Archive for December, 2017
Trust for America’s Health: “As a nation, we—year after year—fail to fully support public health and preparedness. If we don’t improve our baseline funding and capabilities, we’ll continue to be caught completely off-guard when hurricanes, wildfires, and infectious disease outbreaks hit.”
Wednesday, December 20th, 2017“…..the country does not invest enough to maintain strong, basic core capabilities for health security readiness and, instead, is in a continued state of inefficiently reacting with federal emergency supplemental funding packages each time a disaster strikes.
According to Ready or Not?, federal funding to support the base level of preparedness has been cut by more than half since 2002, which has eroded advancements and reduced the country’s capabilities…..
The report card is based on 10 key indicators of public health preparedness. Half of all states scored a 5 or lower (out of 10), with Alaska scoring the lowest (2), and Massachusetts and Rhode Island scoring the highest (9). Delaware, North Carolina, and Virginia each scored 8 out of 10. Florida received a 6.….
Some key findings include:
- Just 19 states and Washington, D.C. increased or maintained funding for public health from Fiscal Year (FY) 2015-2016 to FY 2016-2017.
- The primary source for state and local preparedness for health emergencies has been cut by about one-third (from $940 million in FY 2002 to $667 million in FY 2017) and hospital emergency preparedness funds have been cut in half ($514 million in FY 2003 to $254 million in FY 2017).
- In 20 states and Washington, D.C. 70 percent or more of hospitals reported meeting Antibiotic Stewardship Program core elements in 2016.
- Just 20 states vaccinated at least half of their population (ages 6 months and older) for the seasonal flu from Fall 2016 to Spring 2017—and no state was above 56 percent.
- 47 state labs and Washington, D.C. provided biosafety training and/or provided information about biosafety training courses (July 1, 2016 to June 30, 2017).
The Ready or Not? report provides a series of recommendations that address many of the major gaps in emergency health preparedness, including:
- Communities should maintain a key set of foundational capabilities and focus on performance outcomes in exchange for increased flexibility and reduced bureaucracy.
- Ensuring stable, sufficient health emergency preparedness funding to maintain a standing set of core capabilities so they are ready when needed. In addition, a complementary Public Health Emergency Fund is needed to provide immediate surge funding for specific action for major emerging threats.
- Strengthening and maintaining consistent support for global health security as an effective strategy for preventing and controlling health crises. Germs know no borders.
- Innovating and modernizing infrastructure needs – including a more focused investment strategy to support science and technology upgrades that leverage recent breakthroughs and hold the promise of transforming the nation’s ability to promptly detect and contain disease outbreaks and respond to other health emergencies.
- Recruiting and training a next generation public health workforce with expert scientific abilities to harness and use technological advances along with critical thinking and management skills to serve as Chief Health Strategist for a community.
- Reconsidering health system preparedness for new threats and mass outbreaks. Develop stronger coalitions and partnerships among providers, hospitals and healthcare facilities, insurance providers, pharmaceutical and health equipment businesses, emergency management and public health agencies.
- Preventing the negative health consequences of climate change and weather-related threats. It is essential to build the capacity to anticipate, plan for and respond to climate-related events.
- Prioritizing efforts to address one of the most serious threats to human health by expanding efforts to stop superbugs and antibiotic resistance.
- Improving rates of vaccinations for children and adults – which are one of the most effective public health tools against many infectious diseases.
- Supporting a culture of resilience so all communities are better prepared to cope with and recover from emergencies, particularly focusing on those who are most vulnerable. Sometimes the aftermath of an emergency situation may be more harmful than the initial event. This must also include support for local organizations and small businesses to prepare for and to respond to emergencies…….”
Twelve cruise ship passengers on an excursion in Mexico’s Yucatán region died after their tour bus flipped on a two-lane highway early Tuesday
Wednesday, December 20th, 2017Congenitally acquired Chagas disease reported in Canada
Wednesday, December 20th, 2017During December 2016–June 2017, the largest global epidemic of meningitis caused by Neisseria meningitidis Serogroup C occurred in northern Nigeria, with 14,518 suspected cases and 1,166 deaths reported.
Wednesday, December 20th, 2017Large Outbreak of Neisseria meningitidis Serogroup C — Nigeria, December 2016–June 2017
Weekly / December 15, 2017 / 66(49);1352–1356
Chimeremma Nnadi, MD, PhD1; John Oladejo, MBBS2; Sebastian Yennan, MPH2; Adesola Ogunleye, DDS2; Chidinma Agbai, MPH3; Lawal Bakare, MBBS2; Mohammed Abdulaziz, MBBS4; Amina Mohammed, MBBS5; Mary Stephens, MBBS6; Kyadindi Sumaili, MPH7; Olivier Ronveaux, MBBS8; Helen Maguire, MBBS9; Debra Karch, PhD10; Mahmood Dalhat, MBBS11; Martin Antonio, PhD12; Andre Bita, MBBS13; Ifeanyi Okudo, MBBS6; Patrick Nguku, MBBCH11; Ryan Novak, PhD14; Omotayo Bolu, MD15; Faisal Shuaib, DrPH5; Chikwe Ihekweazu, MBBS2 (View author affili
Summary
What is already known about this topic?
Meningococcal disease caused by Neisseria meningitidis causes severe illness, and could lead to permanent disability or death if not quickly detected and treated. The largest global burden of meningococcal disease is in sub-Saharan Africa, where annual epidemics caused mainly by N. meningitidis serogroup A were previously common. After the introduction of meningococcal A vaccines in 2013, meningitis caused by serogroup A declined. However, N. meningitidis serogroup C (NmC) has now emerged as a cause of large outbreaks.
What is added by this report?
During December 2016–June 2017, the largest global epidemic of meningitis caused by NmC occurred in northern Nigeria, with 14,518 suspected cases and 1,166 deaths reported. An emergency operations center coordinated rapid development and implementation of an emergency outbreak response plan, including administration of meningococcal serogroup C–containing vaccines to >2 million persons. Multiple logistical challenges were encountered during the response; the outbreak was declared over in June 2017.
What are the implications for public health practice?
National and regional evaluations of the outbreak response have outlined recommendations for improving meningitis outbreak prevention, timely detection, and response in Nigeria. Implementation of these recommendations will be key to reducing future meningitis outbreaks. Expanding availability of multivalent vaccines that are effective against non-A serogroups of N. meningitidis might prevent future outbreaks in this region.
On February 16, 2017, the Ministry of Health in Zamfara State, in northwestern Nigeria, notified the Nigeria Centre for Disease Control (NCDC) of an increased number of suspected cerebrospinal meningitis (meningitis) cases reported from four local government areas (LGAs). Meningitis cases were subsequently also reported from Katsina, Kebbi, Niger, and Sokoto states, all of which share borders with Zamfara State, and from Yobe State in northeastern Nigeria. On April 3, 2017, NCDC activated an Emergency Operations Center (EOC) to coordinate rapid development and implementation of a national meningitis emergency outbreak response plan. After the outbreak was reported, surveillance activities for meningitis cases were enhanced, including retrospective searches for previously unreported cases, implementation of intensified new case finding, and strengthened laboratory confirmation. A total of 14,518 suspected meningitis cases were reported for the period December 13, 2016–June 15, 2017. Among 1,339 cases with laboratory testing, 433 (32%) were positive for bacterial pathogens, including 358 (82.7%) confirmed cases of Neisseria meningitidis serogroup C. In response, approximately 2.1 million persons aged 2–29 years were vaccinated with meningococcal serogroup C–containing vaccines in Katsina, Sokoto, Yobe, and Zamfara states during April–May 2017. The outbreak was declared over on June 15, 2017, after high-quality surveillance yielded no evidence of outbreak-linked cases for 2 consecutive weeks. Routine high-quality surveillance, including a strong laboratory system to test specimens from persons with suspected meningitis, is critical to rapidly detect and confirm future outbreaks and inform decisions regarding response vaccination.
Background
All northern Nigeria states lie within the sub-Saharan “Meningitis Belt,” a region of 26 countries that experiences the largest burden of meningococcal disease, with annual epidemics reported during the December–June dry season. Meningitis causes severe illness, and if not detected and treated quickly, could lead to permanent disability that puts a significant burden on families. In many settings, approximately 10% of meningitis cases ultimately result in death. Before introduction of the meningococcal serogroup A conjugate vaccine (MenAfriVac) in 2013 (1), Nigeria experienced some of the largest epidemics of meningococcal meningitis, including the 1996 N. meningitidis serogroup A (NmA) epidemic that resulted in 109,580 suspected cases and 11,717 reported deaths (2). In 2013, a new strain of N. meningitidis serogroup C (NmC) emerged in Nigeria, resulting in small focal outbreaks during 2014–2016 (3,4). In 2015, this strain of NmC entered neighboring Niger, resulting in the largest ever global epidemic of serogroup C meningitis (5), until the 2016–2017 Nigeria epidemic described in this report. Molecular sequencing of bacterial isolates from patients in the region has confirmed the expansion of this new strain of serogroup C in five countries in the region (Ryan Novak, National Center for Immunization and Respiratory Diseases, CDC, personal communication, 2017).
Case Definition and Incidence Thresholds for Response
A suspected case of meningitis was defined as the sudden onset of fever (>100.4°F [>38.0°C]) and at least one meningeal sign, including neck stiffness or altered consciousness in any person, or a bulging anterior fontanelle in children aged <18 months (6). Available cerebrospinal fluid (CSF) or blood specimens from patients meeting the suspected meningitis case definition were transported to a designated laboratory for confirmation by culture, latex agglutination, or real-time–polymerase chain reaction (PCR) tests. World Health Organization (WHO) Meningitis Outbreak Response Guidelines were used to identify geographic areas at risk for epidemics to guide response (6). Attack rates of suspected meningitis cases reported weekly by LGAs were calculated. WHO recommends that a set of preparedness activities be implemented when the attack rate of suspected meningitis in an LGA crosses a defined “Alert” threshold, and additional response activities at a defined “Epidemic” threshold (Table 1).
Outbreak Investigation
Two outbreak investigation teams were deployed to Zamfara and Sokoto states to augment routine surveillance, forward available CSF specimens to a designated laboratory for analysis, verify the extent of the outbreak, and gather specific information regarding the affected population to guide response. The first meningitis cases, a 21-case cluster in a village in Zurmi LGA of Zamfara State, were reported to the State Ministry of Health in December 2016; however, the cluster was not reported to NCDC until February 2017, after the outbreak had spread to four other LGAs in Zamfara, and to Katsina, Kebbi, Niger, and Sokoto states. During December 2016–June 2017, among Nigeria’s 37 state-level jurisdictions, 26 (70%) reported suspected meningitis cases, with peak incidence during reporting week 15 (April 16–22, 2017) (Figure). Meningitis incidence in 56 LGAs met the alert threshold and in 38 met the epidemic threshold. Overall, 14,518 suspected cases and 1,166 deaths (case-fatality ratio = 8.0%), were reported during the outbreak; 7,140 (49%) cases were reported from Zamfara State, and 6,792 (47%) occurred in children aged 5–14 years (Table 2). Confirmatory laboratory testing was conducted for specimens from 1,339 (9%) suspected meningitis patients; among these, 433 (32.3%) were laboratory-confirmed as bacterial meningitis, including 358 (82.7%) with NmC (Table 2).
Early Outbreak Response Activities
Following initial investigations, including health facility register reviews and analysis of community informant reports, NCDC activated the meningitis EOC on April 3, 2017 to coordinate outbreak response strategies and operations across the entire country in collaboration with country partner agencies, including WHO, CDC, the Africa Centre for Disease Control and Prevention, the United Nations Children’s Fund (UNICEF) and the Africa Field Epidemiology Network. To ensure that suspected meningitis cases were rapidly detected and investigated, meningitis surveillance, according to WHO’s Africa Region Guidelines for Enhanced Meningitis Surveillance, was strengthened in all states, regardless of whether states reported cases. EOCs were also activated to coordinate outbreak response activities in Sokoto and Zamfara states, the two states at the epicenter of the outbreak. Rapid response teams of epidemiologists and clinicians were deployed from the national EOC to support states with at least one LGA meeting the defined outbreak threshold.
Early outbreak response activities were hampered by difficulty in accessing some of the more rural and remote communities experiencing the outbreak. A limited capacity for CSF specimen collection among health care workers, deficiencies in the laboratory systems, including a lack of basic test kits and limited resources to support timely and appropriate specimen transportation from health facilities to a laboratory with PCR or culture capacity, contributed to delayed case identification. Additionally, the human resources needed to support effective outbreak detection and response were limited in some of the states with the largest case numbers, necessitating the recruitment and deployment of a large contingent of ad hoc technical support personnel from the national level to support outbreak control activities in these states.
Outbreak Response Vaccination
The National Primary Health Care Development Agency, responsible for vaccination activities in Nigeria, received meningococcal C–containing vaccines through the International Coordinating Group on Vaccine Provision in April 2017, 2 months after the outbreak was first widely reported. Because of limited vaccine supplies, vaccine use was prioritized to the most affected LGAs in Katsina, Sokoto, Yobe, and Zamfara states (6) where approximately 2.1 million (84.4%) of an estimated 2.5 million persons at risk (based on the WHO guidelines) aged 2–29 years were vaccinated. Extensive social mobilization activities, including outreach to community leaders and engagement on social and traditional media helped raise awareness and facilitate desired behavior change, including vaccine acceptance and avoidance of overcrowding, thereby reducing potential for continued transmission.
Discussion
The outbreak likely represents the largest global outbreak of NmC. Response measures implemented during the outbreak, including improved case finding and management as well as mass vaccination campaigns, might have contributed to the outbreak control. However, the large number of cases and prolonged duration of the outbreak highlight key lessons for meningitis outbreak prevention, detection, and response in Nigeria and other countries in the meningitis belt. Timely and appropriate use of meningococcal vaccines is effective in preventing and limiting the spread of meningococcal meningitis outbreaks. The introduction of the meningococcal A conjugate vaccine against NmA in Nigeria and other countries in the meningitis belt represents a major milestone in meningitis outbreak control and has contributed to significant reductions in NmA infections (7,8). However, laboratory data from this and other recent outbreaks point to the evolving regional meningitis epidemiology with increasing proportions of epidemics attributable to bacterial meningitis pathogens other than NmA, for which meningococcal A conjugate vaccine provides no protection (3,4). These findings suggest an urgent need to expand availability of multivalent vaccines that are effective against non-A serogroups.
In Nigeria, meningitis is classified as an epidemic-prone disease, requiring immediate notification, investigation, and necessary action (9); significant lapses in reporting in the early stages of this outbreak (from December 2016 to February 2017) might have contributed to its large size and wide reach. Additionally, limited capacity for CSF specimen collection, a lack of test kits, and inadequate resources to support timely and appropriate specimen transportation from health facilities to a laboratory with PCR or culture capacity contributed to the low percentage of confirmed meningitis cases. Similarly, delays in case finding, reporting and investigation, especially in the more remote areas, limited timely outbreak response. These meningitis surveillance system weaknesses merit further investigation, with remediating action implemented to prevent future reoccurrence. Because delayed access to meningococcal vaccines might have contributed to the prolonged outbreak duration, a careful examination of country vaccine requisition processes, and International Coordinating Group on Vaccine Provision protocols for vaccine requests, approval, delivery and use, is needed.
A surveillance and outbreak response system is most effective when the capacity to prevent, detect, and appropriately respond to outbreaks is available (10). In Nigeria, the human resource capacity to support an effective outbreak response varied widely within and between states, and was severely limited in some of the most at-risk states and LGAs. In low human resource capacity settings, evolving and refining new models for effective and timely outbreak detection and response, including scaling up emergency Rapid Response Team deployment where needed, is critical. In Nigeria, an opportunity exists for improved response coordination with lessons learned from EOCs established for coordination of polio eradication activities and response to Ebola virus disease, as well as leveraging trained personnel from the Nigeria Field Epidemiology and Laboratory Training Program. In the longer term, building adequate health care worker capacity at all national and subnational surveillance system levels will be essential to a timely and effective outbreak response. Functional laboratory systems are pivotal to meningitis case confirmation and provide guidance for critical outbreak response activities, including decisions on appropriate vaccine use.
With the outbreak now declared over, efforts to improve surveillance and outbreak preparedness for meningitis need to continue. Recently concluded national and regional evaluations of the outbreak response have articulated recommendations for improving meningitis outbreak prevention, timely detection, and response in Nigeria, and implementation of these recommendations is needed at all levels of the public health system. Additionally, conducting a review of the implementation of current meningitis outbreak alert and epidemic thresholds in Nigeria, including an assessment of sub-LGA–level sensitivity to outbreaks at the current thresholds could help to ensure optimal and timely detection at the lower levels. Developing and introducing conjugate vaccines effective against non-A meningococcal serogroups might help reduce the risk for future non-serogroup A meningococcal meningitis outbreaks.
Corresponding author: Chimeremma Nnadi, wgq4@cdc.gov, 404-906-63
References
- World Health Organization. Meningococcal meningitis. Fact sheet. Geneva, Switzerland: World Health Organization; 2017. http://www.who.int/mediacentre/factsheets/fs141/en/
- Mohammed I, Nasidi A, Alkali AS, et al. A severe epidemic of meningococcal meningitis in Nigeria, 1996. Trans R Soc Trop Med Hyg 2000;94:265–70. CrossRef PubMed
- Chow J, Uadiale K, Bestman A, et al. Invasive meningococcal meningitis serogroup C outbreak in northwest Nigeria, 2015—third consecutive outbreak of a new strain. PLoS Curr 2016;8:8. PubMed
- Funk A, Uadiale K, Kamau C, Caugant DA, Ango U, Greig J. Sequential outbreaks due to a new strain of Neisseria meningitidis serogroup C in northern Nigeria, 2013–14. PLoS Curr 2014;6:6. PubMed
- Sidikou F, Zaneidou M, Alkassoum I, et al. Emergence of epidemic Neisseria meningitidis serogroup C in Niger, 2015: an analysis of national surveillance data. Lancet Infect Dis 2016;16:1288–94. CrossRef PubMed
- World Health Organization. Meningitis outbreak response in sub-Saharan Africa. WHO guideline. Geneva, Switzerland: World Health Organization; 2014. http://www.who.int/csr/resources/publications/meningitis/guidelines2014/en/
- Trotter CL, Lingani C, Fernandez K, et al. Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–15: an analysis of surveillance data. Lancet Infect Dis 2017;17:867–72. CrossRef PubMed
- Sambo L, Chan M, Davis S, et al. A vaccine meets its promise: success in controlling epidemic meningitis in sub-Saharan Africa. Clin Infect Dis 2015;61(Suppl 5):S387–8. CrossRef PubMed
- Nigeria Centre for Disease Control. Technical guidelines for integrated disease surveillance and response in Nigeria. Abuja, Nigeria: Nigeria Centre for Disease Control; 2016. http://www.ncdc.gov.ng/themes/common/docs/protocols/4_1476085948.pdf
- Lo TQ, Marston BJ, Dahl BA, De Cock KM. Ebola: anatomy of an epidemic. Annu Rev Med 2017;68:359–70. CrossRef PubMed
 TABLE 1. Guidelines for incidence thresholds and interventions for detection and control of epidemic meningococcal meningitis based on population size of the local government area in countries in Africa with endemic disease* — World Health Organization
TABLE 1. Guidelines for incidence thresholds and interventions for detection and control of epidemic meningococcal meningitis based on population size of the local government area in countries in Africa with endemic disease* — World Health Organization
| Incidence threshold | Population size | Interventions | |
|---|---|---|---|
| <30,000 | 30,000–100,000 | ||
| Alert | Two suspected cases in 1 week or increase in incidence compared with nonepidemic years | Three suspected cases per 100,000 population per week (two or more cases in 1 week) | 1) Inform authorities, 2) strengthen surveillance, 3) investigate, 4) confirm (including laboratory), 5) treat cases, 6) prepare for eventual response |
| Epidemic | Five suspected cases in 1 week† or doubling of number of cases in a 3-week period | 10 suspected cases per 100,000 population per week | 1) Conduct mass vaccination§ within 4 weeks of crossing epidemic threshold, 2) distribute treatment to health centers, 3) treat according to epidemic protocol, 4) inform the public |
* Guidelines adapted from http://apps.who.int/iris/handle/10665/144727.
† In special situations such as mass gatherings, refugees, displaced persons or closed institutions, two confirmed cases in a week should prompt mass vaccination.
§ If an area neighboring one targeted for vaccination is considered to be at risk (e.g., cases early in the dry season, no recent relevant vaccination campaign, or high population density), it should be included in a vaccination program.
NTSB: The Amtrak train that derailed Monday in Washington state was traveling 80 mph in a 30 mph zone
Tuesday, December 19th, 2017- The passenger train had run off the tracks, killing at least three and injuring more than 100 others
There are now 174 cases of Candida auris infections in the United States, 17 more than the CDC reported last month.
Tuesday, December 19th, 2017December 15, 2017: Case Count Updated as of November 30, 2017
Candida auris is an emerging fungus that presents a serious global health threat. C. auris causes severe illness in hospitalized patients in several countries, including the United States. Patients can remain colonized with C. auris for a long time and C. auris can persist on surfaces in healthcare environments. This can result in spread of C. auris between patients in healthcare facilities.
Most C. auris cases in the United States have been detected in the New York City area and New Jersey. Strains of C. auris in the United States have been linked to other parts of the world. U.S. C. auris cases are a result of inadvertent introduction into the United States from a patient who recently received healthcare in a country where C. auris has been reported or a result of local spread after such an introduction.
U.S. Map: Clinical cases of Candida auris reported by state, United States, as of November 30, 2017
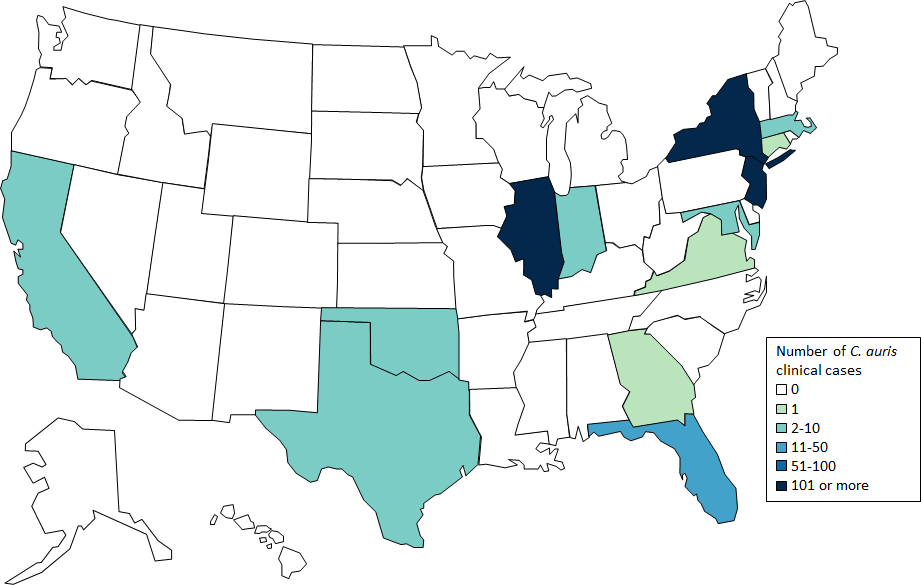 Cases are categorized by the state where the specimen was collected. Most probable cases were identified when laboratories with current cases of C. auris reviewed past microbiology records for C. auris. Isolates were not available for confirmation. Early detection of C. auris is essential for containing its spread in healthcare facilities.
Cases are categorized by the state where the specimen was collected. Most probable cases were identified when laboratories with current cases of C. auris reviewed past microbiology records for C. auris. Isolates were not available for confirmation. Early detection of C. auris is essential for containing its spread in healthcare facilities.
Table: Clinical cases of Candida auris reported by state, United States, as of November 30, 2017
| State | Number and type of clinical Candida auris cases reported | |
|---|---|---|
| Confirmed | Probable | |
| California | 1 | 0 |
| Connecticut | 1 | 0 |
| Florida | 2 | 0 |
| Illinois | 12 | 2 |
| Indiana | 1 | 0 |
| Maryland | 2 | 0 |
| Massachusetts | 6 | 0 |
| New Jersey | 38 | 23 |
| New York | 110 | 4 |
| Oklahoma | 1 | 0 |
| TOTAL | 174 | 29 |
Beyond the clinical case counts reported above, an additional 257 patients have been found to be colonized with C. auris by targeted screening in four states with clinical cases.
CDC encourages all U.S. laboratories that identify C. auris to notify their state or local public health authorities and CDC at candidaauris@cdc.gov. CDC is working closely with public health and healthcare partners to prevent and respond to C. auris infections. The CDC-sponsored Antibiotic Resistance Laboratory Network (ARLN) will help improve detection and response to C. auris nationwide.
Countries from which Candida auris cases have been reported, as of November 30, 2017
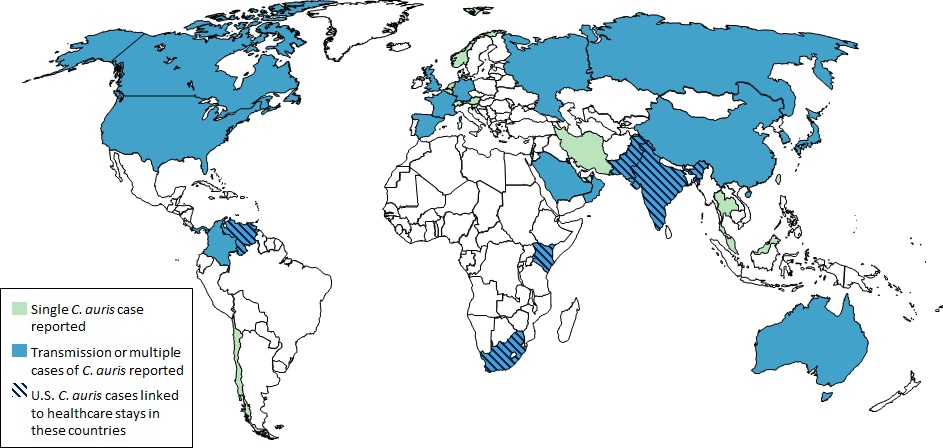
- Single cases of C. auris have been reported from Germany, Japan, Kuwait, and Norway.
- Multiple cases of C. auris have been reported from Canada, Colombia, India, Israel, Kenya, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Kingdom, the United States (primarily from New York City Metropolitan Area and New Jersey) and Venezuela; in some of these countries, extensive transmission of C. auris has been documented in more than one hospital.
- U.S. cases of C. auris have been found in patients who had recent stays in healthcare facilities in India, Pakistan, South Africa and Venezuela, which also have documented transmission.
- Other countries not highlighted on this map may also have undetected or unreported C. auris cases.
The train rounded a curve when it began to wobble and then it fell on its side. Six dead so far;
Monday, December 18th, 2017https://www.youtube.com/watch?v=KT3HKiJRuME
The rape of Rohingya women by Myanmar’s security forces
Monday, December 18th, 2017“…..The AP interviewed 29 women and girls who say they were raped by Myanmar’s armed forces, and found distinct patterns in their accounts, their assailants’ uniforms and the details of the rapes themselves. The most common attack involved groups of soldiers storming into a house, beating any children inside and then beating and gang raping the women. ….”
The death of a patient from septicemic plague in China
Monday, December 18th, 2017“…..The patient, a herder from Jiuquan’s Subei Mongolian autonomous county, died on Tuesday afternoon despite efforts by medical personnel……. The patient’s gender was not disclosed.
Experts said tests had confirmed at 11 pm that the patient died of septicemic plague that evolved from bubonic plague, which was reported as a suspected plague case at 5:30 pm.
Authorities said they had placed 12 people who had close contact with the patient under quarantine, and no abnormalities had been found……”



 * Reporting week 15 corresponds to April 16–22, 2017; week 21 corresponds to June 4–10, 2017.
* Reporting week 15 corresponds to April 16–22, 2017; week 21 corresponds to June 4–10, 2017.