Archive for June, 2017
The London Inferno: At least 12 killed so far…..
Wednesday, June 14th, 2017“…..A blaze engulfed a 24-story housing block in central London on Wednesday, trapping residents as they slept and killing at least 12 people in an inferno that the fire brigade said was unprecedented in its scale and speed.
More than 200 firefighters, backed up by 40 fire engines, fought for hours to try to control the blaze, London’s deadliest for a generation. The Grenfell Tower apartment block was home to about 600 people…..”
The Ministry of Public Health and Population of Yemen has recorded an additional 13 912 cholera cases in Yemen between 3 and 6 June 2017.
Wednesday, June 14th, 2017Dysphagia resulting from congenital Zika virus syndrome microcephaly can develop in infants >3 months of age and is severe.
Wednesday, June 14th, 2017Leal MC, van der Linden V, Bezerra TP, de Valois L, Borges ACG, Antunes MMC, et al. Characteristics of dysphagia in infants with microcephaly caused by congenital Zika virus infection, Brazil, 2015. Emerg Infect Dis. 2017 Aug [date cited]. https://doi.org/10.3201/eid2308.170354
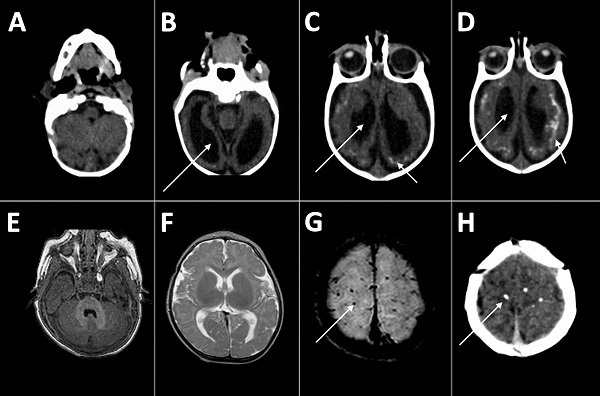
Computed tomography radiographs of the brains of 2 infants with dysphagia and microcephaly caused by congenital Zika virus infection, Brazil, 2015. A–D) Images for patient 4 show malformation of cortical development, ventriculomegaly (long arrows), and calcifications in cortical and subcortical white matter in transition between cortex and white matter (short arrows). E–H) Images for patient 6 show no malformation of cortical development or ventriculomegaly, but calcifications are visible in the cortical area (arrows).
Circulating vaccine-derived poliovirus type 2 – Democratic Republic of the Congo
Wednesday, June 14th, 2017In the Democratic Republic of the Congo (DRC), two separate circulating vaccine-derived poliovirus type 2s (cVDPV2s) have been confirmed. The first cVDPV2 strain has been isolated from two acute flaccid paralysis (AFP) cases from two districts in Haut-Lomami province, with onset of paralysis on 20 February and 8 March 2017. The second cVDPV2 strain has been isolated from Maniema province, from two AFP cases (with onset of paralysis on 18 April and 8 May 2017) and a healthy contact in the community.
Public health response
The Ministry of Health, supported by WHO and partners of the Global Polio Eradication Initiative (GPEI), has completed a risk assessment, including evaluating population immunity and the risk of further spread.
Outbreak response plans are currently being finalized, consisting of strengthening surveillance, including active case searching for additional cases of AFP, and supplementary immunization activities (SIAs) with monovalent oral polio vaccine type 2 (mOPV2), in line with internationally-agreed outbreak response protocols.
Surveillance and immunization activities are being strengthened in neighbouring countries.
WHO risk assessment
WHO assesses the risk of further national spread of these strains to be high, and the risk of international spread to be medium.
The detection of cVDPV2s underscores the importance of maintaining high routine vaccination coverage everywhere, to minimize the risk and consequences of any poliovirus circulation. These events also underscore the risk posed by any low-level transmission of the virus. A robust outbreak response as initiated is needed to rapidly stop circulation and ensure sufficient vaccination coverage in the affected areas to prevent similar outbreaks in the future. WHO will continue to evaluate the epidemiological situation and outbreak response measures being implemented.
WHO advice
It is important that all countries, in particular those with frequent travel and contacts with polio-affected countries and areas, strengthen surveillance for AFP cases in order to rapidly detect any new virus importation and to facilitate a rapid response. Countries, territories and areas should also maintain uniformly high routine immunization coverage at the district level to minimize the consequences of any new virus introduction.
WHO’s International Travel and Health recommends that all travellers to polio-affected areas be fully vaccinated against polio. Residents (and visitors for more than four weeks) from infected areas should receive an additional dose of OPV or inactivated polio vaccine (IPV) within four weeks to 12 months of travel. As per the advice of the Emergency Committee convened under the International Health Regulations (2005), efforts to limit the international spread of poliovirus remains a Public Health Emergency of International Concern (PHEIC). Countries affected by poliovirus transmission are subject to Temporary Recommendations. To comply with the Temporary Recommendations issued under the PHEIC, any country infected by poliovirus should declare the outbreak as a national public health emergency and consider vaccination of all international travellers.
Circulating vaccine-derived poliovirus type 2 – Syrian Arab Republic
Wednesday, June 14th, 2017A circulating vaccine-derived poliovirus type 2 (cVDPV2) outbreak has been confirmed in the Deir Al Zour Governorate of the Syrian Arab Republic. There is evidence of genetic linkage among three isolates of type-2 vaccine-derived polioviruses (VDPV2) isolated in the stool specimens of two acute flaccid paralysis (AFP) cases with dates of onset of paralysis on 5 March and 6 May 2017, and the contact specimen of an AFP case collected on 17 April 2017. Al Mayadeen was also the epi-centre of the wild poliovirus type 1 (WPV1) outbreak in Syrian Arab Republic in 2013. Aggressive multi-country polio outbreak response effectively controlled the WPV1 outbreak and no WPV1 case has been reported in Syrian Arab Republic since 21 January 2014.
Public health response
Since the confirmation of the first VDPV2 during May 2017, AFP surveillance has been intensified in the Governorate, especially in the Al Mayadeen district. As of 6 June 2017, a total of 58 AFP cases have been reported from the Governorate this year. In addition to the two cases that have tested positive for VDPV2, a further 11 have tested negative for polioviruses, with the remaining samples being under process in the laboratories or being transported to the laboratories.
Subsequent to the confirmation of the cVDPV2 outbreak, outbreak response planning is underway, including planning for supplementary immunization activities (SIAs) with monovalent oral polio vaccine type 2 (mOPV2), in line with internationally-agreed outbreak response protocols.
Although access for vaccination is compromised due to prevailing insecurity in Deir Al Zour, the Governorate has been partially reached by several vaccination campaigns against polio and other vaccine-preventable diseases since the beginning of 2016. Most recently, two campaigns have been conducted in March and April 2017 using bivalent oral polio vaccine (bOPV). The most recent full trivalent oral polio vaccine (tOPV) round was conducted in October 2015; while tOPV rounds conducted in the first four months of 2016 only reached part of the target population of the Deir Al Zour Governorate. It is pertinent to mention that Syrian Arab Republic introduced two doses of inactivated polio vaccine (IPV) in the routine infant immunization schedule in 2008. Syrian Arab Republic switched from tOPV to bOPV for routine immunization on 1 May 2016.
A detailed risk analysis is currently being updated, including assessing overall population immunity levels and strengthening active searches for additional cases of AFP. Surveillance and immunization activities are being strengthened in neighbouring countries as well.
WHO risk assessment
The detection of cVDPV2 underscores the importance of maintaining high levels of routine vaccination coverage at all levels to minimize the risk and consequences of any poliovirus circulation. Such events also underscore the risk in areas or regions with continued substantial insecurity that hampers maintaining high population immunity through routine vaccination. A robust outbreak response is needed to rapidly stop the VDPV2 transmission. WHO will continue to evaluate the epidemiological situation and outbreak response measures being implemented.
WHO advice
It is important to complete the ongoing risk assessment as soon as possible to inform the vaccination response with mOPV2 and IPV. The geographical scale of the vaccination response will be in accordance with the findings of the risk assessment. It will be critical to achieve the highest possible coverage during the vaccination response. Given the difficult and challenging security situation in the area, appropriate strategies will be identified and utilized to implement the response. Intensified AFP surveillance should continue.
It is important that all countries, in particular those with frequent travel and contacts with polio-affected countries and areas, strengthen surveillance for AFP cases in order to rapidly detect any new virus importation and to facilitate a rapid response. Countries, territories, and areas should also maintain uniformly high routine immunization coverage at the district level to minimize the consequences of any new virus introduction.
WHO’s International Travel and Health recommends that all travellers to polio-affected areas be fully vaccinated against polio. Residents (and visitors for more than four weeks) from infected areas should receive an additional dose of OPV or IPV within four weeks to 12 months prior to the travel.
As per the advice of an Emergency Committee convened under the International Health Regulations (2005), efforts to limit the international spread of poliovirus remains a Public Health Emergency of International Concern (PHEIC). Countries affected by poliovirus transmission are subject to Temporary Recommendations. To comply with the Temporary Recommendations issued under the PHEIC, any country infected by poliovirus should declare the outbreak as a national public health emergency and consider vaccination of all international travellers.
WHO: Between 1 and 10 June 2017, the national IHR focal point of Saudi Arabia reported 35 additional cases of MERS-CoV
Wednesday, June 14th, 2017Between 1 and 10 June 2017, the national IHR focal point of Saudi Arabia reported 35 additional cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection including three fatal cases and one death among previously reported cases (case number 5 in the Disease Outbreak News published on 6 June 2017).
Details of the cases
Detailed information concerning the cases reported can be found in a separate document (see link below).
Thirty-two of the 35 newly reported cases are associated with three simultaneous clusters of MERS, of which two are related. A description of the three clusters is below.
Cluster 1
A cluster of MERS has been identified in a hospital in Riyadh city, Riyadh Region. Twenty three cases associated with this cluster thus far and include the first identified case (a 47-year-old male reported on 1 June), 14 asymptomatic health care worker contacts, one household contact, and seven hospital contacts who were patients.
Cluster 2
This MERS cluster is occurring in a second hospital in Riyadh City, Riyadh Region. This cluster is related to cluster 1 above. The first identified case of this second cluster visited the emergency room of the cluster 1 hospital. He was asymptomatic and following this visit in hospital 1, he continued to receive kidney dialysis sessions in the second hospital. To date, this cluster involves six cases, including the case involved in cluster 1, and secondary household and health care worker contacts.
Cluster 3
This MERS cluster is currently occurring in a third hospital in Riyadh city, Riyadh Region. To date the cluster involves the four cases including the first identified case who reported contacts with dromedary camels and three asymptomatic or mild cases who were health care worker contacts.
Public health response
The Ministry of Health of Saudi Arabia is evaluating each case and their contacts and implementing measures to limit further human-to-human transmission and bring these outbreaks to a control. These measures include:
- Proper isolation for all confirmed cases;
- Active tracing for all contacts of patients, healthcare workers and community contacts;
- Identification of high and low risk contacts with daily monitoring for all during incubation period of the 14 days and performing laboratory testing for high risk contacts, regardless of the development of symptoms;
- Regular updating of the line list of cases and contacts and conducting epidemiological analysis of data to identify the source of infection, links between patients and reasons for human-to-human transmission within hospitals;
- Searching for suspected cases between patients and healthcare workers based on case definition of the disease;
- Enforcement of strict adherence to proper environmental cleaning, disinfection and terminal cleaning and disinfection for hospital environment with special care in departments where the outbreaks are currently occurring or have occurred;
- Enforcement of visual triage for respiratory diseases in emergency department and outpatient departments and ensure the 24/7 availability of a trained nurse for early detection of patients with respiratory symptoms, and proper documentation in triage forms;
- Extensive training of all healthcare workers on case definition for early detection, implementation of isolation precautions, proper selection, donning and doffing of PPEs, hand hygiene and environmental cleaning and disinfection;
- Ensuring that all healthcare workers tested for N95 fitting (fit test);
- Ensuring availability of infection prevention supplies including hand sanitizer, PPEs, surface disinfectants, portable HEPA filters and fumigation machines;
- Enforcing the implementation of a policy of not allowing healthcare workers to travel without medical clearance to prevent the spread of the virus to other countries.
For cases that report contact with dromedary camels, investigations of MERS-CoV infection in dromedaries is conducted by Ministry of Agriculture officials.
Globally, 2015 laboratory-confirmed cases of infection with MERS-CoV including at least 703 related deaths have been reported to WHO since 2012.
WHO risk assessment
MERS-CoV causes severe human infections resulting in high mortality and has demonstrated the ability to transmit between humans. So far, the observed human-to-human transmission has occurred mainly in health care settings.
The notification of additional cases does not change the overall risk assessment. WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to animals or animal products (for example, following contact with dromedaries) or human source (for example, in a health care setting). WHO is working closely with the Ministry of Health in Saudi Arabia, continues to monitor the epidemiological situation and viral changes, and conducts risk assessment based on the latest available information. To date, there is no indication that there is sustained human-to-human transmission or that the epidemiologic pattern or viral characteristics are different than what has been reported previously.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV early because like other respiratory infections, the early symptoms of MERS-CoV are non-specific. Therefore, health-care workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures.
Until more is understood about MERS-CoV, people with diabetes, renal failure, chronic lung disease, and immunocompromised persons are considered to be at high risk of severe disease from MERS-CoV infection. Therefore, these people should avoid close contact with animals, particularly camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, or eating meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
The Saudi Arabian Ministry of Health (MOH) reported 7 new cases of MERS-CoV, all associated with hospital outbreaks
Wednesday, June 14th, 2017Remembering Orlando’s Pulse: On June 12, 2016, the Pulse nightclub in Orlando was the scene of a mass shooting where 49 people were killed.
Tuesday, June 13th, 2017NY Times 360: https://nyti.ms/2tfu1Pp
https://static01.nyt.com/video/players/offsite/index.html?videoId=100000005156349
In this 360° video, see and hear from some of the people who visited the site and memorialized the victims.






