Archive for September, 2017
Tremors: More than 120,000 people have fled the region around the Mount Agung volcano on the Indonesian tourist island of Bali
Thursday, September 28th, 2017Thousands of cargo containers bearing millions of emergency meals and other relief supplies have been piling up on San Juan’s docks since Saturday.
Thursday, September 28th, 2017‘…..Distributors for big-box companies and smaller retailers are unloading 4,000 20-foot containers full of necessities like food, water and soap this week at a dock in Puerto Rico’s capital operated by Crowley Maritime Corp. In the past few days, Tote Maritime’s terminal has taken the equivalent of almost 3,000. The two facilities have become choke points in the effort to aid survivors of Hurricane Maria.
“There are plenty of ships and plenty of cargo to come into the island,” said Mark Miller, a spokesman for Crowley, based in Jacksonville, Florida. “From there, that’s where the supply chain breaks down — getting the goods from the port to the people on the island who need them.”……’
https://www.youtube.com/watch?v=1lysd3VomDE
NYC is home to 700,000 Puerto Ricans & what are they doing about Puerto Rico?
Thursday, September 28th, 2017“…..Gov. Andrew M. Cuomo announced the launch of the Empire State Relief and Recovery Effort for Puerto Rico, and Mayor Bill de Blasio sent emergency workers to the island to provide aid.
There are now more than 140 city personnel on the ground in Puerto Rico.
Among them: New York Task Force One, our urban search and rescue team; workers from the city’s Buildings Department who have expertise in inspections; members of our Police and Fire Departments who specialize in structural collapses and water rescues; and members of both departments’ Hispanic societies…..”
USVI: “….A week after Maria blew through, the recovery efforts were still lumbering to get off the ground. Power lines sit in tangled piles on the side of the road. Some droop down from broken poles and slap the windshields of cars as they pass by. Houses have been knocked from their foundations and rest precariously on steep hillsides. Piles of garbage grow larger and more fetid by the day, rotting in the tropical sun. And help from the local and federal government can be hard to come by….”
Thursday, September 28th, 2017“….Basic government functions have suffered neglect for years. The government has shortchanged the hospitals of the funding they are supposed to receive. And that has caused the hospitals to fall behind on payments to entities like the local water and power authority, which has raised rates so high on customers that they pay three times as much as the average in the states. Compounding the financial stress, the federal government caps the amount of money it provides the territories for Medicaid…..After Irma hit three weeks ago, aid was slow to trickle into St. Thomas and St. John. When military, law enforcement and emergency medical workers finally did begin to settle in, they were forced to pull out as Maria approached, taking the semblance of safety and order they brought with them…….”
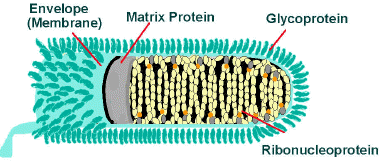
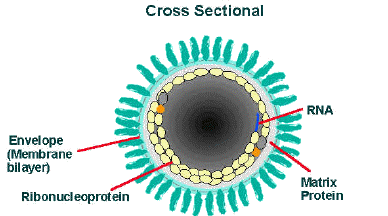
Since 2012, when the virus was first identified in Saudi Arabia, there have been 2081 laboratory-confirmed cases of MERS-CoV infection reported to WHO from 27 countries, with at least 722 deaths – a fatality rate of 35%.
Thursday, September 28th, 2017Countries agree next steps to combat global health threat MERS-CoV
Critical next steps to accelerate the response to the global public health threat posed by Middle-East respiratory syndrome coronavirus (MERS-CoV) have been agreed by representatives from the Ministries of Health and Ministries of Agriculture of affected and at risk countries, and experts. The virus, which circulates in dromedary camels without causing visible disease, can be fatal for humans.
At a meeting hosted by the World Health Organization (WHO), the Food and Agriculture Organization (FAO), and the World Organisation for Animal Health (OIE) in Geneva this week, more than 130 experts from 33 countries, organizations and research institutions met to share what is known about the virus, identify priority research needs, improve cross-collaboration between animal and human health sectors and agree on a plan to address crucial gaps.
“MERS is not only a regional threat. While the majority of human cases have been reported from the Middle-East, the outbreak in the Republic of Korea in 2015 showed MERS’ global reach and capacity to have significant public health and economic consequences,” said Dr Maria Van Kerkhove, MERS-CoV Technical Lead in WHO’s Health Emergencies programme. “We are at the stage where we have to confront the challenges in our ability to detect and respond to MERS outbreaks and improve our knowledge about this virus through collaborative research,” she said.
Since 2012, when the virus was first identified in Saudi Arabia, there have been 2081 laboratory-confirmed cases of MERS-CoV infection reported to WHO from 27 countries, with at least 722 deaths – a fatality rate of 35%. While progress has been made in research and surveillance, significant gaps remain in understanding the virus, including how it circulates in dromedary camels, the natural reservoir host, or how it spills over into the human population.
“MERS-CoV is a disease with a significant impact on public health, which requires further investigations in animal sources to better understand its epidemiology and improve its control in humans. OIE Member Countries are requested to notify any occurrences of MERS-CoV in animals. This crucial information will contribute to escalating a coordinated response from the animal and human health sectors”, said Dr Gounalan Pavade, Chargé de mission, OIE.
More than 80% of MERS cases have been reported from Saudi Arabia. While many of these people were infected in health care facilities, with improved data collection on MERS patients since 2015, a significant proportion of recently reported human cases are believed to have been exposed through direct or indirect contact with infected camels. Frequent international travel has allowed sporadic cases to be exported to every region of the world by individuals who are unknowingly infected before they travel.
“It is in our common interest to address the disease in the human-animal interface, work across sectors and disciplines, together for the sake of our shared goals, healthy people and healthy animals” said Dr Ahmed El Idrissi, Senior Animal Health Officer, FAO. “In doing so we recognize the importance of a One Health approach to health threats of animal origin”.
Human to human transmission remains limited, but health-care associated outbreaks have occurred in several countries in the Middle East and in the Republic of Korea. Infection prevention and control measures are vital to prevent the possible spread of the disease in hospitals and clinics and to protect health-care workers, visitors and other patients. No vaccine or specific treatment is currently available and treatment is supportive and based on the patient’s clinical condition.
MERS-CoV is one of the high threat pathogens included in the WHO’s Research & Development Blue Print which provides a road map for research and development of diagnostic, preventive and therapeutic products for prevention, early detection and response to these threats caused by a list of 11 high prioritized pathogens.
The MERS research priorities and activities being guided by WHO, FAO and OIE build on a series of regional and global meetings organized by the three organizations over the past five years. While tremendous progress has been made, particularly at addressing some key unknowns about the behaviour of this virus in animals and humans, some fundamental gaps about MERS-CoV remain. The global community remains within the grip of this emerging infectious disease.
Madagascar: 93 suspected plague patients have been registered between [1 Aug 2017] and [25 Sep 2017] and 5 of them have died
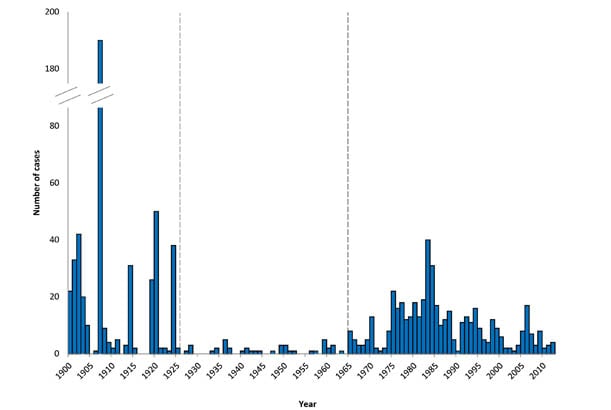
Thursday, September 28th, 2017Plague around the world, 2010–2015
E. Bertherata
“Plague is a bacterial infection mainly affecting small mammals and transmitted by fleas. The geographical distribution of the disease is very focalized. Occasionally, the pathogen Yersinia pestis can infect humans through infected flea bites. Human plague is a serious disease, particularly in its septicaemic and pneumonic forms. The pneumonic form, invariably fatal unless treated early, is especially contagious and can trigger terrifying epidemics through direct person-to-person contact. In these circumstances, plague is simultaneously a medical and a public health emergency.
Between 1 January 2010 and 31 December 2015, 3248 cases of plague in humans were reported, resulting in 584 deaths (Table 1). The principal animal reservoir (which differs from region to region) and local socioeconomic conditions are determinants of the epidemiological characteristics of the disease and the risk of transmission to humans. Plague is a disease of poverty in Africa, South America and India, where the animal reservoir essentially comprises commensal rodents, but tends to be a sporadic disease associated with outdoor occupations in the other endemic regions. ……..”
Africa
“……In Africa, 4 countries still regularly report cases. Madagascar is the most seriously affected country in the world. The surveillance system is relatively effective, thanks to the support of the national Pasteur Institute. Thus, specimens are taken from 95% of suspected cases and nearly 55% of these are confirmed as plague cases. Incidence has declined in the last 2 years but there has been an increase in the overall case fatality rate (23% in 2015) associated with the higher frequency of pneumonic forms (23.3%). This increase in serious forms of the disease is symptomatic of the deteriorating fabric of the health system as a result of the recent social and political crisis in the country. …..”
Adventure of the Seas was scheduled to arrive on Wednesday for humanitarian calls in San Juan, St. Thomas and St. Croix to aid in evacuation and to donate critical supplies. Evacuees on the ship are also scheduled to be ferried to Fort Lauderdale.
Thursday, September 28th, 2017September 28 is World Rabies Day
Thursday, September 28th, 2017September 28 is World Rabies Day, a global health observance started in 2007 to raise awareness about the burden of rabies and bring together partners to enhance prevention and control efforts worldwide. World Rabies Day is observed in many countries, including the United States.
While rabies is a 100% preventable disease, thousands of people die from the disease around the world each day. World Rabies Day is an opportunity to reflect on our efforts to control this deadly disease and remind ourselves that the fight is not yet over.
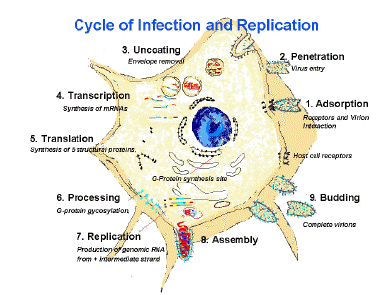
After 1 RN was infected with MERS-CoV in a Saudi Arabian hospital in 2015, investigators determined that 4.6% of healthcare worker (HCW) contacts eventually contracted the virus.
Wednesday, September 27th, 2017Middle East respiratory syndrome coronavirus transmission among health care workers: Implication for infection control
Alfaraj, Sarah H. et al.
American Journal of Infection Control
“…..During the study period in 2015, the index case was a 30-year-old Filipino nurse who had a history of unprotected exposure to a MERS-CoV–positive case on May 15, 2015, and had multiple negative tests for MERS-CoV. Weeks later, she was diagnosed with pulmonary tuberculosis and MERS-CoV infection. A total of 73 staff were quarantined for 14 days, and nasopharyngeal swabs were taken on days 2, 5, and 12 postexposure. Of those contacts, 3 (4%) were confirmed positive for MERS-CoV. An additional 18 staff were quarantined and had MERS-CoV swabs. A fourth case was confirmed positive on day 12. Subsequent contact investigations revealed a fourth-generation transmission. Only 7 (4.5%) of the total 153 contacts were positive for MERS-CoV….”
Bubonic Plague in History
Wednesday, September 27th, 2017Model-based analysis of an outbreak of bubonic plague in Cairo in 1801
“….Bubonic plague is arguably the most devastating infectious disease that mankind has ever been confronted with. Its causative agent, Yersinia pestis, has recently been detected in several human remains dated from the third millennium BCE but at that time lacked the ability to cause epidemics of bubonic plague transmitted by ectoparasites [1,2]. Genetic adaptation to the flea-borne pathogenic lifestyle is estimated to have happened shortly before the beginning of the first millennium BCE [1,3,4], which coincides with some of the first historical descriptions of epidemics that have been putatively attributed to bubonic plague. Ancient historical descriptions are, however, typically insufficient to reach a clear verdict of plague. For example, the disease that struck the Philistines in the eleventh century BCE has been proposed to be the earliest known outbreak of bubonic plague, but could in fact have been caused by dysentery or tularaemia [5,6]. Likewise, the outbreak that ravaged Athens in 430 BCE could have been a number of infectious diseases other than plague, such as Ebola [7,8]. Although there would certainly have been earlier cases at least sporadically, the first human deaths that have been conclusively attributed to Y. pestis using DNA evidence occurred in the sixth century CE, during the so-called plague of Justinian [9,10]. This epidemic was first reported by the contemporary historian Procopius in Egypt in 541 CE, and it would have spread rapidly on ships carrying grain to Constantinople and throughout the Byzantine empire [11]. The first plague pandemic followed, which ravaged Mediterranean and European regions through several waves over the next 200 years [12]. The second plague pandemic started in 1347 with the so-called Black Death epidemic. Once again, DNA evidence has been used to incriminate Y. pestis as the infectious agent [13,14]. The epidemic originated in Central Asia before spreading throughout Europe via trade routes [15]. In Western Europe, the second pandemic lasted until the end of the seventeenth century, with the Marseilles plague of 1720 being an exceptionally late outbreak [16]. For example, in England, the last major outbreak took place in 1665 in London and a few secondary locations [17,18]. Finally, a third pandemic started around 1855 which ravaged China and India for almost a century, and during which the causative bacteria Y. pestis was discovered as well as its flea-borne mode of transmission [19].
Phylogenetic evidence indicates that the third pandemic was caused by a direct descendant from the lineage that had caused the second pandemic [10,15]. Between the end of the second and the beginning of the third pandemic, this lineage would have been restricted to the Middle East [10]. Outbreaks of bubonic plague were indeed regularly reported during the interpandemic period, for example, in Iraq [20], in Syria [21] and in Egypt [21–25]. A comprehensive survey of historical reports of epidemics shows that throughout the eighteenth century and the first half of the nineteenth century, plague was documented in Asia Minor in approximately 85% of years, in Lower Egypt in approximately 30% of years and in Syria in approximately 20% of years [26]. This recurrence of plague in the Middle East at a time when Europe was free of it significantly contributed to the weakening of the Ottoman Empire [22]. Several Western visitors were surprised by the lack of measures taken by the local population to try and protect itself from the disease [25,26]. Very high plague death tolls were recorded by contemporary writers, but many of these were exaggerated and the aetiology is often unclear [25,27]. Thus, although it is beyond doubt that the Middle East was frequently hit by plague between 1700 and 1850, little is known about this important connecting link between the second and third pandemics, and there are virtually no reliable data available for formal epidemiological investigation.
A notable exception concerns the short period from 1798 to 1801 during which a French revolutionary expedition into Ottoman Egypt was led by the future emperor Napoleon Bonaparte. Many French scientists accompanied this expedition, who studied many aspects of the Egyptian country they visited, such as its topography, climate, history, demography and languages. The expedition included a large number of medical officers headed by René Desgenettes who together collected a wealth of medical observations about the health of the Egyptian population [28,29]. Upon his return, Desgenettes reported his findings in a book entitled ‘Histoire médicale de l’armée d’Orient’ which includes a table of the daily number of deaths recorded among men, women and children living in Cairo [30]. This daily mortality statistical table covers an epidemic of plague that took place in early 1801 and which is briefly mentioned in Desgenettes’ book [30] as well as a few monographs written by other medical officers returning from the French expedition [31–33] and secondary sources [34–36]. These data present a unique opportunity to dissect how an outbreak of bubonic plague unfolded in interpandemic Egypt….”