Archive for May, 2017
Compounds containing copper and other metal salts were tested in mice, which like humans are vulnerable to the toxin’s blockage of nerve signals to muscles. They penetrated to the site of the neurotoxin’s action, extending the lives of the mice that were given lethal doses.
Monday, May 29th, 2017Metal Ions Effectively Ablate the Action of Botulinum Neurotoxin A
Abstract: “Botulinum neurotoxin serotype A (BoNT/A) causes a debilitating and potentially fatal illness known as botulism. The toxin is also a known bioterror threat, yet no pharmacological antagonists to counteract its effects has reached clinical approval. Existing strategies to negate BoNT/A intoxication have looked to antibodies, peptides or organic small molecules as potential therapeutics. In this work, a departure from the traditional drug discovery mindset was pursued, in which the enzyme’s susceptibility to metal ions was exploited. A screen of a series of metal salts showed marked inhibitory activity of group 11 and 12 metals against the BoNT/A light chain (LC) protease. Enzyme kinetics revealed that copper (I) and (II) cations displayed noncompetitive inhibition of the LC (Ki ≈ 1 µM), while mercury (II) cations were 10-fold more potent. Crystallographic and mutagenesis studies elucidated a key binding interaction between Cys165 on BoNT/A LC and the inhibitory metals. As potential copper prodrugs, ligand-copper complexes were examined in a cell-based model and were found to prevent BoNT/A cleavage of the endogenous protein substrate, SNAP-25, even at low µM concentrations of complexes. Further investigation of the complexes suggested a bioreductive mechanism causing intracellular release of copper, which directly inhibited the BoNT/A protease. In vivo experiments demonstrated that dithiocarbamate and bis(thiosemicarbazone) copper (II) complexes could delay BoNT/A-mediated lethality in a rodent model, indicating their potential for treating the harmful effects of BoNT/A intoxication. Our studies illustrate that metals can be therapeutically viable enzyme inhibitors; moreover, enzymes that share homology with BoNT LCs may be similarly targeted with metals.”
Asymptomatic Ebola: A Rare Event
Monday, May 29th, 2017Glynn JR, Bower H, Johnson S, et al. Asymptomatic infection and unrecognized Ebola virus disease in Ebola-affected households in Sierra Leone: a cross-sectional study using a new non-invasive assay for antibodies to Ebola virus. Lancet Infect Dis 2017;17:645-653.
“…..By using control subjects, Glynn and colleagues incorporated appropriate rigor into their low overall estimate of 2.6% asymptomatic infection. If asymptomatic infection is a rare event, as this study suggests, then outbreak control should be focused on identifying symptomatic individuals and initiating the appropriate infection control measures to halt an outbreak.
Japan has disaster theme parks: Visitors can ride earthquake simulators, experience a mock-typhoon and use fire extinguishers.
Sunday, May 28th, 2017“…..Guided by the philosophy that experience is the best teacher, Japan wants its citizens to know what it will feel like when the ground under their feet starts to heave — and how to protect themselves. So cities across the country have constructed disaster education centers that combine theme-park-style simulations with sober lessons in survival.
Many of the more than 60 centers feature large shake tables where visitors can ride out fake quakes as powerful as the real thing. In some centers, visitors navigate life-size dioramas of crushed cars and teetering power poles while being quizzed on the best response to dangerous situations. Typhoons, floods and fires get hands-on treatment as well…..”

Qatar: A new MERS-CoV case has been confirmed for a 29 years old camel worker
Sunday, May 28th, 2017Ministry of Public Health (MOPH) has announced that a new Middle East Respiratory Syndrome Corona Virus (MERS-CoV) case has been confirmed for a 29 years old, resident in Qatar, marking the third MERS-CoV case to be confirmed in the country this year and bringing the cumulative number of confirmed MERS-CoV cases since 2012 to 21 cases among whom 7 have died.

The patient is a camel worker and had complaints of fever and dry cough for several days. He sought a medical attention in Hamad General Hospital where an X-Ray investigation suggested a severe pneumonia. Consequently and as he reported an occupational frequent contact with camels, further samples were withdrawn from the patient. He ultimately tested positive for MERS-CoV according to Hamad Medical Corporation laboratories.
Despite his stable condition, the patient was admitted to hospital, in consistence with the national infection prevention and control protocol for confirmed and suspected MERS-CoV cases to ensure the appropriate medical attention. However, neither a history of contact with similar cases nor a recent travel outside the country was reported for the patient who has no comorbidities.
Once the case has been confirmed, the rapid response team of the Health Protection and Communicable disease Control (HP & CDC) department at the MOPH, accompanied with the team from Animal Health Department, Ministry of Municipality and Environment, have started a field investigation to assess the possible source of the infection and to verify whether any of the patient contacts has suspected symptoms according to the WHO standard case definition. Consequently, all traced contacts will be monitored over a period of two weeks, while those who develop suspected symptoms will then be subjected to confirmatory laboratory investigation.
The Ministry of Public Health advices citizens and residents, in particular those with comorbidities or low immunity, to abide to cough etiquette and handwashing with soap and water thoroughly and avoid unnecessary contact with sick animals.
MOPH proclaimed that Health Protection &CDC Hotlines 66740948 & 66740951 are accessible 24/7 to respond to any notification or enquiry related to infectious diseases.
For the first time in its seventy-year history, the World Health Organization (WHO) will, effective July 1, be led by a nonphysician, an African, and a person from the global South: Tedros Adhanom Ghebreyesus of Ethiopia
Sunday, May 28th, 2017“……Tedros has a PhD in community health and has served as his nation’s minister of health and of foreign affairs, as well as a central committee member of the ruling Ethiopian People’s Revolutionary Democratic Front party.
Despite Ethiopia’s dismal human rights record, when campaigning for the position started in 2016, U.S. President Barack Obama’s administration backed Tedros, admiring his track record as minister of health. He is credited with leading a dramatic re-envisioning of health, in which forty thousand community health workers were trained to provide basic services at the village level and hundreds of clinics were built across the large, diverse nation. These steps resulted in sharp reductions in the rates of infectious diseases like malaria and HIV, and a decrease in the number of women dying during childbirth. The United States also appreciated Tedros’s transformative role as chair of the Global Fund to Fight AIDS, Tuberculosis and Malaria, bringing reform to an institution that had been fraught with fraud and “missing money.”….”

First time: Zika virus infection – India
Sunday, May 28th, 2017On 15 May 2017, the Ministry of Health and Family Welfare-Government of India (MoHFW) reported three laboratory-confirmed cases of Zika virus disease in Bapunagar area, Ahmedabad District, Gujarat, State, India.
The routine laboratory surveillance detected a laboratory-confirmed case of Zika virus disease through RT-PCR test at B.J. Medical College, Ahmedabad, Gujarat. The etiology of this case has been further confirmed through a positive RT-PCR test and sequencing at the national reference laboratory, National Institute of Virology (NIV), Pune on 4 January 2017 (case 2, below). Two additional cases (case 1 and case 3), have then been identified through the Acute Febrile Illness (AFI) and the Antenatal clinic (ANC) surveillance. The cases are reported below in chronological order:
- Case 1: During the Acute Febrile Illness (AFI) surveillance between 10 to 16 February 2016, a total of 93 blood samples were collected at BJ Medical College (BJMC), Ahmedabad, Gujarat State. One sample from a 64-year-old male presenting with febrile illness of 8 days’ duration (negative for dengue infection) was found to be positive for Zika virus at BJMC, Ahmedabad. This is the first Zika positive case reported through AFI surveillance at BJMC, Ahmedabad, Gujarat State.
- Case 2: A 34-year-old female, delivered a clinically well baby at BJMC in Ahmedabad on 9 November 2016. During her hospital stay, she developed a low grade fever after delivery. No history of fever during pregnancy and no history of travel for the past three months was reported. A sample from the patient was referred to the Viral Research & Diagnostic Laboratory (VRDL) at the BJMC for dengue testing and thereafter found to be positive for Zika virus. She was discharged after one week (on 16 November 2016). The sample was re-confirmed as Zika virus positive by RT-PCR and sequencing at NIV, Pune.
- Case 3: During the Antenatal clinic (ANC) surveillance between 6 and 12 January 2017, a total of 111 blood samples were collected at BJMC. One sample from a 22-year-old pregnant female in her 37th week of pregnancy has been tested positive for Zika virus disease.
Public health response
- National Guidelines and Action Plan on Zika virus disease have been shared with the States to prevent an outbreak of Zika virus disease and containment of spread in case of any outbreak.
- An Inter-Ministerial Task Force has been set up under the Chairmanship of Secretary (Health and Family Welfare) together with Secretary (Bio-Technology), and Secretary (Department of Health Research). The Joint Monitoring Group, a technical group tasked to monitor emerging and re-emerging diseases is regularly reviewing the global situation on Zika virus disease.
- All the international airports and ports have displayed information for travellers on Zika virus disease.
- The airport health officers along with airport organizations, National Centre for Disease Control, and the National Vector Borne Disease Control Programme are monitoring appropriate vector control measures in airport premises.
- The Integrated Disease Surveillance Programme (IDSP) is tracking for clustering of acute febrile illness in the community.
- In addition to National Institute of Virology, Pune, and NCDC in Delhi, 25 laboratories have also been strengthened by Indian Council of Medical Research for laboratory diagnosis. In addition, 3 entomological laboratories are conducting Zika virus testing on mosquito samples.
- The Indian Council of Medical Research (ICMR) has tested 34 233 human samples and 12 647 mosquito samples for the presence of Zika virus. Among those, close to 500 mosquitos samples were collected from Bapunagar area, Ahmedabad District, in Gujarat, and were found negative for Zika.
- The Rashtriya Bal Swasthya Karyakram (RBSK) is monitoring microcephaly from 55 sentinel sites. As of now, no increase in number of cases or clustering of microcephaly has been reported from these centers.
- Risk communication materials are being finalized by the Central Health Education Bureau, in consultation with UNICEF.
WHO risk assessment
This report is important as it describes the first cases of Zika virus infections and provides evidence on the circulation of the virus in India. These findings suggest low level transmission of Zika virus and new cases may occur in the future. Efforts to strengthen surveillance should be maintained in order to better characterize the intensity of the viral circulation and geographical spread, and monitor Zika virus related complications. Zika virus is known to be circulating in South East Asia Region and these findings do not change the global risk assessment. WHO encourages Member states to report similar findings to better understand the global epidemiology of Zika virus.
The risk of further spread of Zika virus to areas where the competent vectors, the Aedes mosquitoes, are present is significant given the wide geographical distribution of these mosquitoes in various regions of the world. WHO continues to monitor the epidemiological situation and conduct risk assessment based on the latest available information.
WHO advice
Prevention and control relies on reducing mosquitoes through source reduction (removal and modification of breeding sites) and reducing contact between mosquitoes and people. During outbreaks, health authorities may advise that spraying of insecticides be carried out. Insecticides recommended by the WHO Pesticide Evaluation Scheme may also be used as larvicides to treat relatively large water containers.
Basic precautions for protection from mosquito bites should be taken by people traveling to high risk areas, especially pregnant women. These include use of repellents, wearing light colored, long sleeved shirts and pants and ensuring rooms are fitted with screens to prevent mosquitoes from entering.
WHO does not recommend any travel or trade restriction to India based on the current information available.
Health experts say the international community has turned a blind eye to widespread food insecurity in Haiti, where communities across nearly every region of the island are approaching risk of famine.
Sunday, May 28th, 2017“…..In March, a report from the U.N.’s Office for the Coordination of Humanitarian Affairs (OCHA) estimated that of the 2.1 million Haitians affected by the hurricane last October, 1.4 million still don’t have enough food or safe drinking water.
More recently, statistics from the European Commission indicated that eight out of Haiti’s 10 departments have reached “crisis” levels of food insecurity…..”

The humanitarian context in Haiti remains challenging as the country continue to be affected by a convergence of humanitarian crises further aggravated by Hurricane Matthew and which has severely impacted the pre-existing humanitarian situation. Despite immediate humanitarian response provided so far, post Hurricane Matthew’s humanitarian needs are still high with an estimated 1.4 million people in need of humanitarian assistance. Additionally, 1.5 million vulnerable Haitians are currently food insecure and 280 K highly food insecure and in need of urgent food assistance. Cholera and the bi-national crisis continue also to be humanitarian threats to the country with respectively 1,856 cholera cases reported in January 2017 and 175,578 returnees registered from the Dominican Republic as of 2 March 2017.
UN Office for the Coordination of Humanitarian Affairs:
To learn more about OCHA’s activities, please visit http://unocha.org/.

California: About 7 percent of the state’s hospital buildings — 220 — are still designated as having the highest risk of collapse following an earthquake.
Saturday, May 27th, 2017“…..These high-risk buildings must be retrofitted or rebuilt to meet certain safety standards by 2020 — the first of two deadlines….”

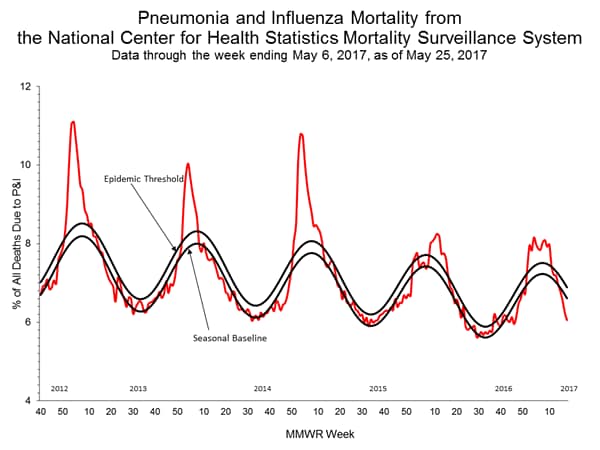
CDC: Week 20 (May 14-20, 2017), influenza activity decreased in the United States.
Saturday, May 27th, 2017During week 20 (May 14-20, 2017), influenza activity decreased in the United States.
- Viral Surveillance: The most frequently identified influenza virus type reported by public health laboratories during week 20 was influenza B. The percentage of respiratory specimens testing positive for influenza in clinical laboratories decreased.
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Three influenza-associated pediatric deaths were reported.
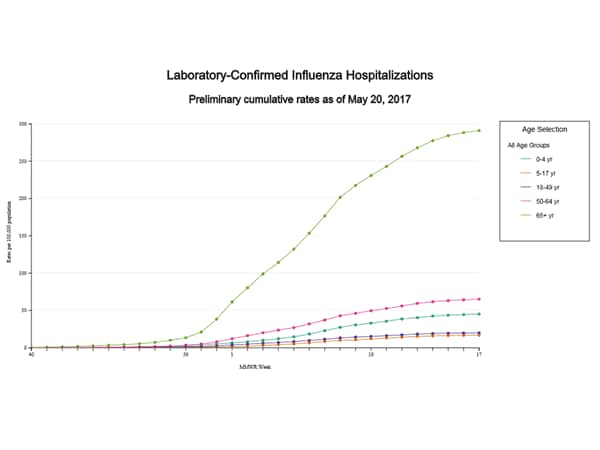
- Influenza-associated Hospitalizations: A cumulative rate for the season of 65.2 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
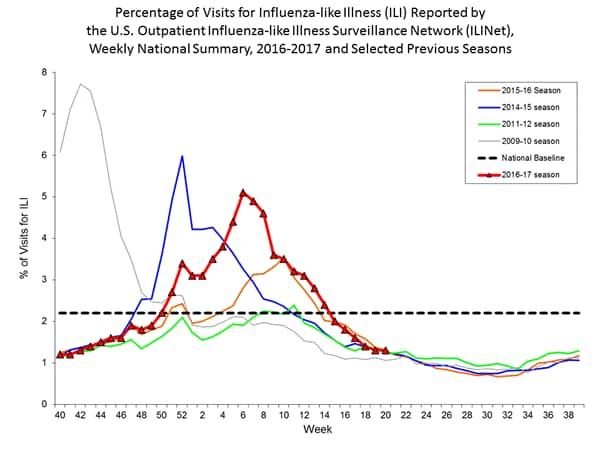
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 1.3%, which is below the national baseline of 2.2%. All ten regions reported ILI below their region-specific baseline levels. One state experienced low ILI activity; New York City, Puerto Rico, and 49 states experienced minimal ILI activity; and the District of Columbia had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in Guam and two states was reported as regional; Puerto Rico and nine states reported local activity; the District of Columbia and 34 states reported sporadic activity; and the U.S. Virgin Islands and five states reported no activity.