). The increasing number of outbreaks involving globally distributed foods underscores the need to strengthen regional and global networks for outbreak detection and information sharing. The importance of having standard protocols for molecular characterization of isolates and systems for rapid traceability of implicated foods to their source was illustrated during the investigation of a listeriosis outbreak linked to Italian cheese imported into the United States in 2012 (9). Newer tools like whole genome sequencing can also help to generate hypothetical transmission networks and in some instances facilitate traceback of foods to their origin (10). Moreover, new tools that aid visualization of supplier networks facilitate the investigation of outbreaks involving the increasingly complex global economy (11).
Nearly all of the outbreaks involved foods under FDA jurisdiction. Only a small proportion of FDA-regulated foods are inspected upon entry into the United States. New rules under the Food Safety Modernization Act of 2011, including the Preventive Controls Rule for Human Food, Produce Safety Rule, Foreign Supplier Verification Program, and Accreditation of Third Party Auditors, will help to strengthen the safety of imported foods by granting FDA enhanced authorities to require that imported foods meet the same safety standards as foods produced domestically (12).
Although data collection has improved in recent years, these findings might underestimate the number of outbreaks associated with imported foods because the origin of only a small proportion of foods causing outbreaks is reported. Similarly, because of how data are collected and reported, the relative safety of imported and domestically produced foods cannot be compared. Because of changes in surveillance and changing import patterns, changes over time should be interpreted cautiously.
Our findings reflect current patterns in food imports and provide information to help guide future outbreak investigations. Prevention focused on the most common imported foods causing outbreaks, produce and seafood, could help prevent outbreaks. Efforts to improve the safety of the food supply can include strengthening reporting by gathering better data on the origin of implicated food items, including whether imported and from what country.
Dr. Gould served as a team lead in the Enteric Diseases Epidemiology Branch, Division of Foodborne, Waterborne, and Environmental Diseases, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention. Her research interests focus on ways to improve surveillance for foodborne illness and understanding the impact of changes in food production on outbreaks and illnesses.
References
- US Department of Agriculture. Import share of consumption. 2016 [cited 2016 Aug 12]. http://www.ers.usda.gov/topics/international-markets-trade/us-agricultural-trade/import-share-of-consumption.aspx
- Gould LH, Walsh KA, Vieira AR, Herman K, Williams IT, Hall AJ, et al.; Centers for Disease Control and Prevention. Surveillance for foodborne disease outbreaks – United States, 1998-2008. MMWR Surveill Summ. 2013;62:1–34.PubMed
- Interagency Food Safety Analytics Collaboration. Completed projects: improve the food categories used to estimate attribution [cited 2015 Nov 5]. http://www.cdc.gov/foodsafety/ifsac/projects/completed.html
- United Nations Statistics Division. Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings [cited 2015 Sep 15]. http://unstats.un.org/unsd/methods/m49/m49regin.htm#americas
- Brooks N, Regmi A, Jerardo AUS. food import patterns, 1998–2007 [cited 2015 Sep 15]. https://naldc.nal.usda.gov/download/32182/PDF
- US Department of Agriculture. U.S. Agricultural trade: imports [cited 2015 Nov 5]. http://www.ers.usda.gov/topics/international-markets-trade/us-agricultural-trade/imports.aspx
- Crowe SJ, Mahon BE, Vieira AR, Gould LH. Vital Signs: multistate foodborne outbreaks—United States, 2010–2014. MMWR Morb Mortal Wkly Rep. 2015;64:1221–5. DOIPubMed
- Nguyen VD, Bennett SD, Mungai E, Gieraltowski L, Hise K, Gould LH. Increase in multistate foodborne disease outbreaks—United States, 1973–2010. Foodborne Pathog Dis. 2015;12:867–72. DOIPubMed
- Acciari VA, Iannetti L, Gattuso A, Sonnessa M, Scavia G, Montagna C, et al. Tracing sources of Listeria contamination in traditional Italian cheese associated with a US outbreak: investigations in Italy. Epidemiol Infect. 2016;144:2719–27. DOIPubMed
- Hoffmann M, Luo Y, Monday SR, Gonzalez-Escalona N, Ottesen AR, Muruvanda T, et al. Tracing origins of the Salmonella Bareilly strain causing a food-borne outbreak in the United States. J Infect Dis. 2016;213:502–8. DOIPubMed
- Weiser AA, Gross S, Schielke A, Wigger JF, Ernert A, Adolphs J, et al. Trace-back and trace-forward tools developed ad hoc and used during the STEC O104:H4 outbreak 2011 in Germany and generic concepts for future outbreak situations. Foodborne Pathog Dis. 2013;10:263–9. DOIPubMed
- US Food and Drug Administration. FDA Issues Two Proposed Rules under FSMA to strengthen the oversight of imported foods [cited 2015 Nov 5]. http://www.fda.gov/Food/NewsEvents/ConstituentUpdates/ucm362532.htm
Figure
Table
Technical Appendix
1Preliminary results from this study were presented at the International Conference on Emerging Infectious Diseases, March 11–14, 2012, Atlanta, Georgia, USA.
2Current affiliation: New York City Department of Mental Health and Hygiene, Queens, New York, USA.
Another series of powerful Pacific storms will bring heavy rain and strong winds to the west coast. Additional floods, flash floods, and mudslides along the west coast possible, especially Friday through Saturday.
Friday, February 17th, 2017A surge of H7N9 avian flu activity in China that began in December shows no sign of tailing off, with 61 new cases reported last week, pushing the mainland’s total to at least 419 cases—100 more than the previous high reported during the second wave in 2013-14.
Friday, February 17th, 2017“According to the Chinese Center for Disease Control and Prevention, about 90 per cent of the patients in the Mainland reported exposure to live poultry, mostly with exposure to live poultry markets (LPMs). There was also an increase in environmental contamination with H7N9 virus as reflected by the positive rate of environmental samples collected from LPMs or other live poultry-related environments in affected provinces,” the spokesman said.”
Interim influenza vaccine effectiveness estimates for the 2016–17 season indicate that vaccination reduced the risk for influenza-associated medical visits by approximately half.
Friday, February 17th, 2017Flannery B, Chung JR, Thaker SN, et al. Interim Estimates of 2016–17 Seasonal Influenza Vaccine Effectiveness — United States, February 2017. MMWR Morb Mortal Wkly Rep 2017;66:167–171. DOI: http://dx.doi.org/10.15585/mmwr.mm6606a3.
“Influenza activity in the United States began to increase in mid-December, remained elevated through February 4, 2016, and is expected to continue for several more weeks. During October 2, 2016–February 4, 2017, influenza A (H3N2) viruses were identified most frequently, but influenza A (H1N1)pdm09 and influenza B viruses were also reported. No antiviral resistance to oseltamivir, zanamivir, or peramivir has been identified among influenza viruses tested to date.”
A bomber blew himself up among devotees in the shrine of Sufi saint Lal Shahbaz Qalandar in the town of Sehwan, Pakistan killing at least 50.
Thursday, February 16th, 2017At least 45 people were killed and dozens more injured when a bomb detonated at a popular car market in southwestern Baghdad on Thursday evening
Thursday, February 16th, 2017Scientists may have solved the mystery of nodding syndrome, a rare form of epilepsy that has disabled thousands of children in East Africa.
Thursday, February 16th, 2017“…..Nodding syndrome is a unique seizure disorder affecting children in parts of East Africa. The cause of nodding syndrome has been an enigma, although an epidemiological association with the parasite Onchocerca volvulus has been established. Johnson et al. demonstrate that patients with nodding syndrome have autoantibodies to leiomodin-1 that are neurotoxic in vitro and that leiomodin-1 is expressed in regions of the brain affected during disease. Leiomodin-1 antibodies cross-react with O. volvulus proteins, linking the parasite to the autoantibody. Thus, nodding syndrome may be an autoimmune epilepsy initiated by a parasitic infection and may be preventable by treatment with antiparasitic strategies such as the drug ivermectin…..”
A malaria vaccine was completely successful in preventing the disease in 35 humans
Thursday, February 16th, 2017Sterile protection against human malaria by chemoattenuated PfSPZ vaccine
Nature Year published:(2017)
DOI:doi:10.1038/nature21060
“…..PfSPZ-CVac is a highly efficacious vaccine candidate; when we are able to optimize the immunization regimen (dose, interval between doses, and drug partner), this vaccine could be used for combination mass drug administration and a mass vaccination program approach to eliminate malaria from geographically defined areas……”