Archive for October, 2017
H7N9: Global time bomb
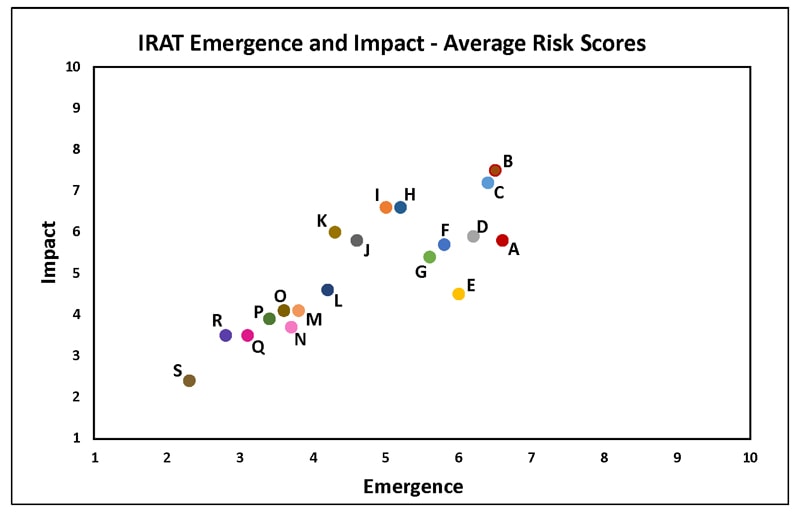
Friday, October 20th, 2017Summary of Influenza Risk Assessment Tool (IRAT) Results
The Influenza Risk Assessment Tool (IRAT) is an evaluation tool conceived by CDC and further developed with assistance from global animal and human health influenza experts. The IRAT is used to assess the potential pandemic risk posed by influenza A viruses that are not currently circulating in people. Input is provided by U.S. government animal and human health influenza experts. Information about the IRAT is available at Influenza Risk Assessment Tool (IRAT) Questions and Answers(https://www.cdc.gov/flu/pandemic-resources/national-strategy/risk-assessment.htm).
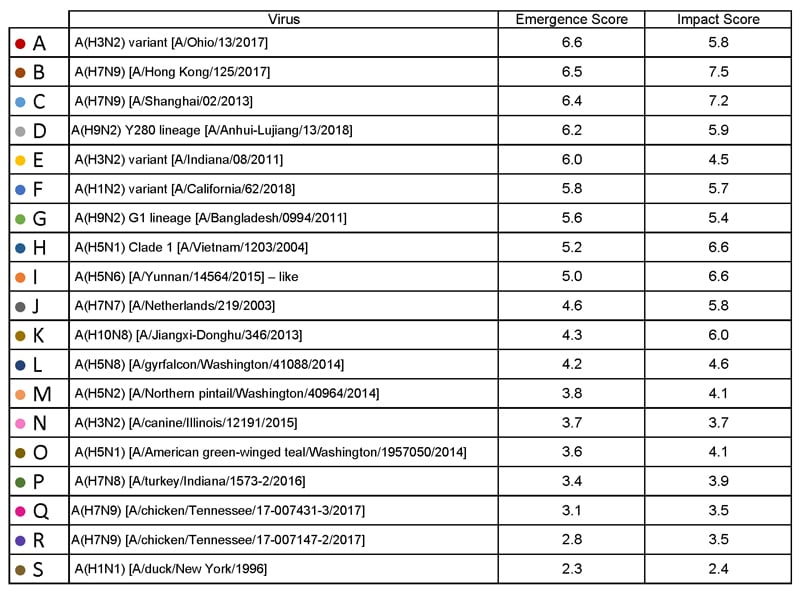
Below is a table of results for influenza A viruses that have been assessed using IRAT because they serve as a representative of a particular subtype or are of unique interest.
| Virus | Most Recent Date Evaluated | Potential Emergence Risk(https://www.cdc.gov/flu/pandemic-resources/tools/risk-assessment.htm#emergence-risk) | Potential Impact Risk(https://www.cdc.gov/flu/pandemic-resources/tools/risk-assessment.htm#impact-risk) | Overall Summary |
|---|---|---|---|---|
| H1N1 [A/duck/New York/1996] | Nov 2011 | 2.3 | 2.4 | Low |
| H3N2 variant [A/Indiana/08/2011] | Dec 2012 | 6.0 | 4.5 | Moderate |
| H3N2 [A/canine/Illinois/12191/2015] | June 2016 | 3.7 | 3.7 | Low |
| H5N1 Clade 1 [A/Vietnam/1203/2004] | Nov 2011 | 5.2 | 6.6 | Moderate |
| H5N1 [A/American green-winged teal/Washington/1957050/2014] | Mar 2015 | 3.6 | 4.1 | Low-Moderate |
| H5N2 [A/Northern pintail/Washington/40964/2014] | Mar 2015 | 3.8 | 4.1 | Low-Moderate |
| H5N6 [A/Yunnan/14564/2015] – like | Apr 2016 | 5.0 | 6.6 | Moderate |
| H5N8 [A/gyrfalcon/Washington/41088/2014] | Mar 2015 | 4.2 | 4.6 | Low-Moderate |
| H7N7 [A/Netherlands/2019/2003] | Jun 2012 | 4.6 | 5.8 | Moderate |
| H7N8 [A/turkey/Indiana/1573-2/2016] | July 2017 | 3.4 | 3.9 | Low |
| H7N9 [A/Hong Kong/125/2017] | May 2017 | 6.5 | 7.5 | Moderate-High |
| H7N9 [A/Shanghai/02/2013] | Apr 2016 | 6.4 | 7.2 | Moderate-High |
| H9N2 G1 lineage [A/Bangladesh/0994/2011] | Feb 2014 | 5.6 | 5.4 | Moderate |
| H10N8 [A/Jiangxi-Donghu/346/2013] | Feb 2014 | 4.3 | 6.0 | Moderate |
H1N1: [North American avian H1N1 [A/duck/New York/1996]
Avian influenza A viruses are designated as highly pathogenic avian influenza (HPAI) or low pathogenic avian influenza (LPAI) based on molecular characteristics of the virus and the ability of the virus to cause disease and death in chickens in a laboratory setting. North American avian H1N1 [A/duck/New York/1996] is a LPAI virus and in the context of the IRAT serves as an example of a low risk virus.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the low risk category (less than 3). Similarly the average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission also falls into the low risk range (less than 3).
H3N2 Variant:[A/Indiana/08/11]
Swine-origin flu viruses do not normally infect humans. However, sporadic human infections with swine-origin influenza viruses have occurred. When this happens, these viruses are called “variant viruses.” Influenza A H3N2 variant viruses (also known as “H3N2v” viruses) with the matrix (M) gene from the 2009 H1N1 pandemic virus were first detected in people in July 2011. The viruses were first identified in U.S. pigs in 2010. In 2011, 12 cases of H3N2v infection were detected in the United States. In 2012, 309 cases of H3N2v infection across 12 states were detected. The latest risk assessment for this virus was conducted in December 2012 and incorporated data regarding population immunity that was lacking a year earlier.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the moderate risk category (less than 6). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the low-moderate risk category (less than 5).
H3N2: [A/canine/Illinois/12191/2015]
The H3N2 canine influenza virus is an avian flu virus that adapted to infect dogs. This virus is different from human seasonal H3N2 viruses. Canine influenza A H3N2 virus was first detected in dogs in South Korea in 2007 and has since been reported in China and Thailand. It was first detected in dogs in the United States in April 2015(https://www.cdc.gov/flu/news/canine-influenza-update.htm). H3N2 canine influenza has reportedly infected some cats as well as dogs. There have been no reports of human cases.
Summary: The average summary risk score for the virus to achieve sustained human-to-human transmission was low risk (less than 4). The average summary risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the low risk range (less than 4).
H5N1 clade 1: [A/Vietnam/1203/2004]
The first human cases of highly pathogenic avian influenza (HPAI) H5N1 virus were reported from Hong Kong in 1997. Since 2003, highly pathogenic H5N1 avian influenza viruses have caused over 850 laboratory-confirmed human cases; mortality among these cases was high. A risk assessment of this H5N1 clade 1 virus was conducted in 2011 soon after the IRAT was first developed and when 12 hemagglutinin (HA) clades were officially recognized.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the moderate risk category (less than 6). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the high-moderate risk category (less than 7).
H5N1: [A/American green winged teal/Washington/1957050/2014]
In December 2014, an H5N1 highly pathogenic avian influenza virus was first isolated from an American green-winged teal in the state of Washington. This virus is a recombinant virus containing four genes of Eurasian lineage (PB2, HA, NP and M) and four genes of North American lineage (PB1, PA, NA and NS).In February 2015, the Canadian government reported isolating this virus from a backyard flock in the Fraser Valley. When this risk assessment was conducted in 2015, these were the only reported isolations of this virus. There have been no reports of human cases.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the low risk category (less than 4). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the low-moderate risk category (less than 5).
H5N2: [A/Northern pintail/Washington/40964/2014]
In December 2014, an H5N2 highly pathogenic avian influenza virus was first reported by the Canadian government from commercial poultry in the Fraser Valley.Subsequently this virus was isolated from wild birds, captive wild birds, backyard flocks and commercial flocks in the United States.This virus is a recombinant virus composed of five Eurasian lineage (PB2, PA, HA, M and NS) genes and three North American lineage (PB1, NP and NA) genes. There have been no reports of human cases.
Summary: The average summary risk score for the virus to achieve sustained human-to-human transmission was low risk (less than 4).The average summary risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the low-moderate risk range (less than 5).
H5N6: [A/Yunnan/14564/2015 (H5N6-like)]
Between January 2014 and March 2016, there have been 10 human cases of H5N6 highly pathogenic avian influenza reported. Nine reportedly experienced severe disease and six died. Avian outbreaks of this virus were first reported from China in 2013. Subsequently avian outbreaks have been reported in at least three countries (China, Vietnam and Lao PDR) through 2015.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the moderate range (less than 6).The average summary risk score for the virus to significantly impact on public health if it were to achieve sustained human-to-human transmission fell in the moderate range (less than 7).
H5N8: [A/gyrfalcon/Washington/41088/2014]
In December 2014, an H5N8 highly pathogenic avian influenza virus was first isolated from a sample collected in the United States from a captive gyrfalcon.Subsequently this virus was isolated from wild birds, captive wild birds, backyard flocks and commercial flocks in the United States.This virus (clade 2.3.4.4) is similar to Eurasian lineage H5N8 viruses that have been isolated in South Korea, China, Japan, the Netherlands, the United Kingdom and Germany in late 2014-early 2015.There have been no reports of human cases.
Summary: The average risk score for the virus to achieve sustained human-to-human transmission was in the low-moderate range< (less than 5). The average summary risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission fell in the low-moderate range (less than 5).
In 2003 the Netherlands reported highly pathogenic avian influenza (HPAI) in approximately 255 commercial flocks.Coinciding with human activities around these infected flocks, 89 human cases of H7N7 were identified.Cases primarily reported conjunctivitis, although a few also reported mild influenza-like illness.There was one death.
Summary: The summary average risk score for this virus to achieve sustained human-to-human transmission was in the low-moderate risk range (less than 5). The summary average risk score for this virus to significantly impact the public’s health if it were to achieve sustained human-to-human transmission fell in the moderate risk range (less than 7).
H7N8: [A/turkey/Indiana/1573-2/2016]
In January 2016, a highly pathogenic avian influenza (HPAI) virus of North American lineage was identified in a turkey flock in Indiana. Putative low pathogenic avian influenza (LPAI) viruses similar to A/turkey/Indiana/1573-2/2016 were subsequently isolated from 9 other turkey flocks in the area. There were no reports of human cases associated with this virus at the time of the IRAT scoring.
Summary: A risk assessment of this LPAI virus was conducted in July 2017. The overall IRAT risk assessment score for this virus falls into the low risk category (< 4). The summary average risk score for the virus to achieve sustained human-to-human transmission is in the low risk category (3.4). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was also in the low risk category (3.9).
Low pathogenic avian influenza (LPAI) H7N9 viruses were first reported from China in March 2013. These viruses were first scored using the IRAT in March 2013 and again in April 2013, and then annually in 2014, 2015, and 2016 with no change in overall risk scores. Between October 2016 and May 2017 evidence of two divergent lineages of these viruses was detected – the Pearl River Delta lineage and the Yangtze River Delta lineage. The IRAT was used to assess LPAI H7N9 [A/Hong Kong/125/2017], a representative of the Yangtze River Delta viruses.
Summary: A risk assessment of H7N9 [A/Hong Kong/125/2017] was conducted in May 2017. The overall IRAT risk assessment score for this virus falls into the moderate-high risk category and is similar to the scores for the previous H7N9 viruses. The summary average risk score for the virus to achieve sustained human-to-human transmission is in the moderate risk category (less than 7). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the moderate-high risk category (less than 8).
H7N9: Avian H7N9 [A/Shanghai/02/2013]
On 31 March 2013, the China Health and Family Planning Commission notified the World Health Organization (WHO) of three cases of human infection with influenza H7N9. As of August 2016, the WHO has received reports of 821 cases, 305 have died. This low pathogenic avian influenza virus was rescored most recently in April 2016 with no substantive change in risk scores since May 2013.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the moderate risk category (less than 7). The average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission fell in the high-moderate risk range (less than 8).
H9N2: Avian H9N2 G1 lineage [A/Bangladesh/0994/2011]
Human infections with influenza AH9N2 virus have been reported sporadically, cases reportedly exhibited mild influenza-like illness. Historically these low pathogenic avian influenza viruses have been isolated from wild and domestic birds. In response to these reports, a risk assessment of this H9N2 influenza virus was conducted in 2014.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was in the moderate risk category (less than 6). The summary average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission also fell in the moderate risk range (less than 6).
H10N8: Avian H10N8 [A/Jiangxi-Donghu/346/2013]
Two human infections with influenza A(H10N8) virus were reported by the China Health and Family Planning Commission in 2013 and 2014 (one each year). Both cases were hospitalized and one died. Historically low pathogenic avian influenza H10 and N8 viruses have been recovered from birds. A risk assessment of the H10N8 influenza was conducted in 2014.
Summary: The summary average risk score for the virus to achieve sustained human-to-human transmission was low-moderate (less than 5). The average risk score for the virus to significantly impact public health if it were to achieve sustained human-to-human transmission was in the moderate risk range (less than 7).
“My World is Finished”: Rohingya targeted in crimes against humanity in Myanmar
Thursday, October 19th, 2017“…..The Rome Statute of the International Criminal Court lists 11 types of acts which, when knowingly committed during such an attack, constitute crimes against humanity. Amnesty International has consistently documented at least six of these amid the current wave of violence in northern Rakhine State: murder, deportation and forcible displacement, torture, rape and other sexual violence, persecution, and other inhumane acts such as denying food and other life-saving provisions……”
“More than 530,000 Rohingya men, women and children have fled northern Rakhine State in terror in a matter of weeks amid the Myanmar security forces’ targeted campaign of widespread and systematic murder, rape and burning, Amnesty International said today in its most detailed analysis yet of the ongoing crisis.
‘My World Is Finished’: Rohingya Targeted in Crimes against Humanity in Myanmar describes how Myanmar’s security forces are carrying out a systematic, organized and ruthless campaign of violence against the Rohingya population as a whole in northern Rakhine State, after a Rohingya armed group attacked around 30 security posts on 25 August.
Dozens of eyewitnesses to the worst violence consistently implicated specific units, including the Myanmar Army’s Western Command, the 33rd Light Infantry Division, and the Border Guard Police. ……”+
Since Sunday, 10,000 to 15,000 Rohingya have crossed into Bangladesh at Anjuman Para
Thursday, October 19th, 2017Predicting Ebola in a patient: Headache, diarrhea, difficulty breathing, nausea and vomiting, loss of appetite, and conjunctivitis. The laboratory tests most useful were creatinine, creatine kinase, alanine aminotransferase, and total bilirubin.
Thursday, October 19th, 2017Oza, S., Sesay, A. A., Russell, N. J., Wing, K., Boufkhed, S., Vandi, L….Checchi, F. (2017). Symptom- and Laboratory-Based Ebola Risk Scores to Differentiate Likely Ebola Infections. Emerging Infectious Diseases, 23(11), 1792-1799. https://dx.doi.org/10.3201/eid2311.170171.
“…..This risk score correctly identified 92% of Ebola-positive patients as high risk for infection; both scores correctly classified >70% of Ebola-negative patients as low or medium risk. Clinicians can use these risk scores to gauge the likelihood of triaged patients having Ebola while awaiting laboratory confirmation…..”
Guidelines focusing on the delivery of supportive care measures to patients in Ebola treatment units where health care resources are limited
Thursday, October 19th, 2017Evidence-based guidelines for supportive care of patients with Ebola virus disease
Lamontagne, François et al.
The Lancet

Seychelles – Suspected Plague
Wednesday, October 18th, 2017Seychelles – Suspected Plague (Ex- Madagascar)
Madagascar is experiencing a large outbreak of plague affecting major cities and other non-endemic areas since August 2017. This outbreak caries a moderate risk of spread to neighbouring Indian Ocean islands. This risk has been mitigated by the short incubation period (the time from exposure to onset of symptoms) of pneumonic plague and the institution of exit screening measures at the airport and other major ports. For more information, see the latest situation report available from:
On 10 October 2017, the Seychellois Ministry of Health notified WHO of a probable case of pneumonic plague. The probable case is a 34-year-old man who had visited Madagascar and returned to Seychelles on 6 October 2017. He developed symptoms on 9 October 2017 and presented to a local health centre. Based on a medical examination and reported history of recent travel to Madagascar, pneumonic plague infection was suspected and he was immediately referred to hospital where he was isolated and treated.
A rapid diagnostic test (RDT) performed within the country on 11 October on a sputum sample was weakly positive. Since then he has been treated as a probable case until confirmation by a WHO plague reference laboratory is completed. The specimen is being sent to Institut Pasteur in Paris, France for confirmation. The patient continues to be hospitalized in isolation until completion of the antibiotic treatment. He is currently asymptomatic and in stable condition.
Between 9 and 11 October 2017, eight of his contacts developed mild symptoms and have been isolated. Two other suspected cases, without any established epidemiological link to the probable case, have also been identified isolated and are on treatment.
In total 10 laboratory specimens have been collected from the probable case, his contacts and the two suspected cases and are being shipped to Institut Pasteur in France for testing.
October 13 was the last day of monitoring of over 320 contact persons of the probable case, including 41 passengers and seven crew from the flight, 12 close family members, and 18 staff and patients from the health centre visited by the probable case. All were provided a prophylactic course of antibiotics to prevent the disease.
In addition, 577 children and 63 teachers in potential contact with one of the individual identified by contact tracing were given antibiotics as a prophylaxis precautionary measure. Thus contact tracing is done thoroughly.
Currently only eleven (11) close contacts and one foreign national who was not in contact with the probable case but recently arrived from Madagascar, are hospitalised as precautionary measure and will remain in the hospital on treatment although they do not present signs of respiratory distress.
Public health response
A Crisis Emergency Committee was established on 10 October, and has since then, been meeting daily to coordinate surveillance, contact tracing, case management, isolation and supplies.
A hotline was revived on 12th October.
The Government has allocated funds to support the Committee interventions, enabling the setting up of a temporary isolation ward (whilst the existing ward is expanded), procurement of key supplies, contact tracing, and expanded contact tracers training next week, etc.
Air Seychelles flights to-from Madagascar were stopped from 8 October to reduce likelihood of further importation of cases from Madagascar.
WHO does not recommend restrictions on travel and trade, based on the currently available information.
On 10 October 2017, Madagascar Ministry of Health, with support from WHO, has implemented exit screening at the international airport in Antananarivo to prevent international spread. Further support from WHO and partners is being planned to strengthen measures at points of entry to avoid international spread.
WHO has deployed three epidemiologists and one risk communication officer to support the Country Office and Ministry of Public Health in responding to the current situation.
WHO risk assessment
Plague is an infectious disease caused by the bacteria Yersinia pestis, a zoonotic bacterium, usually found in small mammals and their fleas. Humans can be contaminated by the bite of infected fleas, through direct contact with infected materials or animals or by inhalation.
There are three forms of plague infection, depending on the route of infection: bubonic, septicaemic and pneumonic.
Pneumonic plague is the most virulent form of plague and can trigger severe epidemics through person-to-person contact via droplets in the air. Incubation period can be as short as 24 hours. Typically, the pneumonic form is caused by spread to the lungs from advanced bubonic plague. However, a person with secondary pneumonic plague may form aerosolized infective droplets and transmit plague to other humans. Plague is treatable disease; however, untreated pneumonic plague is always fatal.
Plague has never been reported in Seychelles, and at this stage, no cases have been definitively confirmed. The case reported above being considered as probable until final classification according to the laboratory results that will be performed at Institut Pasteur in Paris.
The Seychelles Government has established precautionary measures including, enhanced surveillance, isolation and treatment of suspect cases, contact tracing and prophylactic treatment of potential contact.
The risk of further spread in the Seychelles (should the case be confirmed) is considered as low and the overall regional and global risk levels as very low.
WHO travel advice
At this stage, there is a very low risk international travellers would come into contact with plague in Seychelles. WHO advises against any restriction on travel or trade on Seychelles or Madagascar based on the available information.
On 3 October 2017, WHO published advice for international travellers in relation to the outbreak of plague in Madagascar, which should also be followed for travellers to Seychelles.
- Plague – Madagascar
Information for international travellers
On 11 October, the Ministry of Health announced several measures against pneumonic in a press release on its website. As many of these measures significantly interfere with international traffic, on 13 October, the Ministry of Health informed WHO that it will provide the scientific evidence and public health rationale for these measures, as required by Article 43.3 of the International Health Regulations (IHR, 2005).
- Measures reinforced to contain pneumonic plague
Ministry of Health, Republic of Seychelles - International Health Regulations (2005)
For further information on plague, including prevention measures, please visit the WHO Plague website.
“….public health officials say that, in the aftermath of an extreme weather event like a hurricane, the toll of long-term psychological injuries builds in the months and years that follow, outpacing more immediate injuries and swamping the health care system long after emergency workers go home and shelters shut down. ….”
Wednesday, October 18th, 2017“….. As flood waters recede from Hurricanes Harvey, Irma, Maria and Nate, and survivors work to rebuild communities in Texas, Florida and the Caribbean, mental health experts warn that the hidden psychological toll will mount over time, expressed in * *
- heightened rates of depression,
- anxiety,
- post-traumatic stress disorder,
- substance abuse,
- domestic violence,
- divorce,
- murder and
- suicide. …..”
CDC: Preparing your medicine cabinet in case of an emergency
Tuesday, October 17th, 2017Preparing Your Medicine Cabinet for an Emergency: A Checklist
Posted on October 16, 2017 by

If you read our blog on a regular basis you can probably recite the mantra “Make a kit. Have a plan. Be informed.” in your sleep. You are probably familiar with the important items you should keep in your emergency kit – water, food, a flashlight, and a battery-powered radio. What you may not think about is personalizing your kit for your unique medical needs or the needs of your family. Particularly, including prescription medications and other medical supplies in your emergency kit and plans.
As a pharmacist whose job is focused on emergency preparedness and response, I want to give you 10 pointers about how to prepare your medications for an emergency so you can decrease the risk of a life-threatening situation.
- Make a list. Keep a list of all your medications and the dosages in your emergency kit. Make sure you have the phone numbers for your doctors and pharmacies.
- Have your card. Keep your health insurance or prescription drug card with you at all times so your pharmacy benefits provider or health insurance plan can help you replace any medication that was lost or damaged in a disaster.
- Keep a record. Make copies of your current prescriptions and keep them in your emergency kit and/or go bag. You can also scan and email yourself copies, or save them in the cloud. If you can’t reach your regular doctor or your usual pharmacy is not open, this written proof of your prescriptions make it much easier for another doctor to write you a refill.
- Start a stockpile. During and after a disaster you may not be able to get your prescriptions refilled. Make sure you have at least 7 – 10 days of your medications and other medical supplies. Refill your prescription as soon as you are able so you can set aside a few extra days’ worth in your emergency kit to get you through a disaster.
- Storage matters. Keep your medications in labeled, child-proof containers in a secure place that does not experience extreme temperature changes or humidity. Don’t forget to also include nonprescription medications you might need, including pain relievers, cold or allergy medications, and antacids.
- Rotate the date. Don’t let the medications in your emergency supply kit expire. Check the dates at least twice every year.
- Prioritize critical medicines. Certain medications are more important to your health and safety than others. Prioritize your medications, and make sure you plan to have the critical medications available during an emergency.
- Communicate a plan. Talk to your doctor about what you should do in case you run out of a medication during an emergency. If you have a child who takes a prescription medication, talk to their daycare provider or school about a plan in case of an emergency.
- Plan ahead. Make sure you know the shelf life and optimal storage temperature for your prescriptions, because some medications and supplies cannot be safely stored for long periods of time at room temperature. If you take a medication that needs to be refrigerated or requires electronic equipment plan ahead for temporary storage and administration in an emergency situation.
- Check before using. Before using the medication in your emergency kit, check to make sure the look or smell hasn’t changed. If you are unsure about its safety, contact a pharmacist or healthcare provider before using.
Resources
- Centers for Disease Control and Prevention: Gather Emergency Supplies
- Express Scripts: Emergency Preparedness for Prescription Medications
Posted on October 16, 2017 by




