Archive for April, 2017
World Health Worker Week: April 2-8, 2017
Sunday, April 2nd, 2017World Health Worker Week is an opportunity to mobilize communities, partners, and policy makers in support of health workers in your community and around the world. It is a time to celebrate the amazing work that they do and it is a time to raise awareness to the challenges they face every day. Perhaps most importantly, it is an opportunity to fill in the gaps in the health workforce by calling those in power to ensure that health workers have the training, supplies and support they need to do their jobs effectively.
They are caretakers. They are educators. They are your neighbors, friends, and family. Without them, there would be no health care for millions of families in the developing world.
Frontline health workers are midwives, community health workers, pharmacists, peer counselors, nurses and doctors working at community level as the first point of care for communities. They are the backbone of effective health systems and often come from the very communities they serve.
They are the first and often the only link to health care for millions of people. Frontline health workers provide immunizations and treat common infections. They are on the frontlines of battling deadly diseases diseases like Ebola and HIV/AIDS, and many families rely on them as trusted sources of information for preventing, treating and managing a variety of leading killers including diarrhea, pneumonia, malaria and tuberculosis.
Honor health workers in your community (or communities you work in) by sharing their story. Participate in our ‘#HealthWorkersCount because…’ campaign. Download our template or make your own, but share your reasons using the hashtags #WHWWeek and #HealthWorkersCount. You can also use these hashtags to participate in our WHWW Twitter Chat on April 4 at 1pm EDT.
Organize events, local advocacy campaigns and other activities calling global leaders to prioritize health workforce strengthening.
Download our World Health Worker Week Toolkit for Engagement for more ideas!
World Health Worker Week is only seven days, but here is how you can take action and make a difference year round:
Follow us on Twitter and Facebook to get updates of our activities, news and ways to get involved.
The Global Health Workforce Network operates within WHO as a global mechanism for stakeholder consultation, dialogue and coordination on comprehensive and coherent health workforce policies in support of the implementation of the Global Strategy on Human Resources for Health: Workforce 2030 and the recommendations of the High-Level Commission on Health Employment and Economic Growth.
Let your member of Congress know how important frontline health workers are to saving lives and increasing security from global health threats worldwide. Refer to our brief on the Global Health Council’s ‘Global Health Works’ Report for basic facts and recommendations to highlight your message.
Advocacy organizations like the ONE Campaign and RESULTS provide direct actions you can take to raise awareness and urge your policymakers to support US global health efforts. Get involved today and spread the word that #HealthWorkersCount.
Eighteen people were hurt, five of them seriously, when a bonfire effigy blew up at a carnival north of Paris on Saturday.
Sunday, April 2nd, 2017https://www.youtube.com/watch?v=YVaEYnNI_3M
Flooding and mudslides in the Colombian city of Mocoa sent torrents of water and debris crashing onto houses in the early hours of Saturday morning, killing 254 people and injuring hundreds
Sunday, April 2nd, 2017Flu week 12 (March 19-25, 2017) in the United States.
Saturday, April 1st, 2017Synopsis:
During week 12 (March 19-25, 2017), influenza activity remained elevated in the United States.
- Viral Surveillance: The most frequently identified influenza virus subtype reported by public health laboratories during week 12 was influenza A (H3). The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased slightly.
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was above the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Six influenza-associated pediatric deaths were reported.
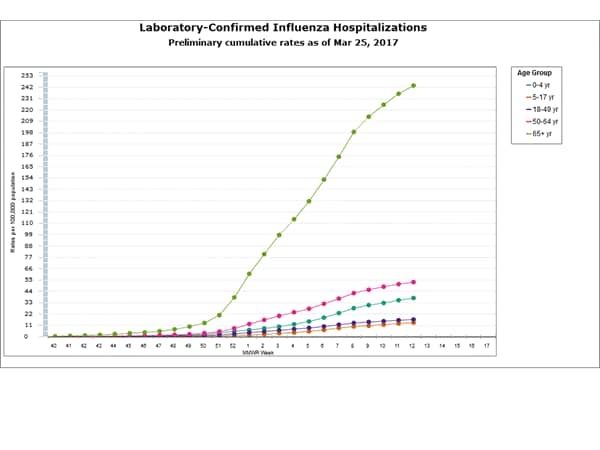
- Influenza-associated Hospitalizations: A cumulative rate for the season of 54.1 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
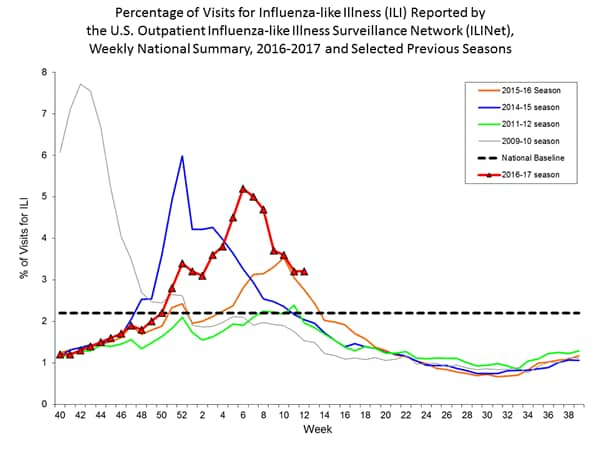
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 3.2%, which is above the national baseline of 2.2%. Eight of ten regions reported ILI at or above their region-specific baseline levels. 10 states experienced high ILI activity; eight states experienced moderate ILI activity; eight states experienced low ILI activity; New York City, Puerto Rico, and 24 states experienced minimal ILI activity; and the District of Columbia had insufficient data.
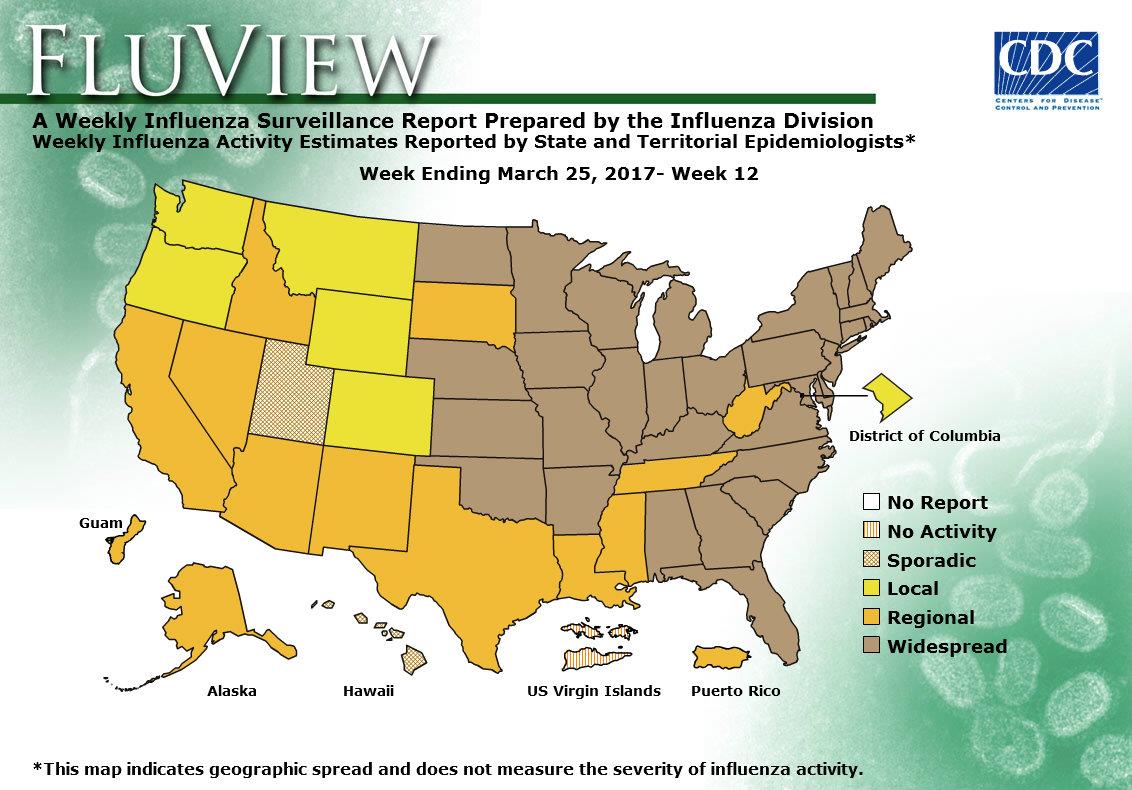
- Geographic Spread of Influenza: The geographic spread of influenza in 31 states was reported as widespread; Guam, Puerto Rico and 12 states reported regional activity; the District of Columbia and five states reported local activity; two states reported sporadic activity; and the U.S. Virgin Islands reported no activity.
How healthcare suffered when ISIL seized Mosul, Iraq
Saturday, April 1st, 2017CITY PROFILE OF MOSUL, IRAQ
Multi-sector assessment of a city under siege
United Nations Human Settlements Programme in Iraq (UN-Habitat) 2016
www.unhabitat.org
Nineveh Governorate was once known for its good
healthcare services and highly-qualified doctors.
Between 2008 and 2014, a substantial number of facilities
were rehabilitated and equipped with new medical
instruments. New specialized hospitals were also planned
in the northern and southern parts of the city, and some
were still under construction when ISIL took over the city
(Map 23).
According to the Ministry of Planning (2013), Mosul city
has in total:
• 13 public hospitals with a 3,200-bed capacity;
• 4 specialized public hospitals (gynaecology, cancer
and nuclear medicine, paediatric and maternity, and
chest diseases and fevers) with a 228-bed capacity;
• 3 private hospitals with a 104-bed capacity;
• 32 public health clinics; and
• 254 private health clinics.

All these facilities were managed by specialist doctors
and were working properly until ISIL occupied the city.
At that point, although hospitals were not destroyed by
air strikes and continue to receive civilian patients, health
services started to deteriorate. Due to the fragile security
situation, many medical staff members fled. This clearly
affected the quality of healthcare and the capacity of
hospitals to deal with surgical cases, and with patients
in general. With regard to surgeries, priority was given
to non-civilians patients. Also, the higher fees that ISIL
imposed on medical services and operations (IQD 100,000
– IQD 500,000) added to the suffering of many civilians.
The fact that ISIL prohibited male doctors from examining
female patients, and female doctors from examining
male patients, has particularly affected maternal health.
Exacerbating the problem is the increasingly poor
sanitation in hospitals and the disposal of hazardous
waste. The lack of obstetric and natal care is another
serious issue especially in view of the depletion of
vaccinations for infants. The availability of other medical supplies and equipment has also decreased, as stocks
were transferred outside Mosul and/or diverted for other
uses by ISIL.
The closure of the highways that connect Mosul with
other Iraqi cities further contributed to the decline of
the city’s health sector. Although many pharmacies are
still open, their stocks is quite limited. Medicines, when
available, are largely unaffordable. According to some city
residents, the only available medicines in Mosul today
are illegally imported from Syria and Turkey through ISIL
followers.
In short, many city inhabitants are affected by poor
healthcare, difficult access to surgery, unavailability of
basic medicines and medical supplies (e.g. insulin and
medicines for high blood pressure), as well as poor solid
waste disposal and limited clean water for drinking.