Archive for August, 2018
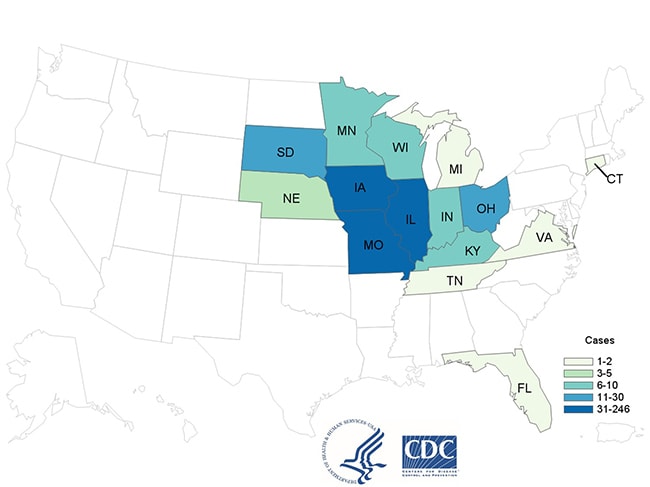
CDC: 40 more cases in a Cyclospora outbreak linked to McDonald’s salads, pushing the illness total to 476.
Saturday, August 18th, 2018DRC: As of 15 August 2018, 78 EVD cases (51 confirmed and 27 probable), including 44 deaths, have been reported.
Saturday, August 18th, 2018Ebola virus disease – Democratic Republic of the Congo
On 1 August 2018, the Ministry of Health (MoH) of the Democratic Republic of the Congo declared a new outbreak of Ebola virus disease (EVD) in the town of Mangina, Mabalako Health Zone, North Kivu Province. Confirmed cases have since between reported from Beni and Mandima health zones, Ituri Province; however, all confirmed exposures and transmission events to date have been linked back to the outbreak epi-centre, Mangina. North Kivu and Ituri are among the most populated provinces in the country, share borders with Uganda and Rwanda, and experience conflict and insecurity, with over one million internally displaced people and migration of refugees to neighbouring countries.
As of 15 August 2018, 78 EVD cases (51 confirmed and 27 probable), including 44 deaths, have been reported.1 Since the DON published on 9 August, 34 new confirmed cases have been reported: seven from Ituri Province (Mandima Health Zone) and 27 from North Kivu Province (one in Beni and 26 in Mabalako health zones). The 78 confirmed or probable cases reside in five health zones in North Kivu and one health zone in Ituri. The majority of cases (39 confirmed and 21 probable) have been reported from Mangina in Mabalako Health Zone (Figure 1). As of 15 August, 24 suspected cases are currently pending laboratory testing to confirm or exclude EVD.
Eight new confirmed cases among health care workers have been reported, bringing the total number of infected health care workers to 10 (nine confirmed and one probable deceased case). These health care workers were likely exposed in clinics, not Ebola treatment centres (ETCs), many of which may have been infected before the declaration of the outbreak. WHO and partners are working to increase awareness of Ebola among health care and other frontline workers, and to strengthen infection prevention and control (IPC) measures.
The MoH, WHO and partners continue to systematically monitor and rapidly investigate all alerts in other provinces and in neighbouring countries. Since the last DON was published, alerts in several provinces of the Democratic Republic of Congo as well as in Uganda, Rwanda, and the Central African Republic were investigated; EVD was ruled out for all.
For more information, see:

ublic health response
The MoH rapidly initiated response mechanisms in North Kivu and Ituri provinces with support from WHO and partners. Priorities include the establishment and strengthening of surveillance, contact tracing, laboratory capacity, IPC, clinical management, vaccination, risk communication and community engagement, safe and dignified burials, response coordination, cross-border surveillance, and preparedness activities in neighbouring provinces and countries.
- During a two-day mission to the outbreak epi-centre, the WHO Director-General (DG), WHO Regional Director (RD) for Africa and WHO Deputy Director-General (DDG), Emergency Preparedness and Response, together with the Minister of Health, observed the launch of Ebola vaccination activities, visited the Emergency Operations Centre (EOC), met with partners and staff to discuss the challenges ahead, and assessed response measures and needs.
- The WHO DG and the RD then visited Uganda where they were briefed by the WHO Representative on the country’s EVD preparedness. The DG and RD later met the Uganda Prime Minister, the Minister of Foreign Affairs, the Minister of Health, and the Minister of State for Primary Health Care to discuss EVD preparedness and WHO support.
- The MoH has activated a multi-partner incident management system and an EOC to coordinate the response, with the main centre in Beni and the field coordination centre in Mangina. WHO has established an incident management team with personnel from the WHO Country Office, Regional Office for Africa and headquarters who are collaborating closely to ensure a comprehensive and effective response to the outbreak.
- On 8 August, the MoH, with support from WHO and partners, launched the Ebola ring vaccination activities for high-risk populations. In the first days, health care and other frontline workers were vaccinated. As of 15 August, a total of five rings have been defined around 13 recently confirmed cases. Within these initial rings, more than 500 contacts and their contacts consented and received rVSV-ZEBOV Ebola vaccine thus far. Teams are continuing to identify and vaccinate all eligible contacts to help interrupt transmission of the virus.
- The MoH and WHO continue to strengthen surveillance in the affected and surrounding areas. As of 15 August, nearly 1600 contacts, including more than 120 health workers, in North Kivu and Ituri provinces have been registered and are being followed up on daily basis.
- As of 15 August, WHO has deployed over 100 technical and logistics specialists to support response activities. Global Outbreak Alert and Response Network (GOARN) partner institutions continue to support the response as well as ongoing readiness and preparedness activities in non-affected provinces of the Democratic Republic of the Congo and in bordering countries. For more information about operational readiness and preparedness activities, please see the DON published on 14 August.
- In addition to the mobile laboratory established in Beni on 3 August, local testing with Xpert Ebola has since been established in hospital facilities in Beni, Goma, and Mangina to facilitate the timely diagnosis of suspected cases.
- The Alliance for International Medical Action (ALIMA) and Médecins Sans Frontières (MSF) have established 60-bed ETCs in Beni and Mangina, respectively. The partners are preparing the ETCs to provide therapeutics under the monitored emergency use of unregistered and experimental interventions (MEURI) protocol in collaboration with MoH and Institut National de Recherche Biomédicale (INRB). WHO is providing technical expertise support on site and assisting with the creation of a data safety management board.
- The MoH team, with support from UNICEF, are training 90 psychosocial agents to provide psychosocial care to patients and other affected people.
- Knowledge, Attitude and Practice (KAP) surveys were conducted in Beni and Mabalako health zones to assess the levels of EVD awareness in the communities. Findings from the survey will be used to improve the risk communication, social mobilization and community engagement strategy.
- Two planes with supplies of cold chain equipment, isolation units and vehicles arrived in Beni on 11 and 12 August.
WHO risk assessment
This latest outbreak of EVD is affecting north-eastern provinces of the Democratic Republic of the Congo which border Uganda. Potential risk factors for transmission of EVD at the national and regional levels include the transportation links between the affected areas, the rest of the country, and neighbouring countries; the internal displacement of populations; and displacement of Congolese refugees to neighbouring countries. The country is concurrently experiencing several epidemics and a long-term humanitarian crisis. Additionally, the security situation in North Kivu and Ituri may hinder the implementation of response activities. Based on this context, the public health risk was assessed to be high at the national and regional levels, and low globally.
WHO advice
The Strategic Advisory Group of Experts (SAGE) working group on Ebola vaccines and the SAGE members have reviewed the epidemiological situation and the evidence available with regard to the different candidate Ebola vaccines and the impact of different interventions. While ring vaccination remains the preferred strategy (as stated in the April 2017 SAGE report, a geographic targeted approach was proposed as an exceptional alternative if the ring vaccination around a laboratory-confirmed case of Ebola proves unfeasible. The following interim recommendation was agreed upon: “Should an Ebola disease outbreak occur before the candidate vaccine is licensed, SAGE recommended that the rVSV-ZEBOV Ebola vaccine be promptly deployed under the Expanded Access framework, with informed consent and in compliance with Good Clinical Practice. If the outbreak is caused by an Ebola virus species other than Zaire, consideration should be given to the use of other candidate vaccines that target the putative viral species”.
For more information, see:
As investigations continue to establish the full extent of this outbreak and the risk of national and regional spread remains high, it is important for neighbouring provinces and countries to enhance surveillance and preparedness activities. WHO will continue to work with neighbouring countries and partners to ensure health authorities are alerted and are operationally ready to respond.
WHO advises against any restriction of travel and trade to the Democratic Republic of the Congo based on the currently available information. WHO continues to closely monitor and, if necessary, verify travel and trade measures in relation to this event.
For more information, see:
- WHO recommendations for international travellers
- – Ebola virus disease in the Democratic Republic of the Congo – Operational readiness and preparedness in neighbouring countries
- Ebola virus disease fact sheet
1The number of cases is subject to change due to ongoing reclassification, retrospective investigation, and the availability of laboratory results.
NYPD SHIELD
Saturday, August 18th, 2018INTRODUCTION
New York City has been targeted by terrorists on several occasions, most notably the 1993 and 2001 attacks against the World Trade Center.
Other plots have been thwarted, such as the attempt to bomb the Atlantic Avenue subway station in 1997 and the 1993 Landmarks plot that targeted key sites, such as the Lincoln and Holland Tunnels, the United Nations and 26 Federal Plaza. New York has persevered and thrived in the face of these events, but we cannot let our guard down. The threat of terrorism remains. Working together, the public and private sectors are stronger than either is alone. This partnership is the cornerstone in defending the City against terrorism.
NYPD SHIELD is an umbrella program for a series of current and future Police Department initiatives that pertain to private sector security and counterterrorism. This is a public private partnership based on information sharing.
NYPD SHIELD is a central destination for private sector security managers to obtain information and engage Police Department resources.
NYPD SHIELD also seeks information from our private sector partners to assist in our efforts to keep the City safe.
WHAT WE DO
NYPD SHIELD addresses private sector business on both an industry-specific and a geographic basis. This enables the NYPD to best serve the unique needs of each constituency. NYPD provides training services to assist public and private sector entities in defending against terrorism.
In addition, information specific to a particular sector or neighborhood is transmitted directly to those affected by one of several methods:
- In-person intelligence and threat briefings conducted by Counterterrorism Bureau and Intelligence Division personnel
- Informal conferrals with Patrol Borough Counterterrorism Coordinators
- NYPD Website postings
- Shield Alert e-mail messages
NYPD SHIELD keeps our private sector partners informed of developing situations in the City, preparations for upcoming events and new intelligence and threat information.
WHAT WE ASK
NYPD SHIELD is a two-way street; the key to success is for information to flow in two directions. Private sector personnel are well situated to serve as eyes and ears of the NYPD. We ask your assistance in the fight against terrorism by reporting suspicious behavior as soon as possible.
In addition, we recognize that our private sector partners are uniquely qualified to assist NYPD personnel during counterterrorism deployments. Your personnel know your buildings, blocks and neighborhoods from a different perspective. You know what belongs and what is out of place. We urge you and your staff to speak with the police officers you see on the street, particularly those assigned to posts in the vicinity of sensitive and critical locations. Sharing your perspective can help us be more effective. If you have information to pass to the NYPD but cannot do so in person, please use our 24-hour hotline, 1-888-NYC-SAFE or 311. In an emergency, always call 911.
India, 2016: Severe Manifestations of Chikungunya Fever in Kids
Saturday, August 18th, 2018“……A total of 49 children had chikungunya fever; 36 had nonsevere disease and 13 had severe disease. All patients with severe disease were admitted to the PICU; 11 had illness consistent with the case definition of severe sepsis and septic shock, and 2 had acute liver failure. Of the 36 patients with nonsevere disease, 16 were admitted to the PICU (11 had seizures, 4 had fluid-responsive shock, 1 had peripheral cyanosis and mottling) and 20 were admitted to the pediatric high-dependency unit (3 had bleeding manifestations, 4 had severe abdominal pain, 2 had underlying cyanotic congenital heart disease, 2 had body temperature >40.3°C with irrelevant talking, 7 had dehydration, and 2 had severe rash). The median age was 12 years for patients with severe disease and 6.5 years for patients with nonsevere disease; male sex predominated in both groups (Table). Frequency of fever, body ache, arthralgia, and vomiting were similar for both groups. Peripheral cyanosis, along with mottling of skin and encephalopathy, was significantly higher in the group with severe disease. Serum albumin was significantly lower in the group with severe disease (3 vs. 3.75 g/dL). Of the 11 children with septic shock, 8 were admitted to the hospital within 24 hours of developing fever; 9 had hypotensive shock, and 2 had compensated shock. In this group, 6 children required 1 vasoactive agent, 3 children required 2 vasoactive agents, and 2 children required 3 vasoactive agents. Dopamine was used in 8 patients, dobutamine in 5 patients, epinephrine in 2 patients, and norepinephrine in 2 patients. The median duration of vasoactive support was 56 hours (range 31–114 hours), and the median vasoactive inotropic score in the first 24 hours was 10 (range 5–90; score >15–20 is considered serious). A vasoactive inotropic score >20 was seen in 2 children. Mean pH was 7.26 (reference range 7.35–7.45), mean lactate 5.1 mmol/L (reference range <2 mmol/L), mixed venous saturation 55% (reference range 70%–80%), and mean base excess at admission –7.7 mEq (reference range –2 to 2 mEq). Of the 2 children with acute liver failure with encephalopathy, 1 had dengue virus (positive dengue IgM by enzyme immunoassay) and the other had hepatitis E virus (reactive anti–hepatitis E IgM by enzyme immunoassay) co-infection…..”
| Sharma PK, Kumar M, Aggarwal GK, Kumar V, Srivastava R, Sahani A, et al. Severe Manifestations of Chikungunya Fever in Children, India, 2016. Emerg Infect Dis. 2018;24(9):1737-1739. https://dx.doi.org/10.3201/eid2409.180330
|
Floods in the southern state of Kerala in India have left more than 320 people dead and more than 220,000 displaced.
Friday, August 17th, 20188/17/1999: More than 17,000 people are killed with damages totaling $6.5 billion in a 7.4M earthquake in Turkey
Friday, August 17th, 2018https://www.youtube.com/watch?v=bgGB0rlPlWs
Lassa Fever: 9 new confirmed cases were reported from three different states in Nigeria
Friday, August 17th, 2018In the reporting Week 31 (July 30-August 5, 2018) nine new confirmedi cases were reported from Edo(7), Ondo(1) and Enugu(1) with two new deaths from Edo(1) and Enugu (1)
Enugu state recorded the first confirmed case in the state since the beginning of the outbreak with death in the confirmed case From 1st January to 5th August 2018, a total of 2334 suspected cases have been reported from 22 states. Of these, 481 were confirmed positive, 10 are probable, 1844 negative (not a case)
Since the onset of the 2018 outbreak, there have been 123 deaths in confirmed cases and 10 in probable cases.
Case Fatality Rate in confirmed cases is 25.6%
In the reporting week 31, no new healthcare worker was infected. Thirty-nine health care workers have been affected since the onset of the outbreak in seven states
A total of 6383 contacts have been identified from 22 states. Of these 439(6.9%) are currently being followed up, 5846 (91.6%) have completed 21 days follow up while 10(0.2%) were lost to follow up. 88 (1.4%) symptomatic contacts have been identified, of which 30 (34%) have tested positive from five states
Lassa fever national multi-partner, multi-agency Technical Working Group(TWG) continues to coordinate response activities at all levels
Red Tide & Florida: NOAA
Thursday, August 16th, 2018NEW: Summer 2018 Red Tide Event Affecting the West Coast of Florida
What is happening?
An unusually persistent harmful algal bloom (red tide) is currently affecting portions of the southwest coast of Florida. For the latest updates on this event, visit the Florida Fish and Wildlife Conservation Commission red tide status website or the NOAA Harmful Algal Bloom Bulletin.
How long will this red tide last?
If and when bloom the current bloom will end remains an open-ended question. Red tides can last as little as a few weeks or longer than a year. They can even subside and then reoccur. In 2005, for example, a bloom started off the coast of St. Petersburg, Florida, in January and then spread from there to Pensacola and Naples by October, persisting for the majority of the year. The duration of a bloom in nearshore Florida waters depends on physical and biological conditions that influence its growth and persistence, including sunlight, nutrients, and salinity, as well as the speed and direction of wind and water currents. Researchers are watching oceanographic conditions in the region carefully and using forecasting tools similar to seasonal weather forecasts to predict how long this bloom will last.
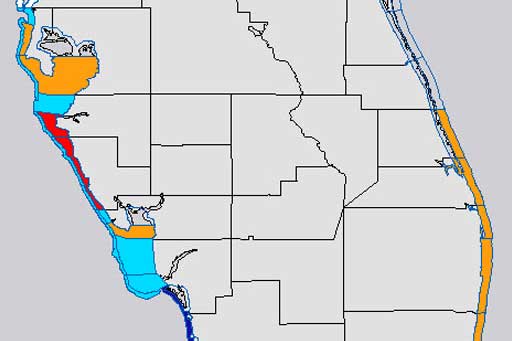
What is NOAA’s role in responding to this red tide event?
NOAA conducts scientific research and provides forecasts to give communities advance warnings to better deal with the adverse environmental impacts, health effects and economic losses associated with red tide and other harmful algal bloom events.
NOAA monitors conditions year round and provides official forecasts for red tide through two main products: conditions reports and bulletins. The conditions report identifies if red tide cell concentrations are present and provides forecasts of the highest potential level of respiratory irritation over the next three to four days. Bulletins provide decision-makers with a more in-depth analysis of the location of a current bloom and reported impacts, as well as forecasts of potential development, intensification, transport, and associated impacts of blooms. Both products are updated twice weekly during a bloom.
In addition, NOAA and a network of trained and authorized professionals from state and local organizations work together to respond to stranded marine animals found along the coastline during these events.
Can this red tide event be stopped?
There are currently no means of controlling the occurrence of red tide.
Is this red tide dangerous?
The Florida red tide organism, Karenia brevis, produces potent neurotoxins, called brevetoxins, that can affect the central nervous system of many animals, causing them to die. That is why red tides are often associated with fish kills. Mortalities of other species, including manatees, dolphins, sea turtles, and birds also occur.
Wave action near beaches can break open K. brevis cells and release the toxins into the air, leading to respiratory irritation. For people with severe or chronic respiratory conditions, such as emphysema or asthma, red tide can cause serious illness. People with respiratory problems should avoid affected beaches during red tides.
Red tide toxins can also accumulate in filter-feeders mollusks such as oysters and clams, which can lead to Neurotoxic Shellfish Poisoning (NSP) in people who consume contaminated shellfish. While not fatal, NSP causes diarrhea and discomfort for about three days. Rigorous state monitoring of cells and toxins is conducted to close commercial shellfish harvesting if necessary to protect human health. Recreational shellfish harvesters should check State web pages to make sure it is safe to consume shellfish.
Is it still safe to go to the beach?
Some areas may be more affected than others. Check NOAA forecasts to assist in locating unaffected areas, and learn more about red tide health concerns from Florida Health.
Is this normal?
This year’s bloom is different from what we’ve seen before in several ways:
Timing: Blooms of this alga typically start in late summer or early fall. The last large early summer bloom was in 2005. The current bloom started last fall and is still going.
Duration: While not unprecedented in its duration, this bloom is unusually persistent. It started in October 2017 and continued through spring of 2018. By early summer, the bloom resurged and was detected in five southwest Florida counties. Some shellfish harvesting areas have been closed since November 2017.
Size: The size of the bloom changes from week to week, and it is patchy. Not every beach is affected every day, so it is important to stay up to date with the NOAA conditions report. As of August 15, the bloom stretched from Pinellas County to Collier County, more than 150 miles.
While the timing, duration, and size of this red tide are unusual, red tides are not new to the Gulf Coast. Red tides were documented in the southern Gulf of Mexico as far back as the 1700s and along Florida’s Gulf coast in the 1840s. Fish kills near Tampa Bay were even mentioned in the records of Spanish explorers. For more information on historical red tide events in Florida, see the Florida Fish and Wildlife Conservation Commission’s harmful algal bloom monitoring database.
What do you do if you see sick, injured, stranded, or dead wildlife?
If you see sick, injured, or stranded wildlife, such as a sea turtle, manatee, dolphin, seabird, or a large fish kill in Florida, report it to the following standing network hotlines. To report an injured, hooked, entangled, or stranded sea turtle, call 1-877-942-5343. To report other sick or injured wildlife and fish kills, contact FWC Wildlife Alert or call 888-404-FWCC (888-404-3922). If you see dead or injured marine mammals, call 1-877-WHALE HELP (1-877-942-5343). You can also report via the Dolphin and Whale 911 Phone App.
What is the projected effect of this red tide on marine life? How long will it take for impacted marine life to recover?
There is no way to project the cumulative effects of this red tide event. Red tide occurs naturally in coastal waters of the Gulf of Mexico with blooms appearing seasonally. Although the Florida red tide organism, Karenia brevis, typically blooms between August and December, blooms often deviate from that time frame. The current bloom continues to be monitored by our local and state partners. Visit the Florida Fish and Wildlife Conservation Commission’s (FWC) red tide status page. Reports of fish kills and marine animal deaths are made publicly available on FWC’s website. For more information on the effects of red tide on marine animals, shellfish, and people, visit our health information page for more information.
Can NOAA provide travel advice for people planning to visit this region?
While NOAA provides regional harmful algal bloom forecasts and supports research to better understand the causes, impacts, and effects of these events, we are not in a position to provide travel advice. We have provided links to Florida state resources in the right column of this announcement that we hope will help people make informed decisions about their travel plans.
Resources for More Information:
NOAA Resources
- Gulf of Mexico Harmful Algal Bloom Forecast: NOAA’s Red Tide Bulletins are issued twice weekly during a red tide event.
- General information and resources about harmful algal blooms: NOAA portal with links to educational information about harmful algal blooms.
- Harmful Algal Bloom Detection and Resources: NOAA National Centers for Coastal Ocean Science projects, news, products, data, and general information related to harmful algal blooms.
- What is a red tide?: View our infographics to learn about red tide and NOAA harmful algal bloom forecasting.
Florida Resources
- Algal Bloom Monitoring and Support: Consolidated site from Florida Department of Environmental Protection portal for all Florida algal bloom resources.
- Red Tide Blooms: Florida Department of Health Red Tide Information
- Fish and Wildlife Research Institute Red Tide Resources: Red tide status, frequently asked questions, tools for tracking red tides, and general information from Florida Fish and Wildlife Conservation Commission
- Aquatic Toxins: Poison Control Center: Resources on aquatic toxins, to include Florida red tide, from Florida’s Poison Control Center.
- Visitbeaches.org: Mote Marine Lab’s Beach Conditions Report & Red Tide Information
General Information about Red Tide and NOAA’s Role in HAB Forecasting
What is red tide?
Harmful algal blooms occur nearly every summer along the nation’s coasts. Often, the blooms turn the water a deep red. While many people call all such events “red tides,” scientists prefer the term harmful algal bloom or HAB. A red tide or HAB results from the rapid growth of microscopic algae. Some produce toxins that have harmful effects on people, fish, marine mammals, and birds. In Florida and Texas, this is primarily caused by the harmful algae species Karenia brevis. Red tide can result in varying levels of eye and respiratory irritation for people, which may be more severe for those with preexisting respiratory conditions (such as asthma). The blooms can also cause large fish kills and discolored water along the coast.

Red Tide in Florida and Texas
Red Tide in Florida and Texas is caused by the rapid growth of a microscopic algae called Karenia brevis. When large amounts of this algae are present, it can cause a harmful algal bloom (HAB) that can be seen from space. NOAA issues HAB forecasts based on satellite imagery and cell counts of Karenia brevis collected in the field and analyzed by NOAA partners. | Transcript
How Does the NOAA Forecast Work?
NOAA uses a combination of satellite imagery and water samples of the algae species Karenia brevis, collected from the field by local partners, to forecast the location and intensity of red tide events. Satellite imagery is a key tool for detecting blooms before they reach the coast, verifying bloom movement and forecasting potential respiratory irritation.

Why Should You Care?
Red Tide in Florida and Texas produces a toxin that may have harmful effects on marine life. For people, The toxin may also become airborne, which can lead to eye irritation and respiratory issues in people. People with serious respiratory conditions such as asthma may experience more severe symptoms.| Transcript
Putting the Forecast into Action
The condition reports for red tide in Florida and Texas are available to the public and give the daily level of respiratory irritation forecasts by coastal region. NOAA also issues HAB bulletins that contain analyses of ocean color satellite imagery, field observations, models, public health reports, and buoy data. The bulletins also contain forecasts of potential Karenia brevis bloom transport, intensification, and associated respiratory irritation based on the analysis of information from partners and data providers. The bulletins are primarily issued to public health managers, natural resource managers, and scientists interested in HABs. A week after the the bulletin is issued, it is posted to the Bulletin Archive where the public can access it.

Making Choices
State and local resources are available to help beachgoers find nearby beaches and coastal areas that are not affected by red tide, but are still nearby. | Transcript
<!–

NOAA Forecasts Can Save Your Beach Day
By paying attention to NOAA’s HAB forecasts, beachgoers can still have a good time along the Florida and Texas coast. The conditions report for Red Tide in Florida and Texas can
be found online. | Transcript
–>
Infographic Transcript: Red Tide
Red Tide in Florida and Texas is caused by the rapid growth of a microscopic algae called Karenia brevis. When large amounts of this algae are present, it can cause a harmful algal bloom (HAB) that can be seen from space. NOAA issues HAB forecasts based on satellite imagery and cell counts of Karenia brevis collected in the field and analyzed by NOAA partners.
Why should you care? Red Tide in Florida and Texas produces a toxin that can have harmful effects for marine life. For people, the toxin can become airborne and cause respiratory issues and eye irritation. These symptoms can be more severe for people with serious respiratory issues such as asthma.
Making Choices. State and local resources are available to help beachgoers find beaches and coastal areas that are not impacted by Red Tide, but are still nearby.