Archive for April, 2019
The increasing availability of antibiotics has accelerated an alarming downside: The drugs are losing their ability to kill the germs they were created to conquer.
Monday, April 8th, 2019“…..Antibiotic resistance is a global threat, but it is often viewed as a problem in rich countries, where comfortably insured patients rush to the doctor to demand prescriptions at the slightest hint of a cough or cold.
In fact, urban poverty is a huge and largely unappreciated driver of resistance. And so, the rise of resistant microbes is having a disproportionate impact on poor countries, where squalid and crowded living conditions, lax oversight of antibiotic use and a scarcity of affordable medical care are fueling the spread of infections increasingly unresponsive to drugs……”
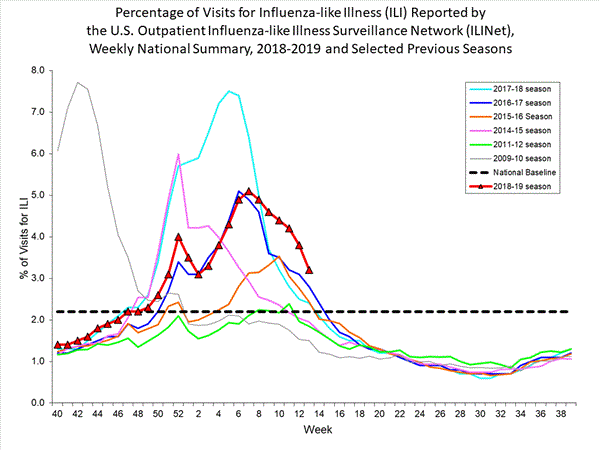
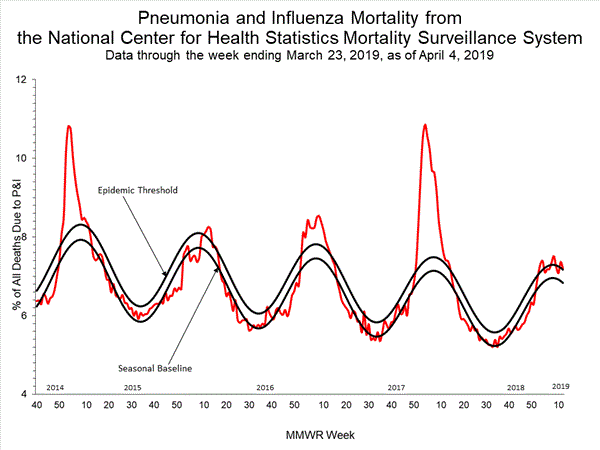
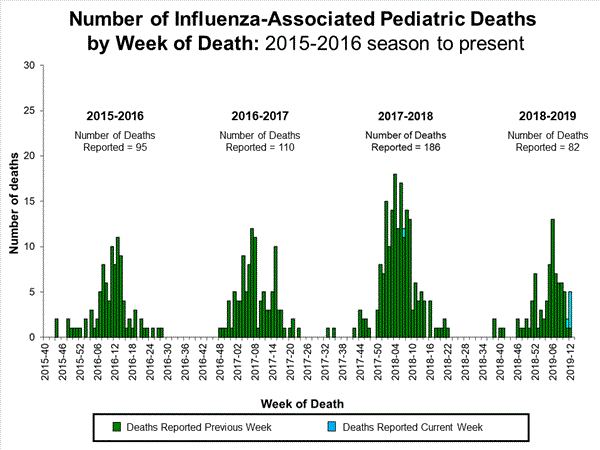
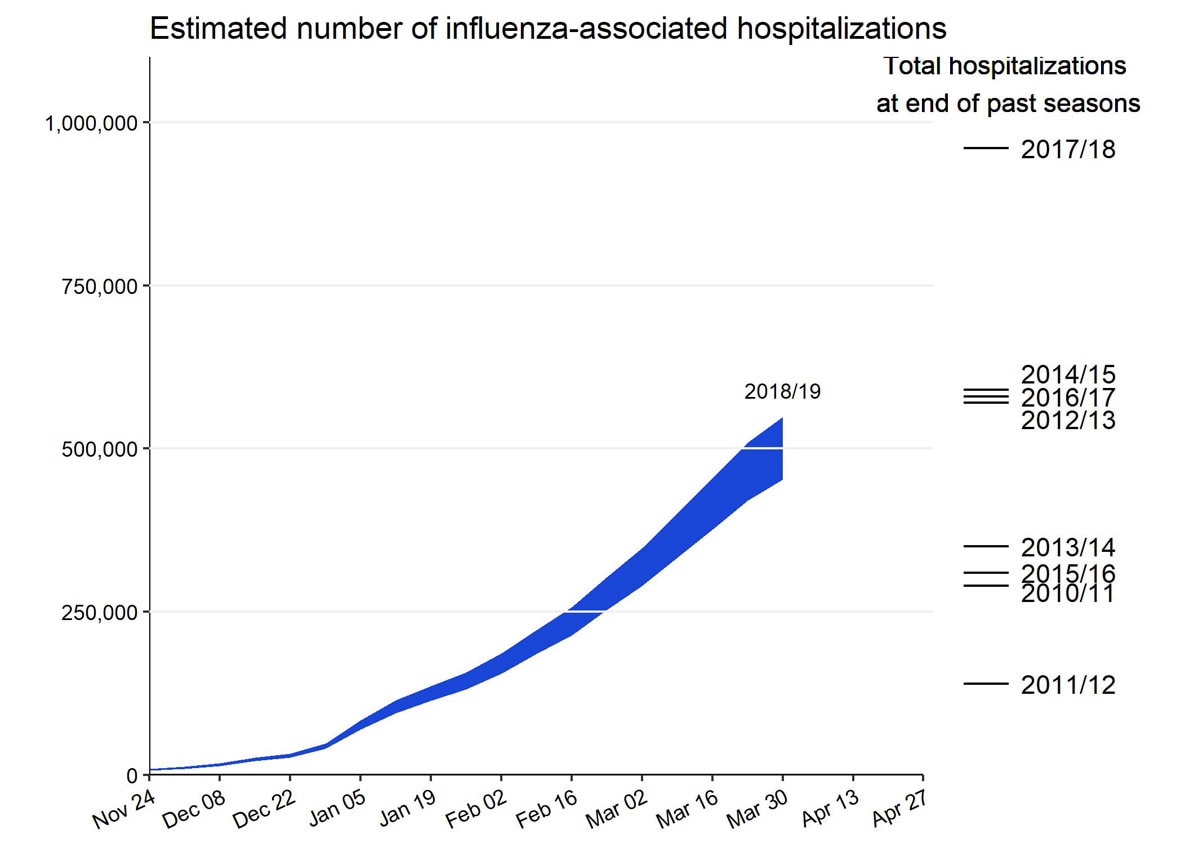
2018-2019 Influenza Season Week 13 ending March 30, 2019: Influenza activity decreased but remains elevated in the United States.
Sunday, April 7th, 2019H1ssF_3928: The universal flu vaccine?
Sunday, April 7th, 2019“The first clinical trial of an innovative universal influenza vaccine candidate is examining the vaccine’s safety and tolerability as well as its ability to induce an immune response in healthy volunteers. Scientists at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, developed the experimental vaccine, known as H1ssF_3928.
H1ssF_3928 is designed to teach the body to make protective immune responses against diverse influenza subtypes by focusing the immune system on a portion of the virus that varies relatively little from strain to strain. ….

The clinical trial is being conducted at the NIH Clinical Center in Bethesda, Maryland. It is being led by Grace Chen, M.D., of NIAID’s Vaccine Research Center (VRC) Clinical Trials Program. The trial will gradually enroll at least 53 healthy adults aged 18 to 70 years. The first five participants will be aged 18 to 40 years and will receive a single 20-microgram (mcg) intramuscular injection of the experimental vaccine. The remaining 48 participants will receive two 60-mcg vaccinations spaced 16 weeks apart. They will be stratified by age into four groups of 12 people each: 18 to 40 years, 41 to 49 years, 50 to 59 years, and 60 to 70 years. Investigators hope to understand how participants’ immune responses to the experimental vaccine may vary based on age and the likelihood of their previous exposure to different influenza variants.
Study participants will be asked to record their temperature and any symptoms on a diary card for one week after each injection. They also will be asked to visit the clinic to provide blood samples at various time points. Investigators will test the samples in the laboratory to characterize and measure levels of anti-influenza antibodies, which are potentially indicative of immunity against influenza. Participants will return for nine to 11 follow-up visits over 12 to 15 months. They will not be exposed to any influenza virus as part of the clinical trial…..”
CDC: People at High Risk of Developing Serious Flu–Related Complications
Sunday, April 7th, 2019People at High Risk of Developing Flu-Related Complications
- Children younger than 5, but especially children younger than 2 years old
- Adults 65 years of age and older
- Pregnant women (and women up to two weeks postpartum)
- Residents of nursing homes and other long-term care facilities
- Also, American Indians and Alaska Natives[1.1 MB, 2 pages] seem to be at higher risk of flu complications
People who have medical conditions including:
- Asthma
- Neurological and neurodevelopmental conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury)
- Chronic lung disease (such as chronic obstructive pulmonary disease [COPD] and cystic fibrosis)
- Heart disease (such as congenital heart disease, congestive heart failure and coronary artery disease)
- Blood disorders (such as sickle cell disease)
- Endocrine disorders (such as diabetes)
- Kidney disorders
- Liver disorders
- Metabolic disorders (such as inherited metabolic disorders and mitochondrial disorders)
- Weakened immune system due to disease or medication (such as people with HIV or AIDS, or cancer, or those on chronic steroids)
- People younger than 19 years of age who are receiving long-term aspirin therapy
- People with extreme obesity (body mass index [BMI] of 40 or more) Calculate your Body Mass Index or BMI
Preliminary Burden Estimates: CDC estimates that, from October 1, 2018, through March 30, 2019, there have been:
Saturday, April 6th, 2019
flu illnesses
15.3 million – 17.8 million
flu medical visits
452,000 – 549,000
flu hospitalizations
30,600 – 50,900
flu deaths
WHO-UNICEF: One in four health care facilities around the world lacks basic water services, impacting over 2 billion people
Saturday, April 6th, 2019
The WHO/UNICEF JMP report, WASH in Health Care Facilities, is the first comprehensive global assessment of water, sanitation and hygiene (WASH) in health care facilities. It also finds that 1 in 5 health care facilities has no sanitation service*, impacting 1.5 billion people. The report further reveals that many health centres lack basic facilities for hand hygiene and safe segregation and disposal of health care waste.
These services are crucial to preventing infections, reducing the spread of antimicrobial resistance and providing quality care, particularly for safe childbirth.
“Water, sanitation and hygiene services in health facilities are the most basic requirements of infection prevention and control, and of quality care. They are fundamental to respecting the dignity and human rights of every person who seeks health care and of health workers themselves,†said António Guterres, United Nations Secretary-General. “I call on people everywhere to support action for WASH in all health care facilities. This is essential to achieve the Sustainable Development Goals.â€
The WHO/UNICEF JMP report found that just half – 55 per cent – of health care facilities in Least Developed Countries (LDCs) had basic water services. It is estimated that 1 in 5 births globally takes place in LDCs, and that, each year, 17 million women in these countries give birth in health centres with inadequate water, sanitation and hygiene.
“When a baby is born in a health facility without adequate water, sanitation and hygiene, the risk of infection and death for both the mother and the baby is high,†said UNICEF Executive Director Henrietta Fore. “Every birth should be supported by a safe pair of hands, washed with soap and water, using sterile equipment, in a clean environment.â€
In an accompanying report, Water, sanitation, and hygiene in health care facilities: Practical steps to achieve universal access for quality care, WHO and UNICEF researchers note that more than 1 million deaths each year are associated with unclean births. Infections account for 26% of neonatal deaths and 11% of maternal mortality.
“Imagine giving birth or taking your sick child to a health centre with no safe water, toilets or handwashing facilities,†said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “That’s the reality for millions of people every day. No one should have to do that, and no health worker should have to provide care in those circumstances. Ensuring that all health care facilities have basic water, sanitation and hygiene services is essential for achieving a healthier, safer, fairer world.â€
At the 2019 World Health Assembly to be held in May, governments will debate a resolution on Water, Sanitation and Hygiene in Health Care Facilities which was unanimously approved by the WHO Executive Board earlier this year.
The WHO and UNICEF Practical Steps report provides details on eight actions governments can take to improve the WASH services in health care facilities including establishing national plans and targets, improving infrastructure and maintenance and engaging communities. These actions and resulting improvements in WASH services can yield dramatic returns on investment in the form of improved maternal and newborn health, preventing antimicrobial resistance, stopping disease outbreaks and improving quality of care.
According to UNICEF, 7,000 newborn babies died every day in 2017, mostly from preventable and treatable conditions including infections like sepsis. As part of its Every Child Alive Campaign, UNICEF is calling for governments and authorities to make sure every mother and baby have access to affordable, quality care.Â
Last year, Fore and Dr Tedros called on countries to strengthen their primary health care systems as an essential step toward achieving universal health coverage.
–
“Scary Monsters and Nice Sprites” in the fight against Aedes Aegyptii
Friday, April 5th, 2019“…..The observation that such music can delay host attack, reduce blood feeding, and disrupt mating provides new avenues for the development of music-based personal protective and control measures against Aedes-borne diseases…..”
Acta Tropica
Volume 194, June 2019, Pages 93-99

The electronic song “Scary Monsters and Nice Sprites” reduces host attack and mating success in the dengue vector Aedes aegypti
Using A Tiny Guillotine In The Fight Against Malaria
Friday, April 5th, 2019440,000 died from malaria in 2016.
“…..To produce a vaccine for mass deployment, biotech firm Sanaria has to decapitate and dissect out the salivary glands, which hold the malaria-causing parasite, for each individual mosquito—by hand. To speed up this painstaking process, they’ve partnered with medical roboticists from Johns Hopkins University to engineer a mosquito guillotine that technicians can use to decapitate 30 insects at a time. It’s a first step toward an eventual goal of a fully automated robotic guillotine, which could help Sanaria produce that elusive mass-produced, effective malaria vaccine…..”
The Scottish island of Gruinard (Anthrax Island): The Island of Death.
Friday, April 5th, 2019“….Over the summer of 1942 and 1943, sheep were placed in open pens and then exposed to bombs, dropped from a Vickers Wellington bomber plane, that scattered anthrax spores across the land. The power of anthrax became quickly clear when the sheep started dying after three days with its potential to cause mass destruction summed up in the report of the tests……”
3 April 2019: An oral cholera vaccination campaign to protect survivors of Cyclone Idai begins today in Beira, Mozambique.
Friday, April 5th, 2019WHO
An oral cholera vaccination campaign to protect survivors of Cyclone Idai begins today in Beira, Mozambique. Funded by Gavi, the Vaccine Alliance, the campaign will be carried out by the Mozambique Ministry of Health, with support from WHO and other partners, including UNICEF, the International Federation of the Red Cross and Red Crescent Societies (IFRC), Médecins Sans Frontières (MSF) and Save the Children.
There has already been one reported cholera death and almost 1500 reported cases following the cyclone, which caused severe flooding in Mozambique, Zimbabwe, Malawi and Madagascar after making landfall in March. Nine cholera treatment centres, with 500-bed capacity, are already admitting patients.
“Cyclone Idai’s trail of devastation has left the city of Beira’s water and sanitation infrastructure in ruins, providing the perfect conditions for cholera to spread,” said Gavi CEO, Dr Seth Berkley. “This cyclone has already caused enough devastation and misery across south east Africa; we have to hope these vaccines will help stop a potentially major outbreak and prevent yet more suffering.”
“Hundreds of thousands of people are living in terrible conditions in temporary settlements without safe drinking water and sanitation, putting them at serious risk of cholera and other diseases,” said Dr Tedros Adhanom Ghebreyesus, Director-General of WHO. “The key thing is to make sure that people can access rapid treatment and clean water and sanitation. The oral cholera vaccine is a vital emergency measure that will help save lives and stop the spread of this horrible disease.”
WHO is supporting the Ministry of Health to coordinate the oral cholera vaccination campaign, including working with partners to ensure an appropriate cold chain storage and providing logistical support.
Cholera is endemic to Mozambique, which has had regular outbreaks over the past five years. About 2 000 people were infected in the last outbreak, which ended in February 2018.
The 884 953 doses of oral cholera vaccine arrived in Mozambique on Tuesday. They were taken from the global cholera vaccine stockpile, which is fully-funded by Gavi. Gavi is also supporting operational costs of the campaign. The use of the stockpile for outbreak response is managed by the International Coordinating Group (ICG), which features representatives from WHO, UNICEF, IFRC and MSF.
Since the stockpile was launched in 2013, millions of doses every year have helped tackle outbreaks across the globe. In the fifteen years between 1997 and 2012, just 1.5 million doses of oral cholera vaccine were used worldwide. In 2018 alone, the stockpile provided 17 million of doses to 22 different countries. Since the beginning of 2019, more than 6 million doses have already been shipped to respond to outbreaks or address endemic cholera in many countries including Democratic Republic of the Congo, Nigeria, Somalia and Zimbabwe.