Objectives
To study the associations between Influenza like illness (ILI) and socioeconomic status (SES), gender and wave during the 1918-19 influenza pandemic.
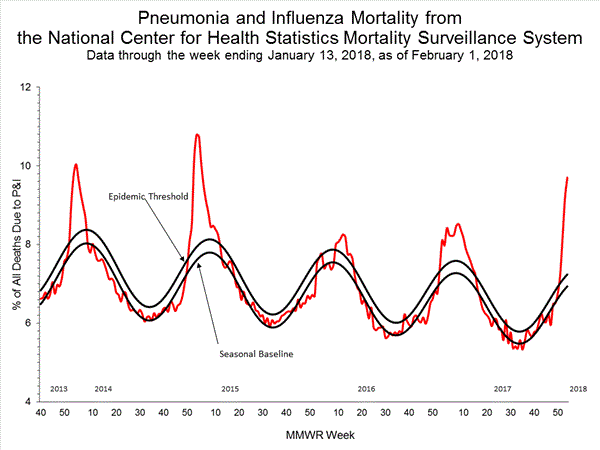
During week 4 (January 21-27, 2018), influenza activity increased in the United States.
Seventeen influenza-associated pediatric deaths were reported to CDC during week 4.
Five deaths were associated with an influenza A(H3) virus and occurred during weeks 1, 2, 3, and 4 (the weeks ending January 6, January 13, January 20, and January 27, 2018). Two deaths were associated with an influenza A(H1N1)pdm09 virus and occurred during weeks 3 and 4 (the weeks ending January 20, 2018, and January 27, 2018, respectively). Four deaths were associated with an influenza A virus for which no subtyping was performed and occurred during weeks 3 and 4. Five deaths were associated with an influenza B virus and occurred during weeks 1, 3, and 4 (the week ending January 6, January 20, and January 27, 2018, respectively).
A total of 53 influenza-associated pediatric deaths have been reported for the 2017-2018 season.
One death that occurred during the 2015-2016 season was associated with an influenza A virus for which no subtyping was performed and occurred during week 28 (the week ending July 16, 2016). This death brings the total number of reported influenza-associated deaths occurring during that season to 93.
The Influenza Hospitalization Surveillance Network (FluSurv-NET) conducts population-based surveillance for laboratory-confirmed influenza-related hospitalizations in children younger than 18 years of age (since the 2003-2004 influenza season) and adults (since the 2005-2006 influenza season).
The FluSurv-NET covers more than 70 counties in the 10 Emerging Infections Program (EIP) states (CA, CO, CT, GA, MD, MN, NM, NY, OR, and TN) and additional Influenza Hospitalization Surveillance Project (IHSP) states. The IHSP began during the 2009-2010 season to enhance surveillance during the 2009 H1N1 pandemic. IHSP sites included IA, ID, MI, OK and SD during the 2009-2010 season; ID, MI, OH, OK, RI, and UT during the 2010-2011 season; MI, OH, RI, and UT during the 2011-2012 season; IA, MI, OH, RI, and UT during the 2012-2013 season; and MI, OH, and UT during the 2013-2014, 2014-15, 2015-16, 2016-17, and 2017-18 seasons.
Data gathered are used to estimate age-specific hospitalization rates on a weekly basis, and describe characteristics of persons hospitalized with influenza illness. The rates provided are likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications.
A total of 14,676 laboratory-confirmed influenza-associated hospitalizations were reported between October 1, 2017 and January 27, 2018. The overall hospitalization rate was 51.4 per 100,000 population. The highest rate of hospitalization was among adults aged ≥65 years (226.8 per 100,000 population), followed by adults aged 50-64 (54.0 per 100,000 population) and children aged 0-4 years (33.3 per 100,000 population). Among 14,676 hospitalizations, 12,849 (87.5%) were associated with influenza A virus, 1,762 (12.0%) with influenza B virus, 35 (0.2%) with influenza A virus and influenza B virus co-infection, and 30 (0.2%) with influenza virus for which the type was not determined. Among those with influenza A subtype information, 2,797 (86.5%) were A(H3N2) and 437 (13.5%) were A(H1N1)pdm09 virus.
Among 1,708 hospitalized adults with information on underlying medical conditions, 1,183 (69.3%) had at least one reported underlying medical condition; the most commonly reported were cardiovascular disease, metabolic disorder, obesity, and chronic lung disease. Among 180 hospitalized children with information on underlying medical conditions, 93 (51.7%) had at least one underlying medical condition; the most commonly reported were asthma, neurologic disorder, and obesity. Among 138 hospitalized women of childbearing age (15-44 years) with information on pregnancy status, 33 (23.9%) were pregnant.
Nationwide during week 4, 7.1% of patient visits reported through the U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) were due to influenza-like illness (ILI). This percentage is above the national baseline of 2.2%.(ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.)
Additional ILINet data, including national, regional and select state-level data, are available at http://gis.cdc.gov/grasp/fluview/fluportaldashboard.html.
On a regional level, the percentage of outpatient visits for ILI ranged from 2.8% to 13.0% during week 4. All 10 regions reported percentages of outpatient visits for ILI at or above their region specific baselines.
“….As reported from Australia for the 2017 southern hemisphere vaccine, interim estimates from Canada for the 2017/18 northern hemisphere vaccine indicate low VE of less than 20% against influenza A(H3N2), notably among working-age adults. While the influenza A(H3N2) epidemic continues, adjunct protective measures should be reinforced to minimise the associated disease burden in high-risk individuals….”
“…..The CDC plans to narrow its focus to 10 “priority countries,” starting in October 2019, the official said. They are India, Thailand and Vietnam in Asia; Jordan in the Middle East; Kenya, Uganda, Liberia, Nigeria and Senegal in Africa; and Guatemala in Central America.
Countries where the CDC is planning to scale back include some of the world’s hot spots for emerging infectious disease, such as China, Pakistan, Haiti, Rwanda and Congo……”
“…..The health care plan, part of the government’s 2018-19 budget presented on Thursday, would offer 100 million families up to 500,000 rupees, or about $7,860, of coverage each year. That sum, while small by Western standards, would be enough to cover the equivalent of five heart surgeries in India…..”
1918 H1N1 influenza virus replicates and induces pro-inflammatory cytokine responses in extra-respiratory tissues of ferrets.
The Journal of Infectious Diseases, jiy003, https://doi.org/10.1093/infdis/jiy003
Published: 10 January 2018
“….1918 H1N1 virus spread to, and induced cytokine responses in tissues outside the respiratory tract, which likely contributed to the severity of infection. Moreover, our data support the suggested link between 1918 H1N1 infection and CNS disease.….”
Mamelund, S.-E. (), 1918 pandemic morbidity: the first wave hits the poor, the second wave hits the rich. Influenza Other Respi Viruses. Accepted Author Manuscript. doi:10.1111/irv.12541
To study the associations between Influenza like illness (ILI) and socioeconomic status (SES), gender and wave during the 1918-19 influenza pandemic.
Availability of incidence data on the 1918-19 pandemic is scarce, in particular for waves other than the “fall wave” October-December 1918. Here, an overlooked survey from Bergen, Norway (n=10,633), is used to study differences in probabilities of ILI and ILI probability ratios by apartment size as a measure of SES and gender for three waves including the waves prior to and after the “fall wave”.
SES was negatively associated with ILI in the first wave, but positively associated in the second wave. At all SES levels, men had the highest ILI in the summer, while women had the highest ILI in the fall. There were no SES or gender differences in ILI in the winter of 1919.
For the first time it is documented a crossover in the role of socioeconomic status in 1918 pandemic morbidity. The poor came down with influenza first, while the rich with less exposure in the first wave had the highest morbidity in the second wave. The study suggest that socioeconomically disadvantaged should be prioritized if vaccines are of limited availability in a future pandemic.