Archive for December, 2018
Uganda Python Cave, Egyptian fruit bats, and the deadly Marburg virus
Thursday, December 20th, 2018..
Deep inside the forests of Uganda, Python Cave swarms with thousands of Egyptian fruit bats. CDC scientists have found that many of these bats carry the deadly Marburg virus, a close cousin to Ebola.
Tourists visiting the cave have contracted Marburg, and nearby villages have experienced devastating outbreaks.
But predicting which villages are at risk is challenging. What health experts really need to know is where the bats go at night to better understand how the virus is transmitted to humans. To answer that question, CDC scientists have spearheaded a small pilot project with Ugandan experts to put GPS units on the backs of bats to track their movements. It’s wild work but the risk will have been worth it if the information they get can help shed light on where the bats are going and how they get there. Operating a mobile lab in a remote jungle has its challenges, not to mention monkeys- lots of them. In the heart of Queen Elizabeth National Park, scientists trail through one and a half kilometers of terrain to reach the entrance of the cave as nearby hippos, elephants and zebras take notice. Besides bats, Python Cave is full of sharp rocks, ants, ticks, and-of course-snakes. So scientists must wear head-to-toe protective gear to safely work under these conditions. One by one, these wing flapping mammals are captured in fabric bags. Back at the mobile lab, scientists carefully glue a small GPS unit onto the bat’s backs, in a place that doesn’t interfere with their ability to fly.The bats are then released to go back to the cave. When evening falls, the magic begins. As the bats fly out to forage, their routes are tracked by satellite.
The project at Python Cave has shown that some bats fly dozens of miles in a single night and visit other local caves. Scientists hope that the information from this project will help better predict which areas are most at risk for Marburg, so the next outbreak can be stopped before it ever starts.
Explaining Extreme Events in 2017 from a Climate Perspective
Thursday, December 20th, 2018
Download by Chapter:
- Hydroclimatic Extremes as Challenges for the Water Management Community: Lessons from Oroville Dam and Hurricane Harvey
- Observations of the Rate and Acceleration of Global Mean Sea Level Change
- Anthropogenic Contributions to the Intensity of the 2017 United States Northern Great Plains Drought
- Attribution of the 2017 Northern High Plains Drought
- The Extremely Wet March of 2017 in Peru
- Contribution of Anthropogenic Climate Change to April–May 2017 Heavy Precipitation over the Uruguay River Basin
- December 2016: Linking the Lowest Arctic Sea-Ice Extent on Record with the Lowest European Precipitation Event on Record
- The Exceptional Summer Heat Wave in Southern Europe 2017
- Examining the Potential Contributions of Extreme “Western v” Sea Surface Temperatures to the 2017 March–June East African Drought
- Risks of Pre-Monsoon Extreme Rainfall Events of Bangladesh: Is Anthropogenic Climate Change Playing a Role?
- The Effects of Natural Variability and Climate Change on the Record Low Sunshine over Japan During August 2017
- Anthropogenic Contribution to the 2017 Earliest Summer Onset in South Korea
- Anthropogenic Influence on the Heaviest June Precipitation in Southeastern China Since 1961
- Attribution of the Persistent Spring–Summer Hot and Dry Extremes over Northeast China in 2017
- Anthropogenic Warming Has Substantially Increased the Likelihood of July 2017–like Heat Waves over Central Eastern China
- Attribution of a Record-Breaking Heatwave Event in Summer 2017 over the Yangtze River Delta
- The Role of Natural Variability and Anthropogenic Climate Change in the 2017/18 Tasman Sea Marine Heatwave
- On Determining the Impact of Increasing Atmospheric CO2 on the Record Fire Weather in Eastern Australia in February
Emergent BioSolutions Inc. announced that Health Canada has approved the company’s New Drug Submission (NDS) for its anthrax vaccine, BioThrax® (Anthrax Vaccine Adsorbed).
Thursday, December 20th, 2018- BioThrax is indicated for active immunization for the prevention of disease caused by Bacillus anthracis, in individuals 18 through 65 years of age, whose occupation or other activities place them at risk of exposure, regardless of the route of exposure.
- BioThrax is administered in a three-dose primary schedule (0, 1 and 6 months) with boosters at three-year intervals recommended thereafter.
Nigeria: Since the beginning of the yellow fever outbreak on 12 September 2017, a total of 3 510 suspected cases including 74 deaths (CFR 2.1%).
Wednesday, December 19th, 2018EVENT DESCRIPTION Nigeria experienced a large yellow fever outbreak from September 2017 to late-March 2018 and since then, sporadic cases continued to occur. However since late-September 2018, a new cluster of suspected yellow fever cases emerged in Edo State, located in the southern part of Nigeria. In week 41 (week ending 14 October 2018), one presumptive yellow fever case was confirmed, followed by three presumptive cases in week 42, and more cases occurred subsequently. Between 22 September and 10 December 2018, a total of 97 suspected yellow fever cases, including 23 deaths (case fatality ratio (CFR) 23.7%) were reported across 15 (out of 18) local government areas (LGAs) in Edo State. More than half of these cases occurred in the last two weeks. …..


Since the beginning of the yellow fever outbreak on 12 September 2017, a total of 3 510 suspected cases including 74 deaths (CFR 2.1%), have been reported from all 36 states and the Federal Capital Territory……
Males constitute 58% of all cases and the most affected age groups are 1-10 years (41%), followed by 11-20 years (22%) and 21-30 years (19%).
PUBLIC HEALTH ACTIONS The International Coordinating Group (ICG) has approved 1.38 million doses of yellow fever vaccine from the global emergency vaccine stockpile for an immediate reactive mass vaccination campaign, targeting 1.24 million people in eight LGAs. Active surveillance has been enhanced across the country, including active case search and case investigations of alerts. A National Rapid Response Team (RRT) has been deployed to Edo State to conduct epidemiological, entomological and laboratory investigations and support local response efforts. The RRT is working with the state health authorities, WHO and other partners to implement outbreak response activities, including active case search, sensitization of health workers and communities, and entomological surveillance. Implementation of vector surveillance and targeted vector control activities are ongoing, with emphasis on managing Aedes species. WHO is providing technical support to the state and national authorities, including deploying yellow fever experts to support the country response in Edo State.
SITUATION INTERPRETATION A new focus of yellow fever outbreak has been confirmed in Edo State, Nigeria, following the large outbreak that started in September 2017 up to late-March 2018. While Nigeria introduced yellow fever vaccine into routine immunization in September 2016, the country remains vulnerable to the disease. The global strategy to Eliminate Yellow Fever Epidemic (EYE) identified Nigeria as a high priority country for large preventive mass vaccination campaigns. Entomological investigations conducted in various parts of the country identified the presence of competent mosquito vectors (Aedes aeqypti). In response to the 2017 outbreak, several rounds of reactive vaccination campaign have already been conducted in a number of states, while a scheduled preventive vaccination campaign is currently ongoing in six states.
In Edo State, yellow fever vaccination coverage in children below one year of age is about 69% and approximately 60% in the rest of the population, leaving a significant number of people susceptible to the disease. The current outbreak has occurred close to the state capital, Benin city, which is moderately cosmopolitan, with high population movements due to trade.
An influx of persons with low immunity to yellow fever coming from other parts of the country, Europe and America into Edo state for the Christmas holidays is expected. All these underlying issues are significant, calling for the rapid implementation of the upcoming reactive vaccination campaign.
157
Lassa Fever Outbreak in Benin
Wednesday, December 19th, 2018EVENT DESCRIPTION On 7 December 2018, the Ministry of Health in Benin notified WHO of an outbreak of Lassa fever in Borgou Department, located in the north-east, at the border with Nigeria. The event was initially reported by the departmental health authority on 6 December 2018, following detection of a suspected Lassa fever case in the Departmental University Hospital Centre (CHUD) of Borgou-Alibori in Parakou city.

The case-patient, a 22-year old Beninese housewife who live in Taberou village, Kwara State, Nigeria, reportedly developed a febrile illness on 23 November 2018 while in Nigeria, from where she initially sought medical treatment. However due to lack of improvement, the family brought her back home to Benin on 29 November 2018 and she was admitted to the teaching hospital (the same day), presenting with fever, haematemesis (vomiting blood), and melaena (blood in her stools). The disease eventually progressed in the subsequent days, with conjunctival hyperaemia, severe weakness and dysphagia, among other symptoms. Blood and urine specimens were obtained and shipped to the viral haemorrhagic fever national laboratory in Cotonou, arriving on 6 December 2018. Test results released on 7 December 2018 were positive for Lassa fever by reverse transcription polymerase chain reaction (RT-PCR).
On 6 December 2018, the spouse of the confirmed index case was found to have symptoms and a blood specimen was obtained, and the test result also turned out positive for Lassa fever. On 9 December 2018, one of the two children of the confirmed cases (a couple) developed high fever and a blood specimen was obtained and the initial test result was negative. However, a repeat sample tested positive for Lassa fever.
As of 16 December 2018, three confirmed cases have been reported, with no deaths. The three patients are admitted in the CHUD and all are reported to be in good clinical condition. A total of 33 contacts, including 24 health professionals, four carers and four patients, have been identified and are being monitored. Further epidemiological investigations are ongoing.
PUBLIC HEALTH ACTIONS On 7 December 2018, the Minister of Health held a press conference to declare the Lassa fever outbreak and provide information on preventive measures to the public. The Ministry of Health convened an emergency meeting of the Crisis Management Committee (CMC) on 7 December 2018 to plan and institute response measures to the outbreak. Structures of the CMC have been activated, including the sub-committees and coordination meetings have been scheduled at the national and sub-national levels. The national rapid response team have been deployed to the affected area to conduct detailed epidemiological investigations and support local response efforts. Isolation and treatment rooms have been prepared to manage the suspected and confirmed cases. Medical commodities, including personal protective equipment, medicines, and medical consumables previously positioned are being used, while additional supplies are being mobilized. Surveillance has been enhanced, including active case search, identification and follow-up of contacts. Public health education and sensitization of the population is ongoing, in particular native healers, opinion, religious and traditional leaders. Dissemination of public awareness messages on prevention measures through local radios and other communication channels is taking place. Aware raising activities have been conducted, targeting taxi and motorcycle-taxi drivers, community relays, religious leaders, teachers and traditional healers, aimed to improve case detection and prevention of Lassa fever infections.
SITUATION INTERPRETATION An outbreak of Lassa fever has been confirmed in Benin, with an epidemiological link to Kwara State in Nigeria. The national authorities have moved quickly in the bid to contain this outbreak, to prevent further spread and establishment of local transmission. Several measures have been instituted, including contact identification and follow-up, aimed to promptly detect, isolate and investigate suspected cases for speedy laboratory confirmation. Further investigations are also ongoing to better understand the outbreak.
However, this event should be a wakeup call to the national authorities to step up preparedness measures for Lassa fever across the country, especially along the borders with Nigeria. Functional port health services and cross border surveillance is paramount, in light of the fact that the index case in this event crossed the border with symptoms. Improving routine universal precautions in healthcare settings is also critical, since about 70% of contacts during this event are health professionals.
Geographical
‘Vacation Cutting’
Wednesday, December 19th, 2018“….Girls in Kenya are being taken across the border to countries such as Uganda, Tanzania, Somalia and Ethiopia for female genital mutilation (FGM) to avoid a crackdown on the harmful traditional practice at home, campaigners said on Monday.
Kenya criminalized FGM in 2011 with a minimum punishment of three years imprisonment and a U.S. $2,000 fine….”

CDC: Prepare Your Vehicle for Winter Weather
Wednesday, December 19th, 2018

Prepare for extremely cold weather every winter—it’s always a possibility. You can avoid many dangerous winter travel problems by planning ahead.

There are steps you can take in advance for greater wintertime safety in your car.
Have maintenance service on your vehicle as often as the manufacturer recommends. In addition, every fall, do the following:
- Have the radiator system serviced or check the antifreeze level yourself with an antifreeze tester. Add antifreeze as needed.
- Replace windshield-wiper fluid with a wintertime mixture.
- Replace any worn tires, make sure the tires have adequate tread, and check the air pressure in the tires.
During winter, keep the gas tank near full to help avoid ice in the tank and fuel lines.
Checklist
Keep your car fueled and in good working order. Be sure to check the following:
- Antifreeze
- Windshield wiper fluid (wintertime mixture)
- Heater
- Defroster
- Brakes
- Brake fluid
- Ignition
- Emergency flashers
- Exhaust
- Tires (air pressure and wear)
- Fuel
- Oil
- Battery
- Radiator
Brazil: 14 confirmed Chagas disease cases after a family drank the juice of the bacaba, a type of palm tree from the Amazon.
Tuesday, December 18th, 2018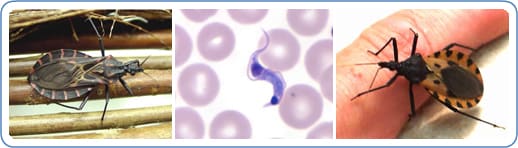
“…..The suspicion is that feces of the barbeque beetle, which transmits the disease, have gone into the juice…..”
Infection can also occur from:
- mother-to-baby (congenital),
- contaminated blood products (transfusions),
- an organ transplanted from an infected donor,
- laboratory accident, or
- contaminated food or drink (rare)
Chagas disease has an acute and a chronic phase. If untreated, infection is lifelong.
Acute Chagas disease occurs immediately after infection, may last up to a few weeks or months, and parasites may be found in the circulating blood. Infection may be mild or asymptomatic. There may be fever or swelling around the site of inoculation (where the parasite entered into the skin or mucous membrane). Rarely, acute infection may result in severe inflammation of the heart muscle or the brain and lining around the brain.
Following the acute phase, most infected people enter into a prolonged asymptomatic form of disease (called “chronic indeterminate”) during which few or no parasites are found in the blood. During this time, most people are unaware of their infection. Many people may remain asymptomatic for life and never develop Chagas-related symptoms. However, an estimated 20 – 30% of infected people will develop debilitating and sometimes life-threatening medical problems over the course of their lives.
Complications of chronic Chagas disease may include:
- heart rhythm abnormalities that can cause sudden death;
- a dilated heart that doesn’t pump blood well;
- a dilated esophagus or colon, leading to difficulties with eating or passing stool.
In people who have suppressed immune systems (for example, due to AIDS or chemotherapy), Chagas disease can reactivate with parasites found in the circulating blood. This occurrence can potentially cause severe disease.

Romaña’s sign, the swelling of the child’s eyelid, is a marker of acute Chagas disease. The swelling is due to bug feces being accidentally rubbed into the eye, or because the bite wound was on the same side of the child’s face as the swelling. Photo courtesy of WHO/TDR
The U.S. AFM (Acute Flaccid Myelitis) outbreak grows to 165 cases in 36 states
Tuesday, December 18th, 2018



