Archive for March, 2017
The WHO weighed in on 84 recently reported H7N9 cases reported by China, including a recent imported case from Hong Kong, noting three possible human-to-human illness clusters.
Friday, March 17th, 2017Human infection with avian influenza A(H7N9) virus – China
Between 24 February and 7 March 2017, a total of 58 additional laboratory-confirmed cases of human infection have been reported to WHO from mainland China and China, Hong Kong Special Administrative Region (SAR).
On 24 February 2017, the National Health and Family Planning Commission of China (NHFPC) notified WHO of 35 additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus. On 3 March 2017, the NHFPC notified WHO of 22 additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus. On 7 March 2017, the Department of Health, China, Hong Kong SAR confirmed a case of human infection with avian influenza A(H7N9) virus.
Details of the cases
Between 24 February and 3 March 2017, the NHFPC reported a total of 57 human cases of infection with avian influenza A(H7N9) virus. Onset dates of the cases ranged from 26 January to 27 February 2017. Of these 57 cases, 13 were female. Cases range in age from 4 to 81 years and the median age is 56 years. The cases are reported from Anhui (9), Beijing (1), Fujian (1), Guangdong (11), Guangxi (4), Guizhou (2), Henan (3), Hunan (3), Hubei (2), Jiangsu (7), Jiangxi (4), Shandong (2), Shanghai (1), Sichuan (2), and Zhejiang (5).
At the time of notification, there were 11 deaths, and 39 cases diagnosed as either pneumonia (7) or severe pneumonia (32). One case has mild symptoms. The clinical presentations of the other six (6) cases are not available at this time. Forty-three cases are reported to have had exposure to poultry or live poultry market, four (4) cases have possibility of human to human transmission (among them, two cases also had exposure history to poultry or live poultry market), four (4) had no exposure to poultry and for eight (8) the possible exposures are unknown or under investigation.
On 24 February 2017, two clusters of possible human to human transmission were reported.
First cluster:
- A 40-year-old male from Jiangsu Province, and relative of the 63-year old female described below. He had symptom onset on 26 January 2017 and was admitted to hospital. He bought a live chicken on 24 January 2017.
- A 63-year-old female from Zhejiang Province. She had symptom onset on 10 February 2017, and was admitted to hospital for pneumonia. She had exposure to domestic poultry (farmer by trade) and contact with her son.
All 21 contacts of these 2 cases were healthy and did not develop any symptoms.
Second cluster:
- A 29-year-old male from Anhui Province. He had symptom onset on 3 February 2017, and was admitted to hospital for severe pneumonia. He had exposure to live poultry before onset of disease.
- A 62-year-old female from Anhui Province. She was admitted to the same hospital as the 29-year old male case mentioned above for chronic cough. She had been on the same ward for one day. After initial improvement her condition worsened and she passed away on 16 February 2017.
- A 58-year-old male from Anhui Province, the father of the 29-year-old male case mentioned above. He had symptom onset on 17 February 2017 and was admitted to hospital. He had exposure to live poultry on 31 January 2017 but took also care for his sick son.
All 32 contacts of these 3 cases were healthy and did not develop any symptoms.
On 3 March 2017, one cluster of possible human to human transmission was reported.
- A 60-year-old male from Anhui Province, and grandfather of the 10-year-old male described below. He had symptoms onset on 24 February 2017 and was admitted to a hospital on 25 February 2017. He passed away on 1 March. He had exposure to live poultry.
- A 10-year-old male from Anhui Province. He had symptoms onset on 27 February 2017, and was admitted to hospital on 1 March 2017 for pneumonia. He also had a history of exposure to live poultry.
On 7 March 2017, the Department of Health, China, Hong Kong SAR confirmed a case of human infection with avian influenza A(H7N9) virus in a 76-year-old man with underlying illnesses. The patient travelled to Fuzhou, Fujian between 11 February and 1 March 2017 and he visited a wet market there.
He developed symptoms on 3 March 2017. His nasopharyngeal aspirate specimen tested positive for avian influenza A(H7N9) on 7 March 2017. His clinical diagnosis is pneumonia and he is now in a critical condition. The patient’s close contact has remained asymptomatic so far and has been put under medical surveillance. Tracing of his other contacts in China, Hong Kong SAR is underway.
To date, a total of 1281 laboratory-confirmed human infections with avian influenza A(H7N9) virus have been reported through IHR notification since early 2013.
Public health response
Considering the increase in the number of human infections with avian influenza A(H7N9) since December 2016, the Chinese government has enhanced measures such as:
- The NHFPC strengthened epidemic surveillance, conducted timely risk assessment and analysed the information for any changes in epidemiology.
- The NHPFC requested local NHFPCs to implement effective control measures on the source of outbreaks and to minimize the number of affected people.
- Strengthened early diagnosis and early treatment, treatment of severe cases to reduce occurrence of severe cases and deaths.
- Further enhanced medical treatment.
- Joint investigation teams between NHFPC and Ministries of Agriculture, Industry and Commerce visited Jiangsu, Zhejiang, Anhui and Guangdong provinces where more cases occurred for joint supervision, inspection and guidance on local surveillance, medical treatment, prevention and control and to promote control measures with a focus on live poultry market management and cross-regional transportation.
- Relevant prefectures in Jiangsu province have closed live poultry markets in late December 2016 and Zhejiang, Guangdong and Anhui provinces have strengthened live poultry market regulations.
- Conducted public risk communication and shared information with the public.
The Centre for Health Protection of the Department of Health in China, Hong Kong SAR has taken the following measures:
- Urged the public to maintain strict personal, food and environmental hygiene both locally and during travel.
- Issued an alert to doctors, hospitals, schools and institutions of the latest situation.
WHO risk assessment
The number of human cases with onset from 1 October 2016 is greater than the total numbers of human cases in earlier waves.
Human infections with the avian influenza A(H7N9) virus remain unusual. Close observation of the epidemiological situation and further characterization of the most recent human viruses are critical to assess associated risk and to adjust risk management measures timely.
Most human cases are exposed to avian influenza A(H7N9) virus through contact with infected poultry or contaminated environments, including live poultry markets. Since the virus continues to be detected in animals and environments, and live poultry vending continues, further human cases can be expected. Although small clusters of human cases with avian influenza A(H7N9) virus have been reported including those involving patients in the same ward, current epidemiological and virological evidence suggests that this virus has not acquired the ability of sustained transmission among humans. Therefore the likelihood of further community level spread is considered low.
Human infection with avian influenza A(H7N9) virus – China
On 10 March 2017, the National Health and Family Planning Commission of China (NHFPC) notified WHO of 26 additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus in mainland China.
Details of the cases
Onset dates ranged from 19 February to 4 March 2017. Of these 26 cases, 8 were female. The median age is 56.5 years (age range among the cases is 15 to 79 years old). The cases were reported from Chongqing (1), Fujian (2), Guangxi (5), Guizhou (2), Henan (4), Hunan (2), Hubei (1), Jiangsu (2), Jiangxi (4) and Sichuan (3).
This is the first case of human infection with avian influenza A(H7N9) reported in Chongqing municipality since H7N9 cases were first reported in 2013.
At the time of notification, there were 3 deaths, and 21 cases were diagnosed as either pneumonia (3) or severe pneumonia (18). The clinical presentations of two (2) cases were not available at time of notification. Twenty-two (22) cases were reported to have had exposure to poultry or live poultry market. Two (2) cases had no exposure to poultry and two (2) cases are still under investigation. No clusters were reported.
To date, a total of 1307 laboratory-confirmed human infections with avian influenza A(H7N9) virus have been reported through IHR notification since early 2013.
Public health response
Considering the increase in the number of human cases since December 2016, the Chinese government at national and local levels is taking further measures including:
- Provincial governments convened meetings; some key provinces have closed live poultry markets.
- The provinces have further strengthened multi-sectoral supervision, inspection and guidance on local surveillance, prevention and control, and are promoting source control measures focused on live poultry market management and cross-regional transportation.
- Training is continued in health care facilities in all places to guide medical treatment of cases.
- Strengthening the technical guidance for prevention and control for some central and western provinces, as cases reported in those provinces increased recently.
- Risk communication and information is provided to the public with guidance on self-protection.
WHO risk assessment
The number of human infections with avian influenza A(H7N9) in the fifth epidemic wave (i.e. onset since 1 October 2016) is greater than the numbers of human cases reported in earlier waves.
.Human infections with the avian influenza A(H7N9) virus remain unusual. Close observation of the epidemiological situation and further characterization of the most recent human viruses are critical to assess associated risk and to adjust risk management measures in a timely manner.
Most human cases are exposed to avian influenza A(H7N9) virus through contact with infected poultry or contaminated environments, including live poultry markets. Since the virus continues to be detected in animals and environments, and live poultry vending continues, further human cases can be expected. Although small clusters of cases of human infection with avian influenza A(H7N9) virus have been reported including those involving patients in the same ward, current epidemiological and virological evidence suggests that this virus has not acquired the ability of sustained transmission among humans. Therefore the likelihood of further community level spread is considered low.
WHO advice
WHO advises that travellers to countries with known outbreaks of avian influenza should avoid, if possible, poultry farms, contact with animals in live poultry markets, entering areas where poultry may be slaughtered, or contact with any surfaces that appear to be contaminated with faeces from poultry or other animals. Travellers should also wash their hands often with soap and water, and follow good food safety and good food hygiene practices.
WHO does not advise special screening at points of entry with regard to this event, nor does it currently recommend any travel or trade restrictions. As always, a diagnosis of infection with an avian influenza virus should be considered in individuals who develop severe acute respiratory symptoms while travelling in or soon after returning from an area where avian influenza is a concern.
WHO encourages countries to continue strengthening influenza surveillance, including surveillance for severe acute respiratory infections (SARI) and influenza-like illness (ILI) and to carefully review any unusual patterns, ensure reporting of human infections under the IHR 2005, and continue national health preparedness actions.
CDC’s PHPR (Office of Public Health Preparedness and Response) In Action
Friday, March 17th, 2017What We Do

An emergency can happen at any moment, and every community in the U.S. must be ready to respond. A pandemic, natural disaster, or chemical or radiological release often strikes without warning. The costs—both economic and human—can be dear.
-

READY FOR EMERGENCIES
In an emergency, you can’t respond effectively if you’re not ready
-

EMERGENCY OPERATIONS
Bringing resources and experts together to respond to emergencies quickly and to scale
-

CRITICAL MEDICINES
AND SUPPLIESMaking sure critical medicines and supplies can get to the right place at the right time
-

LABORATORY RESPONSE
Building capacity to quickly detect, diagnose, and treat those who are impacted by health emergencies
More than 3,300 children were hospitalized in Egypt on Tuesday after an outbreak of food poisoning at several state-run primary schools
Thursday, March 16th, 2017“…..A total of 3,353 children became ill, and at least 50 ambulances were sent to the schools, state news media said. Since then, all but 17 of the students have recovered and been discharged. No deaths or serious complications were reported…..”
4th case of Yellow Fever reported in Europeans who had recently traveled to South America in the past 8 months.
Thursday, March 16th, 2017A travel-associated case of yellow fever has been reported by the Netherlands in March 2017 after travel to Suriname. During the past eight months, four travel-associated cases of yellow fever have been identified among EU travellers returning from South America. This represents a significant increase on four travel-associated cases of yellow fever among EU travellers during the last 27 years (1999 to July 2016).
Brazil has been experiencing a yellow fever outbreak since January 2017 and travel recommendations have been updated accordingly [1,2]. Therefore, EU travellers travelling to areas at risk of yellow fever in South America should be informed of the potential exposure to yellow fever virus and an individual risk benefit analysis should be conducted during pre-travel medical consultation. The ongoing yellow fever outbreak in Brazil should be carefully monitored, as the establishment of an urban cycle of yellow fever would have the potential to rapidly affect a significant number of people. The risk of introduction and further transmission of the yellow fever virus in the EU is currently considered very low.
Advice to travellers EU citizens who travel to, or live in areas where there is evidence of periodic or persistent yellow fever virus transmission, especially those in outbreak-affected regions, are advised to:
• Be aware of the risk of yellow fever in endemic areas throughout South America, including recently affected States in Brazil. WHO publishes a list of countries, territories and areas with yellow fever vaccination requirements and recommendations [1-3].
• Check vaccination status and get vaccinated if necessary. Vaccination against yellow fever is recommended from nine months of age for people visiting or living in yellow fever risk areas. An individual risk benefit analysis should be conducted prior to vaccination, taking into account the period, destination, duration of travel and the likelihood of exposure to mosquitoes (e.g. rural areas, forests) as well as individual risk factors for adverse events following yellow fever vaccination.
• Take measures to prevent mosquito bites indoors and outdoors, especially between sunrise and sunset when Aedes and sylvatic yellow fever mosquito vectors are most active [4]. These measures include: − the use of mosquito repellent in accordance with the instructions indicated on the product label; − wearing long-sleeved shirts and long trousers; − sleeping or resting in screened/air-conditioned rooms, or using mosquito nets at night and during the day.
Advice to health professionals: Physicians, health professionals and travel health clinics should be provided with or have access to regularly updated information about areas with ongoing yellow fever transmission and should consider yellow fever in the differential diagnoses for illnesses in relation to travellers returning from affected areas. To reduce the risk of adverse events following immunisation, healthcare practitioners should be aware of contraindications and comply with the manufacturers’ precautionary advice before administering yellow fever vaccine [5].

Moving targets: A Pakistani vaccination strategy as agile and stubborn as the polio virus itself.
Thursday, March 16th, 2017“….makeshift vaccination clinics set up at bus stops, border crossings, army posts, and police checkpoints across the country in an effort to reach children who are on the move…..
At hundreds of sites, teams of health workers verify that every child passing through receives the vaccine.
Another child, another family, another generation is protected, and Pakistan moves one step closer to having zero polio cases…..”

Egypt’s Health Ministry says 2 262 schoolchildren have been admitted to hospital in a suspected mass food poisoning this week from 8 schools in the southern province of Sohag
Thursday, March 16th, 2017“….most of those admitted to hospital have been released. Samples of the meals were being analyzed to ascertain the cause of the suspected poisoning………[T]he Sohag governor suspended the food program pending the outcome of the analysis…..”
Lithuania: An emergency has been declared in the capital city of Vilnius after Legionella bacteria were found in the water systems of several apartment buildings.
Wednesday, March 15th, 2017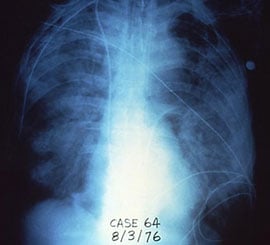
Legionellosis is bacterial respiratory disease caused by Legionella that can present as either Legionnaires’ disease or Pontiac fever. Legionnaires’ disease is a common cause of severe pneumonia requiring hospitalization, while Pontiac fever generally resolves on its own.
The following table summarizes key clinical differences between Legionnaires’ disease and Pontiac fever.
| Legionnaires’ disease | ||
|---|---|---|
| Clinical features | Pneumonia, cough, fever | |
| Pathogenesis | Replication of organism | |
| Radiographic pneumonia | Yes | |
| Incubation period | 2 to 10* days after exposure | |
| Percent of persons who become ill, when exposed to the source of an outbreak |
Less than 5% | |
| Isolation of organism | Possible | |
| Outcome | Hospitalization common Case-fatality rate: 10%, approximately 30% for healthcare-associated cases |
John Snow, known as the father of epidemiology, was born on March 15, 1813.
Wednesday, March 15th, 2017
John Snow, known as the father of epidemiology, was born on March 15, 1813. This week, we honor the birthday of the first true disease detective.
The Story of the Broad Street Pump
London, 1854: A cramped Soho neighborhood teems with people and animals living in cramped and dirty quarters. A deadly outbreak of cholera is spreading. Doctors and scientists believe it’s caused by “miasma,” or bad air. They theorize that particles from rotting matter and waste are getting into the air and making people sick.
Enter John Snow. An accomplished physician, he becomes convinced that something other than the air might be responsible for the illness. Through carefully mapping the outbreak, he finds that everyone affected has a single connection in common: they have all retrieved water from the local Broad Street pump.
On September 8, 1854, Snow tests his theory by removing the pump’s handle, effectively stopping the outbreak, proving his theory, and opening the door to modern epidemiology.
Valuable Lessons for a Modern Age
In 1854, John Snow was the first to use maps and records to track the spread of a disease back to its source. Today, his ideas provide the foundation for how we find and stop disease all over the world.
We have better, more modern tools now for identifying and tracking illness, like access to state-of-the-art labs and computer systems. We have in-depth knowledge of germs and how they spread. But when we train today’s disease detectives, we still return to the basics. CDC disease detectives are trained to look for clues by asking:
- WHO is sick?
- WHAT are their symptoms?
- WHEN did they get sick?
- WHERE could they have been exposed to the cause of the illness?
We live in a world where disease can travel across the globe in a matter of hours. This means we must not only apply these basic lessons of epidemiology, but we must constantly be looking for ways to find better answers, faster.
Disease Detectives Make a Difference
When outbreaks or other threats emerge, CDC’s disease detectives, some of whom are trained through our Epidemic Intelligence Service (EIS), are on the scene. These boots-on-the ground staff, called EIS officers, support over 100 public health investigations (Epi-Aids) each year in the U.S. and worldwide.
CDC’s disease detectives have been instrumental in tracking down threats like:
Anthrax: During the 2001 anthrax outbreak among U.S. postal workers, disease detectives investigated the route of contaminated envelopes and how workers became infected.
E. coli: For the first time, disease detectives conclusively showed that flour was the source of a 2016 E. coli outbreak. Millions of pounds of flour were taken off the shelves, including flour-containing products like bread, cake, and muffin mixes.
Seoul virus: Disease detectives have been working to track and stop an outbreak of Seoul virus, an emerging rodent-borne hantavirus, involving home-based rat breeders this year. The outbreak was first identified after two Wisconsin rat breeders became ill in December and, as of March 13, the investigation has so far included rat-breeding facilities in 15 states, with 17 people infected in seven states.
Like Snow’s map that revealed cases of cholera congregated around the Broad Street pump, we must keep tabs on where and how disease is spreading. Once the source of disease is identified, it is crucial to develop and implement interventions to help prevent people from getting sick. We must remain innovative and creative, like Snow when he removed the handle of the Broad Street pump to stop disease at the source.
References
- MMWR: 150th Anniversary of John Snow and the Pump Handle
- CDC: Epidemic Intelligence Service (EIS)
- CDC: Epidemic Intelligence Service Conference
- Public Library of Science: John Snow – The First Epidemiologist
- TED Talk: How the “ghost map” helped end a killer disease