Chagas Disease: Approximately 300,000 people are living with this disease in the United States.
April 23rd, 2017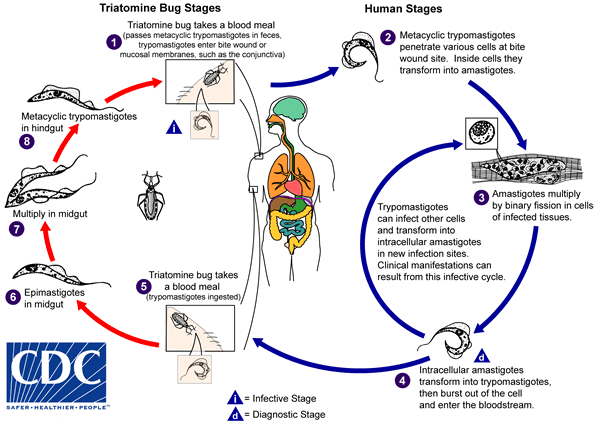
An infected triatomine insect vector (or “kissing” bug) takes a blood meal and releases trypomastigotes in its feces near the site of the bite wound. Trypomastigotes enter the host through the wound or through intact mucosal membranes, such as the conjunctiva  . Common triatomine vector species for trypanosomiasis belong to the genera Triatoma, Rhodnius, and Panstrongylus. Inside the host, the trypomastigotes invade cells near the site of inoculation, where they differentiate into intracellular amastigotes
. Common triatomine vector species for trypanosomiasis belong to the genera Triatoma, Rhodnius, and Panstrongylus. Inside the host, the trypomastigotes invade cells near the site of inoculation, where they differentiate into intracellular amastigotes  . The amastigotes multiply by binary fission
. The amastigotes multiply by binary fission  and differentiate into trypomastigotes, and then are released into the circulation as bloodstream trypomastigotes
and differentiate into trypomastigotes, and then are released into the circulation as bloodstream trypomastigotes  . Trypomastigotes infect cells from a variety of tissues and transform into intracellular amastigotes in new infection sites. Clinical manifestations can result from this infective cycle. The bloodstream trypomastigotes do not replicate (different from the African trypanosomes). Replication resumes only when the parasites enter another cell or are ingested by another vector. The “kissing” bug becomes infected by feeding on human or animal blood that contains circulating parasites
. Trypomastigotes infect cells from a variety of tissues and transform into intracellular amastigotes in new infection sites. Clinical manifestations can result from this infective cycle. The bloodstream trypomastigotes do not replicate (different from the African trypanosomes). Replication resumes only when the parasites enter another cell or are ingested by another vector. The “kissing” bug becomes infected by feeding on human or animal blood that contains circulating parasites  . The ingested trypomastigotes transform into epimastigotes in the vector’s midgut
. The ingested trypomastigotes transform into epimastigotes in the vector’s midgut  . The parasites multiply and differentiate in the midgut
. The parasites multiply and differentiate in the midgut  and differentiate into infective metacyclic trypomastigotes in the hindgut
and differentiate into infective metacyclic trypomastigotes in the hindgut  .
.
Trypanosoma cruzi can also be transmitted through blood transfusions, organ transplantation, transplacentally, and in laboratory accidents.
Chagas disease is caused by the parasite Trypanosoma cruzi, which is transmitted to animals and people by insect vectors that are found only in the Americas (mainly, in rural areas of Latin America where poverty is widespread). Chagas disease (T. cruzi infection) is also referred to as American trypanosomiasis.
It is estimated that as many as 8 million people in Mexico, Central America, and South America have Chagas disease, most of whom do not know they are infected. If untreated, infection is lifelong and can be life threatening.
The impact of Chagas disease is not limited to the rural areas in Latin America in which vectorborne transmission occurs. Large-scale population movements from rural to urban areas of Latin America and to other regions of the world have increased the geographic distribution and changed the epidemiology of Chagas disease. In the United States and in other regions where Chagas disease is now found but is not endemic, control strategies should focus on preventing transmission from blood transfusion, organ transplantation, and mother-to-baby (congenital transmission).
How do people get Chagas disease?
People can become infected in various ways. In Chagas disease-endemic areas, the main way is through vectorborne transmission. The insect vectors are called triatomine bugs. These blood-sucking bugs get infected by biting an infected animal or person. Once infected, the bugs pass T. cruzi parasites in their feces. The bugs are found in houses made from materials such as mud, adobe, straw, and palm thatch. During the day, the bugs hide in crevices in the walls and roofs. During the night, when the inhabitants are sleeping, the bugs emerge. Because they tend to feed on people’s faces, triatomine bugs are also known as “kissing bugs. ” After they bite and ingest blood, they defecate on the person. The person can become infected if T. cruzi parasites in the bug feces enter the body through mucous membranes or breaks in the skin. The unsuspecting, sleeping person may accidentally scratch or rub the feces into the bite wound, eyes, or mouth.
People also can become infected through:
- congenital transmission (from a pregnant woman to her baby);
- blood transfusion;
- organ transplantation;
- consumption of uncooked food contaminated with feces from infected bugs; and
- accidental laboratory exposure.
It is generally considered safe to breastfeed even if the mother has Chagas disease. However, if the mother has cracked nipples or blood in the breast milk, she should pump and discard the milk until the nipples heal and the bleeding resolves.
Chagas disease is not transmitted from person-to-person like a cold or the flu or through casual contact with infected people or animals.
If I have Chagas disease, should my family members be tested for the infection?
Possibly. They should be tested if they:
- could have become infected the same way that you did, for example, by vectorborne transmission in Latin America;
- received blood or organs that you donated after you already were infected;
- are your children and were born after you were infected; or if
- there are other reasons to think that they might have Chagas disease.
In what parts of the world is Chagas disease found?
People who have Chagas disease can be found anywhere in the world. However, vectorborne transmission is confined to the Americas, principally rural areas in parts of Mexico, Central America, and South America. In some regions of Latin America, vector-control programs have succeeded in stopping this type of disease spread. Vectorborne transmission does not occur in the Caribbean (for example, in Puerto Rico or Cuba). Rare vectorborne cases of Chagas disease have been noted in the southern United States.
What are the signs and symptoms of Chagas disease?
Much of the clinical information about Chagas disease comes from experience with people who became infected as children through vectorborne transmission. The severity and course of infection might be different in people infected at other times of life, in other ways, or with different strains of the T. cruzi parasite.
There are two phases of Chagas disease: the acute phase and the chronic phase. Both phases can be symptom free or life threatening.
The acute phase lasts for the first few weeks or months of infection. It usually occurs unnoticed because it is symptom free or exhibits only mild symptoms and signs that are not unique to Chagas disease. The symptoms noted by the patient can include fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. The signs on physical examination can include mild enlargement of the liver or spleen, swollen glands, and local swelling (a chagoma) where the parasite entered the body. The most recognized marker of acute Chagas disease is called Romaña’s sign, which includes swelling of the eyelids on the side of the face near the bite wound or where the bug feces were deposited or accidentally rubbed into the eye. Even if symptoms develop during the acute phase, they usually fade away on their own, within a few weeks or months. Although the symptoms resolve, if untreated the infection persists. Rarely, young children (<5%) die from severe inflammation/infection of the heart muscle (myocarditis) or brain (meningoencephalitis). The acute phase also can be severe in people with weakened immune systems.
During the chronic phase, the infection may remain silent for decades or even for life. However, some people develop:
- cardiac complications, which can include an enlarged heart (cardiomyopathy), heart failure, altered heart rate or rhythm, and cardiac arrest (sudden death); and/or
- intestinal complications, which can include an enlarged esophagus (megaesophagus) or colon (megacolon) and can lead to difficulties with eating or with passing stool.
The average life-time risk of developing one or more of these complications is about 30%.
What should I do if I think I have Chagas disease?
You should discuss your concerns with your health care provider, who will examine you and ask you questions (for example, about your health and where you have lived). Chagas disease is diagnosed by blood tests. If you are found to have Chagas disease, you should have a heart tracing test (electrocardiogram), even if you feel fine. You might be referred to a specialist for more tests and for treatment.
What if I’ve been diagnosed with Chagas disease but have a normal EKG?
If you have been diagnosed with Chagas disease, your doctor may perform an electrocardiogram (EKG or ECG) to check for any problems with the electrical activity of your heart. Even if this test is normal, you still may need to be given antiparasitic medication used to treat Chagas disease. Your physician may wish to review CDC’s recommendations for evaluation and treatment for more information.
How is Chagas disease treated?
There are two approaches to therapy, both of which can be life saving:
- antiparasitic treatment, to kill the parasite; and
- symptomatic treatment, to manage the symptoms and signs of infection.
Antiparasitic treatment is most effective early in the course of infection but is not limited to cases in the acute phase. In the United States, this type of treatment is available through CDC. Your health care provider can talk with CDC staff about whether and how you should be treated. Most people do not need to be hospitalized during treatment.
Symptomatic treatment may help people who have cardiac or intestinal problems from Chagas disease. For example, pacemakers and medications for irregular heartbeats may be life saving for some patients with chronic cardiac disease.
I plan to travel to a rural area of Latin America that might have Chagas disease. How can I prevent infection?
No drugs or vaccines for preventing infection are currently available. Travelers who sleep indoors, in well-constructed facilities (for example, air-conditioned or screened hotel rooms), are at low risk for exposure to infected triatomine bugs, which infest poor-quality dwellings and are most active at night. Preventive measures include spraying infested dwellings with residual-action insecticides, using bed nets treated with long-lasting insecticides, wearing protective clothing, and applying insect repellent to exposed skin. In addition, travelers should be aware of other possible routes of transmission, including bloodborne and foodborne.


