Archive for the ‘CDC’ Category
CDC: Coronavirus Disease 2019 (COVID-19) Situation Summary, 2/25/20
Tuesday, February 25th, 2020https://www.cdc.gov/coronavirus/2019-nCoV/summary.html
This is an emerging, rapidly evolving situation and CDC will provide updated information as it becomes available, in addition to updated guidance.
Updated February 25, 2020
Background
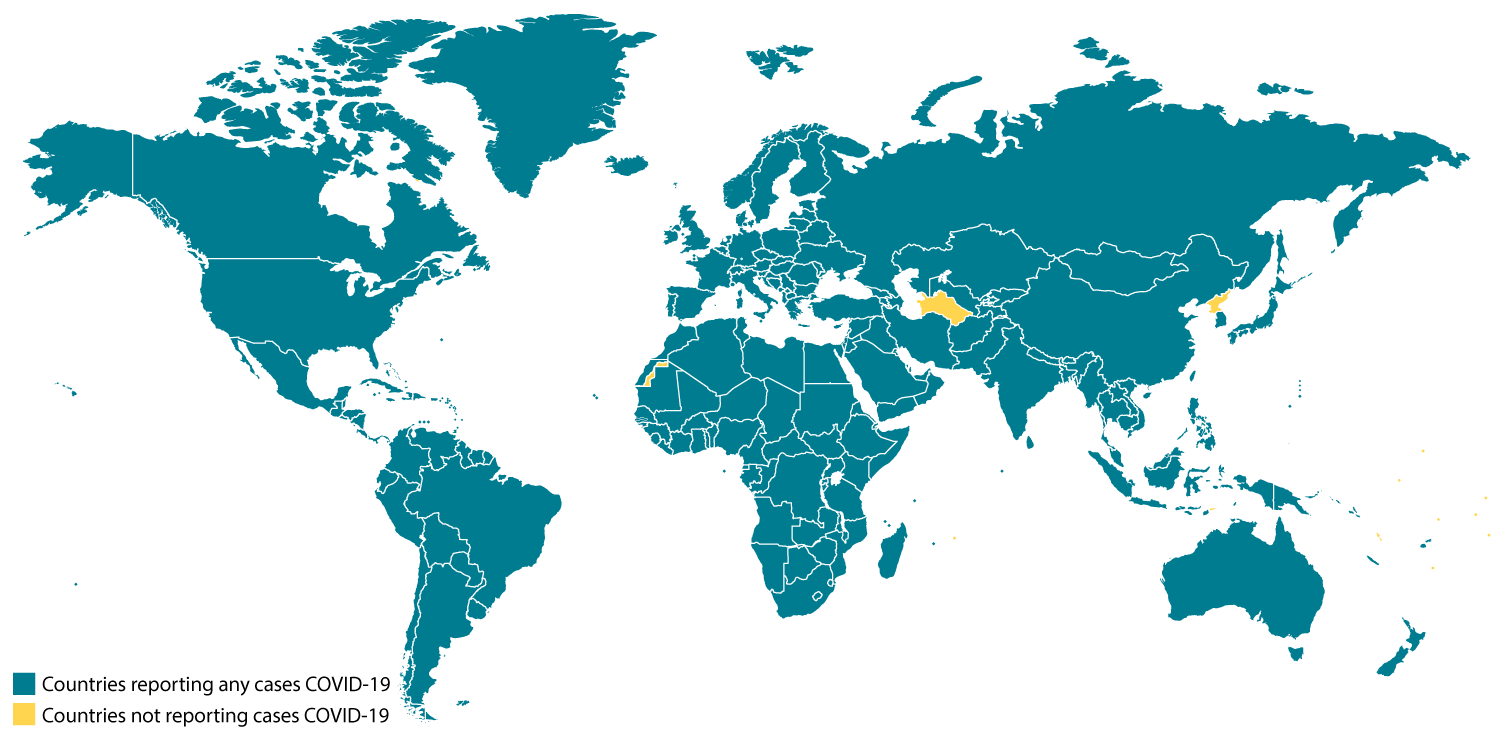
CDC is responding to an outbreak of respiratory disease caused by a novel (new) coronavirus that was first detected in Wuhan City, Hubei Province, China and which has now been detected in 37 locations internationally, including cases in the United States. The virus has been named “SARS-CoV-2” and the disease it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”).
On January 30, 2020, the International Health Regulations Emergency Committee of the World Health Organization declared the outbreak a “public health emergency of international concernexternal icon” (PHEIC). On January 31, 2020, Health and Human Services Secretary Alex M. Azar II declared a public health emergency (PHE) for the United States to aid the nation’s healthcare community in responding to COVID-19.
Source and Spread of the Virus
Coronaviruses are a large family of viruses that are common in many different species of animals, including camels, cattle, cats, and bats. Rarely, animal coronaviruses can infect people and then spread between people such as with MERS-CoV, SARS-CoV, and now with this new virus (named SARS-CoV-2).
The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats. The sequences from U.S. patients are similar to the one that China initially posted, suggesting a likely single, recent emergence of this virus from an animal reservoir.
Early on, many of the patients in the COVID-19 outbreak in Wuhan, China had some link to a large seafood and live animal market, suggesting animal-to-person spread. Later, a growing number of patients reportedly did not have exposure to animal markets, indicating person-to-person spread. Person-to-person spread has been reported outside China, including in the United States and other locations. Chinese officials report that sustained person-to-person spread in the community is occurring in China. In addition, other destinations have apparent community spread, meaning some people have been infected who are not sure how or where they became infected. Learn what is known about the spread of newly emerged coronaviruses.
Situation in U.S.
Imported cases of COVID-19 in travelers have been detected in the U.S. Person-to-person spread of COVID-19 also has been seen among close contacts of returned travelers from Wuhan, but at this time, this virus is NOT currently spreading in the community in the United States.
Illness Severity
Both MERS-CoV and SARS-CoV have been known to cause severe illness in people. The complete clinical picture with regard to COVID-19 is not fully understood. Reported illnesses have ranged from mild to severe, including illness resulting in death. Learn more about the symptoms associated with COVID-19.
There are ongoing investigations to learn more. This is a rapidly evolving situation and information will be updated as it becomes available.
Risk Assessment
Outbreaks of novel virus infections among people are always of public health concern. The risk from these outbreaks depends on characteristics of the virus, including how well it spreads between people, the severity of resulting illness, and the medical or other measures available to control the impact of the virus (for example, vaccine or treatment medications). The fact that this disease has caused illness, including illness resulting in death, and sustained person-to-person spread is concerning. These factors meet two of the criteria of a pandemic. As community spread is detected in more and more countries, the world moves closer toward meeting the third criteria, worldwide spread of the new virus.
The potential public health threat posed by COVID-19 is high, both globally and to the United States.
But individual risk is dependent on exposure.
- For the general American public, who are unlikely to be exposed to this virus at this time, the immediate health risk from COVID-19 is considered low.
- Under current circumstances, certain people will have an increased risk of infection, for example healthcare workers caring for patients with COVID-19 and other close contacts of persons with COVID-19. CDC has developed guidance to help in the risk assessment and management of people with potential exposures to COVID-19.
However, it’s important to note that current global circumstances suggest it is likely that this virus will cause a pandemic. In that case, the risk assessment would be different.
What May Happen
More cases are likely to be identified in the coming days, including more cases in the United States. It’s also likely that person-to-person spread will continue to occur, including in the United States. Widespread transmission of COVID-19 in the United States would translate into large numbers of people needing medical care at the same time. Schools, childcare centers, workplaces, and other places for mass gatherings may experience more absenteeism. Public health and healthcare systems may become overloaded, with elevated rates of hospitalizations and deaths. Other critical infrastructure, such as law enforcement, emergency medical services, and transportation industry may also be affected. Health care providers and hospitals may be overwhelmed. At this time, there is no vaccine to protect against COVID-19 and no medications approved to treat it. Nonpharmaceutical interventions would be the most important response strategy.
CDC Response
Global efforts at this time are focused concurrently on containing spread of this virus and mitigating the impact of this virus. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this public health threat. The public health response is multi-layered, with the goal of detecting and minimizing introductions of this virus in the United States so as to reduce the spread and the impact of this virus. CDC is operationalizing all of its pandemic preparedness and response plans, working on multiple fronts to meet these goals, including specific measures to prepare communities to respond local transmission of the virus that causes COVID-19. There is an abundance of pandemic guidance developed in anticipation of an influenza pandemic that is being repurposed and adapted for a COVID-19 pandemic.
Highlights of CDC’s Response
- CDC established a COVID-19 Incident Management System on January 7, 2020. On January 21, CDC activated its Emergency Operations Center to better provide ongoing support to the COVID-19 response.
- The U.S. government has taken unprecedented steps with respect to travel in response to the growing public health threat posed by this new coronavirus:
- Effective February 2, at 5pm, the U.S. government suspended entry of foreign nationals who have been in China within the past 14 days.
- U.S. citizens, residents, and their immediate family members who have been in Hubei province and other parts of mainland China are allowed to enter the United States, but they are subject to health monitoring and possible quarantine for up to 14 days.
- CDC has issued the following travel guidance related to COVID-19:
- China — Level 3, Avoid Nonessential Travel — updated February 22;
- South Korea — Level 3, Avoid Nonessential Travel — updated February 24;
- Japan — Level 2, Practice Enhanced Precautions — updated February 22;
- Iran — Level 2, Practice Enhanced Precautions — issued February 23;
- Italy — Level 2, Practice Enhanced Precautions — issued February 23;
- Hong Kong — Level 1, Practice Usual Precautions — issued February 19.
- CDC also recommends that all travelers reconsider cruise ship voyages into or within Asia at this time.
- CDC is issuing clinical guidance, including:
- An interim Health Alert Network (HAN) Update to inform state and local health departments and healthcare professionals about this outbreak on February 1.
- On January 30, CDC published guidance for healthcare professionals on the clinical care of COVID-19 patients.
- On February 3, CDC posted guidance for assessing the potential risk for various exposures to COVID-19 and managing those people appropriately.
- CDC has deployed multidisciplinary teams to support state health departments with clinical management, contact tracing, and communications.
CDC has worked with the Department of State, supporting the safe return of Americans who have been stranded as a result of the ongoing outbreaks of COVID-19 and related travel restrictions. CDC has worked to assess the health of passengers as they return to the United States and provided continued daily monitoring of people who are quarantined.

This is a picture of CDC’s laboratory test kit for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). CDC is shipping the test kits to laboratories CDC has designated as qualified, including U.S. state and local public health laboratories, Department of Defense (DOD) laboratories and select international laboratories. The test kits are bolstering global laboratory capacity for detecting SARS-CoV-2.
- CDC laboratories have supported the COVID-19 response, including:
- CDC has developed a real time Reverse Transcription-Polymerase Chain Reaction (rRT-PCR) test that can diagnose COVID-19 in respiratory samples from clinical specimens. On January 24, CDC publicly posted the assay protocol for this test.
- CDC has been uploading the entire genome of the viruses from reported cases in the United States to GenBank as sequencing was completed.
- CDC has grown the COVID-19 virus in cell culture, which is necessary for further studies, including for additional genetic characterization. The cell-grown virus was sent to NIH’s BEI Resources Repositoryexternal icon for use by the broad scientific community.
CDC Recommends
- While the immediate risk of this new virus to the American public is believed to be low at this time, everyone can do their part to help us respond to this emerging public health threat:
- It’s currently flu and respiratory disease season and CDC recommends getting a flu vaccine, taking everyday preventive actions to help stop the spread of germs, and taking flu antivirals if prescribed.
- If you are a healthcare provider, be on the look-out for people who recently traveled from China and have fever and respiratory symptoms.
- If you are a healthcare provider caring for a COVID-19 patient or a public health responder, please take care of yourself and follow recommended infection control procedures.
- If you have been in China or have been exposed to someone sick with COVID-19 in the last 14 days, you will face some limitations on your movement and activity. Please follow instructions during this time. Your cooperation is integral to the ongoing public health response to try to slow spread of this virus. If you develop COVID-19 symptoms, contact your healthcare provider, and tell them about your symptoms and your travel or exposure to a COVID-19 patient.
- For people who are ill with COVID-19, please follow CDC guidance on how to reduce the risk of spreading your illness to others.
Other Available Resources
The following resources are available with information on COVID-19
Coronavirus Disease 2019 Information for Travel
Tuesday, February 25th, 2020https://www.cdc.gov/coronavirus/2019-ncov/travelers/index.html
This page includes information about Coronavirus Disease 2019 (COVID-19) for travelers and travel related industries.
CDC recommends that travelers avoid all nonessential travel to:
These destinations are experiencing sustained community transmission of respiratory illness caused by the novel coronavirus (COVID-19). The virus can spread from person to person. Older adults and those with chronic medical conditions should consider postponing nonessential travel.
CDC does not recommend canceling or postponing travel to the following destinations. Travelers should practice usual precautions.
- Singapore
- Taiwan
- Thailand
- Vietnam
Community spread means people have been infected with the virus, including some who are not sure how or where they became infected. At this time, the extent of virus spread is not sustained or widespread enough to meet the criteria for a travel health notice. If that changes, CDC will update this page.
Resources for Ships
Resources for Airlines
CDC Travelers’ Health Update: 2/25/20
Tuesday, February 25th, 2020Coronavirus Disease 2019
Travel: Because of the novel (new) coronavirus outbreak, CDC recommends that travelers avoid travel to mainland China, South Korea, and reconsider cruise ship travel to or within Asia. The recommendation to avoid travel to China applies only to mainland China and does not include Hong Kong, Macau, or the island of Taiwan. CDC has posted several country-specific travel health notices for coronavirus. These notices are also listed in the travel health notice section below. The coronavirus situation is evolving rapidly, and CDC is following it very closely.
CDC: Flowchart to Identify and Assess 2019 Novel Coronavirus
Tuesday, February 11th, 2020
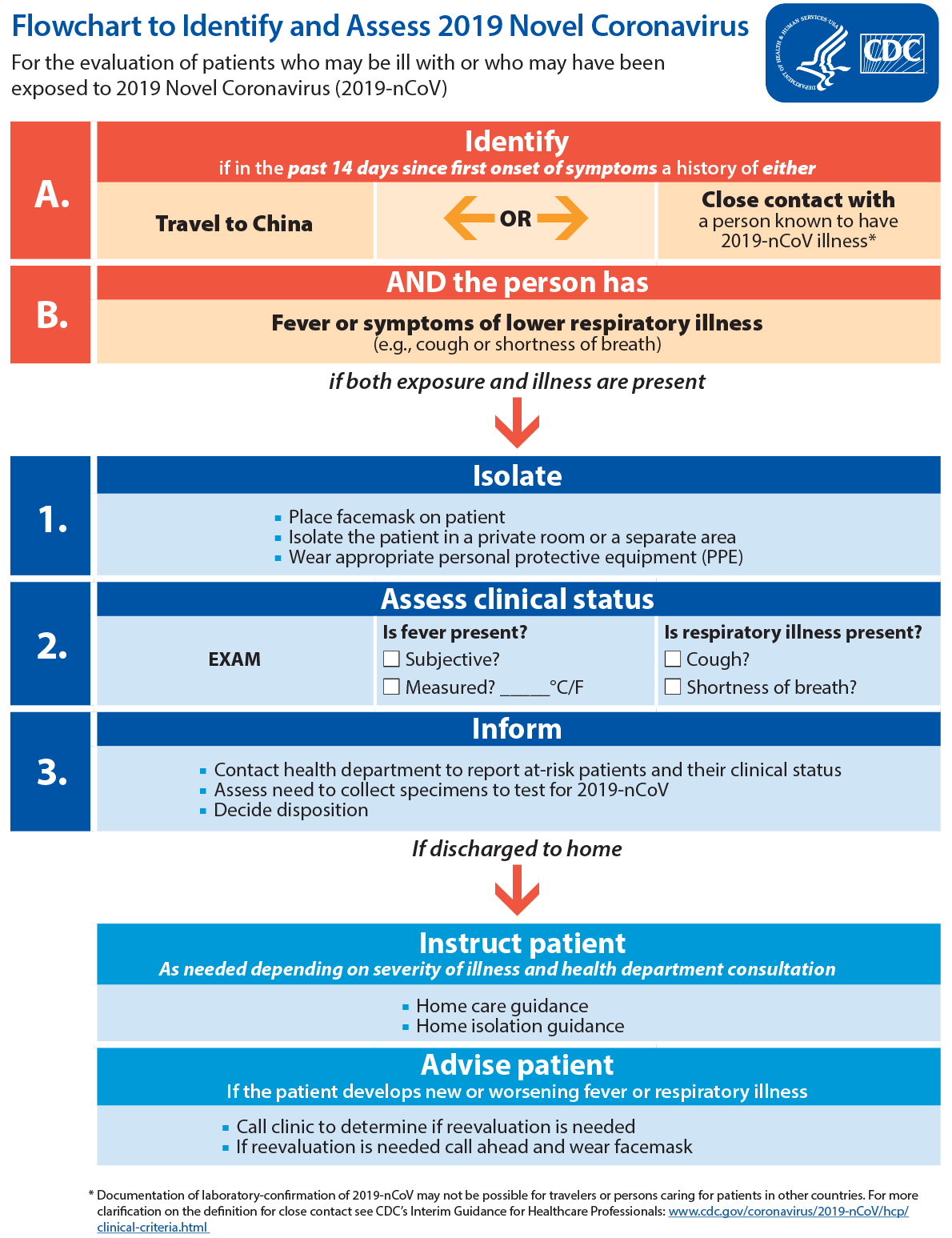
Text Equivalent
For the evaluation of patients who may be ill with or who may have been exposed to 2019 Novel Coronavirus (2019-nCoV)
- Identify if in the past 14 days since first onset of symptoms a history of either travel to china or close contact with a person known to have 2019-nCoV illness*
- AND the person has fever or symptoms of lower respiratory illness (e.g., cough or shortness of breath)
if both exposure and illness are present
- Isolate
- Place facemask on patient
- Isolate the patient in a private room or a separate area
- Wear appropriate personal protective equipment (PPE)
- Assess clinical status.
EXAM
Is fever present?
Subjective?
Measured? _____°C/F
Is respiratory illness present?
Cough?
Shortness of breath?
- Inform
- Contact health department to report at-risk patients and their clinical status
- Assess need to collect specimens to test for 2019-nCoV
- Decide disposition
If discharged to home
Instruct patient as needed depending on severity of illness and health department consultation
- Home care guidance
- Home isolation guidance
Advise patient if the patient develops new or worsening fever or respiratory illness
- Call clinic to determine if reevaluation is needed
- If reevaluation is needed call ahead and wear facemask
* Documentation of laboratory-confirmation of 2019-nCoV may not be possible for travelers or persons caring for patients in other countries. For more clarification on the definition for close contact see CDC’s Interim Guidance for Healthcare Professionals.
CDC: Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for 2019-nCoV in the United States
Tuesday, February 11th, 2020https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-for-ems.html
Background
Emergency medical services (EMS) play a vital role in responding to requests for assistance, triaging patients, and providing emergency medical treatment and transport for ill persons. However, unlike patient care in the controlled environment of a healthcare facility, care and transports by EMS present unique challenges because of the nature of the setting, enclosed space during transport, frequent need for rapid medical decision-making, interventions with limited information, and a varying range of patient acuity and jurisdictional healthcare resources.
When preparing for and responding to patients with confirmed or possible 2019-Novel Coronavirus (2019-nCov) infection, close coordination and effective communications are important among 911 Public Safety Answering Points (PSAPs)— commonly known as 911 call centers, the EMS system, healthcare facilities, and the public health system. Each PSAP and EMS system should seek the involvement of an EMS medical director to provide appropriate medical oversight. For the purposes of this guidance, “EMS clinician” means prehospital EMS and medical first responders. When 2019-nCoV is suspected in a patient needing emergency transport, prehospital care providers and healthcare facilities should be notified in advance that they may be caring for, transporting, or receiving a patient who may have 2019-nCoV infection.
Updated information about 2019-nCov may be accessed at https://www.cdc.gov/coronavirus/2019-ncov/index.html. Infection prevention and control recommendations can be found here: https://www.cdc.gov/coronavirus/2019-nCoV/hcp/infection-control.html. Additional information for healthcare personnel can be found at https://www.cdc.gov/coronavirus/2019-nCoV/guidance-hcp.html.
Case Definition for 2019-nCoV
CDC’s most current case definition for a person under investigation (PUI) for 2019-nCov may be accessed at https://www.cdc.gov/coronavirus/2019-nCoV/clinical-criteria.html.
Recommendations for 911 PSAPs
Municipalities and local EMS authorities should coordinate with state and local public health, PSAPs, and other emergency call centers to determine need for modified caller queries about 2019-nCoV, outlined below.
Development of these modified caller queries should be closely coordinated with an EMS medical director and informed by local, state, and federal public health authorities, including the city or county health department(s), state health department(s), and CDC.
Modified Caller Queries
PSAPs or Emergency Medical Dispatch (EMD) centers (as appropriate) should question callers and determine the possibility that this call concerns a person who may have signs or symptoms and risk factors for 2019-nCoV. The query process should never supersede the provision of pre-arrival instructions to the caller when immediate lifesaving interventions (e.g., CPR or the Heimlich maneuver) are indicated. Patients in the United States who meet the appropriate criteria should be evaluated and transported as a PUI. Information on 2019-nCoV will be updated as the public health response proceeds. PSAPs and medical directors can access CDC’s PUI definitions here.
Information on a possible PUI should be communicated immediately to EMS clinicians before arrival on scene in order to allow use of appropriate personal protective equipment (PPE). PSAPs should utilize medical dispatch procedures that are coordinated with their EMS medical director and with the local or state public health department.
PSAPs and EMS units that respond to ill travelers at US international airports or other ports of entry to the United States (maritime ports or border crossings) should be in contact with the CDC quarantine station of jurisdiction for the port of entry (see: CDC Quarantine Station Contact List) for planning guidance. They should notify the quarantine station when responding to that location if a communicable disease is suspected in a traveler. CDC has provided job aids for this purpose to EMS units operating routinely at US ports of entry. The PSAP or EMS unit can also call CDC’s Emergency Operations Center at (770)488-7100 to be connected with the appropriate CDC quarantine station.
Recommendations for EMS Clinicians and Medical First Responders
EMS clinician practices should be based on the most up-to-date 2019-nCoV clinical recommendations and information from appropriate public health authorities and EMS medical direction.
State and local EMS authorities may direct EMS clinicians to modify their practices as described below.
Patient assessment
- If PSAP call takers advise that the patient is suspected of having 2019-nCoV, EMS clinicians should put on appropriate PPE before entering the scene. EMS clinicians should consider the signs, symptoms, and risk factors of 2019-nCoV (https://www.cdc.gov/coronavirus/2019-nCoV/clinical-criteria.html).
- If information about potential for 2019-nCoV has not been provided by the PSAP, EMS clinicians should exercise appropriate precautions when responding to any patient with signs or symptoms of a respiratory infection. Initial assessment should begin from a distance of at least 6 feet from the patient, if possible. Patient contact should be minimized to the extent possible until a facemask is on the patient. If 2019-nCoV infection is suspected, all PPE as described below should be used. If 2019-nCoV infection is not suspected, EMS clinicians should follow standard procedures and use appropriate PPE for evaluating a patient with a potential respiratory infection.
- A facemask should be worn by the patient for source control. If a nasal cannula is in place, a facemask should be worn over the nasal cannula. Alternatively, an oxygen mask can be used if clinically indicated. If the patient requires intubation, see below for additional precautions for aerosol-generating procedures.
- During transport, limit the number of providers in the patient compartment to essential personnel to minimize possible exposures.
Recommended Personal Protective Equipment (PPE)
- EMS clinicians who will directly care for a patient with possible 2019-nCoV infection or who will be in the compartment with the patient should follow Standard, Contact, and Airborne Precautions, including the use of eye protection. Recommended PPE includes:
- A single pair of disposable patient examination gloves. Change gloves if they become torn or heavily contaminated,
- Disposable isolation gown,
- Respiratory protection (i.e., N-95 or higher-level respirator), and
- Eye protection (i.e., goggles or disposable face shield that fully covers the front and sides of the face).
- Drivers, if they provide direct patient care (e.g., moving patients onto stretchers), should wear all recommended PPE . After completing patient care and before entering an isolated driver’s compartment, the driver should remove and dispose of PPE and perform hand hygiene to avoid soiling the compartment.
- If the transport vehicle does not have an isolated driver’s compartment, the driver should remove the face shield or goggles, gown and gloves and perform hand hygiene. A respirator should continue to be used during transport.
- All personnel should avoid touching their face while working.
- On arrival, after the patient is released to the facility, EMS clinicians should remove and discard PPE and perform hand hygiene. Used PPE should be discarded in accordance with routine procedures.
- Other required aspects of Standard Precautions (e.g., injection safety, hand hygiene) are not emphasized in this document but can be found in the guideline titled Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings.
Precautions for Aerosol-Generating Procedures
- If possible, consult with medical control before performing aerosol-generating procedures for specific guidance.
- In addition to the PPE described above, EMS clinicians should exercise caution if an aerosol-generating procedure (e.g., bag valve mask (BVM) ventilation, oropharyngeal suctioning, endotracheal intubation, nebulizer treatment, continuous positive airway pressure (CPAP), bi-phasic positive airway pressure (biPAP), or resuscitation involving emergency intubation or cardiopulmonary resuscitation (CPR)) is necessary.
- BVMs, and other ventilatory equipment, should be equipped with HEPA filtration to filter expired air.
- EMS organizations should consult their ventilator equipment manufacturer to confirm appropriate filtration capability and the effect of filtration on positive-pressure ventilation.
- If possible, the rear doors of the transport vehicle should be opened and the HVAC system should be activated during aerosol-generating procedures. This should be done away from pedestrian traffic.
EMS Transport of a PUI or Patient with Confirmed 2019-nCoV to a Healthcare Facility (including interfacility transport)
If a patient with an exposure history and signs and symptoms suggestive of 2019-nCoV infection requires transport to a healthcare facility for further evaluation and management (subject to EMS medical direction), the following actions should occur during transport:
- EMS clinicians should notify the receiving healthcare facility that the patient has an exposure history and signs and symptoms suggestive of 2019-nCoV infection so that appropriate infection control precautions may be taken prior to patient arrival.
- Keep the patient separated from other people as much as possible.
- Family members and other contacts of patients with possible 2019-nCoV infection should not ride in the transport vehicle, if possible. If riding in the transport vehicle, they should wear a facemask.
- Isolate the ambulance driver from the patient compartment and keep pass-through doors and windows tightly shut.
- When possible, use vehicles that have isolated driver and patient compartments that can provide separate ventilation to each area.
- Close the door/window between these compartments before bringing the patient on board.
- During transport, vehicle ventilation in both compartments should be on non-recirculated mode to maximize air changes that reduce potentially infectious particles in the vehicle.
- If the vehicle has a rear exhaust fan, use it to draw air away from the cab, toward the patient-care area, and out the back end of the vehicle.
- Some vehicles are equipped with a supplemental recirculating ventilation unit that passes air through HEPA filters before returning it to the vehicle. Such a unit can be used to increase the number of air changes per hour (ACH) (https://www.cdc.gov/niosh/hhe/reports/pdfs/1995-0031-2601.pdfpdf icon).
- If a vehicle without an isolated driver compartment and ventilation must be used, open the outside air vents in the driver area and turn on the rear exhaust ventilation fans to the highest setting. This will create a negative pressure gradient in the patient area.
- Follow routine procedures for a transfer of the patient to the receiving healthcare facility (e.g., wheel the patient directly into an Airborne Infection Isolation Room).
Documentation of patient care
- Documentation of patient care should be done after EMS clinicians have completed transport, removed their PPE, and performed hand hygiene.
- Any written documentation should match the verbal communication given to the emergency department providers at the time patient care was transferred.
- EMS documentation should include a listing of EMS clinicians and public safety providers involved in the response and level of contact with the patient (for example, no contact with patient, provided direct patient care). This documentation may need to be shared with local public health authorities.
Cleaning EMS Transport Vehicles after Transporting a PUI or Patient with Confirmed 2019-nCoV
The following are general guidelines for cleaning or maintaining EMS transport vehicles and equipment after transporting a PUI:
- After transporting the patient, leave the rear doors of the transport vehicle open to allow for sufficient air changes to remove potentially infectious particles.
- The time to complete transfer of the patient to the receiving facility and complete all documentation should provide sufficient air changes.
- When cleaning the vehicle, EMS clinicians should wear a disposable gown and gloves. A face shield or facemask and goggles should also be worn if splashes or sprays during cleaning are anticipated.
- Ensure that environmental cleaning and disinfection procedures are followed consistently and correctly, to include the provision of adequate ventilation when chemicals are in use. Doors should remain open when cleaning the vehicle.
- Routine cleaning and disinfection procedures (e.g., using cleaners and water to pre-clean surfaces prior to applying an EPA-registered, hospital-grade disinfectant to frequently touched surfaces or objects for appropriate contact times as indicated on the product’s label) are appropriate for 2019-nCoV in healthcare settings, including those patient-care areas in which aerosol-generating procedures are performed.
- Products with EPA-approved emerging viral pathogens claims are recommended for use against 2019-nCoV. These products can be identified by the following claim:
- “[Product name] has demonstrated effectiveness against viruses similar to 2019-nCoV on hard non-porous surfaces. Therefore, this product can be used against 2019-nCoV when used in accordance with the directions for use against [name of supporting virus] on hard, non-porous surfaces.”
- This claim or a similar claim, will be made only through the following communications outlets: technical literature distributed exclusively to health care facilities, physicians, nurses and public health officials, “1-800” consumer information services, social media sites and company websites (non-label related). Specific claims for “2019-nCoV” will not appear on the product or master label.
- See additional information about EPA-approved emerging viral pathogens claimsexternal icon.
- If there are no available EPA-registered products that have an approved emerging viral pathogen claim, products with label claims against human coronaviruses should be used according to label instructions.
- Clean and disinfect the vehicle in accordance with standard operating procedures. All surfaces that may have come in contact with the patient or materials contaminated during patient care (e.g., stretcher, rails, control panels, floors, walls, work surfaces) should be thoroughly cleaned and disinfected using an EPA-registered hospital grade disinfectant in accordance with the product label.
- Clean and disinfect reusable patient-care equipment before use on another patient, according to manufacturer’s instructions.
- Follow standard operating procedures for the containment and disposal of used PPE and regulated medical waste.
- Follow standard operating procedures for containing and laundering used linen. Avoid shaking the linen.
Follow-up and/or Reporting Measures by EMS Clinicians After Caring for a PUI or Patient with Confirmed 2019-nCoV
EMS clinicians should be aware of the follow-up and/or reporting measures they should take after caring for a PUI or patient with confirmed 2019-nCoV:
- State or local public health authorities should be notified about the patient so appropriate follow-up monitoring can occur.
- EMS agencies should develop policies for assessing exposure risk and management of EMS personnel potentially exposed to 2019-nCoV in coordination with state or local public health authorities. Decisions for monitoring, excluding from work, or other public health actions for HCP with potential exposure to 2019-nCoV should be made in consultation with state or local public health authorities. Refer to the Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with 2019 Novel Coronavirus (2019-nCoV) for additional information.
- EMS agencies should develop sick-leave policies for EMS personnel that are nonpunitive, flexible, and consistent with public health guidance. Ensure all EMS personnel, including staff who are not directly employed by the healthcare facility but provide essential daily services, are aware of the sick-leave policies.
- EMS personnel who have been exposed to a patient with suspected or confirmed 2019-nCoV should notify their chain of command to ensure appropriate follow-up.
- Any unprotected exposure (e.g., not wearing recommended PPE) should be reported to occupational health services, a supervisor, or a designated infection control officer for evaluation.
- EMS clinicians should be alert for fever or respiratory symptoms (e.g., cough, shortness of breath, sore throat). If symptoms develop, they should self-isolate and notify occupational health services and/or their public health authority to arrange for appropriate evaluation.
EMS Employer Responsibilities
The responsibilities described in this section are not specific for the care and transport of PUIs or patients with confirmed 2019-nCoV. However, this interim guidance presents an opportunity to assess current practices and verify that training and procedures are up-to-date.
- EMS units should have infection control policies and procedures in place, including describing a recommended sequence for safely donning and doffing PPE.
- Provide all EMS clinicians with job- or task-specific education and training on preventing transmission of infectious agents, including refresher training.
- Ensure that EMS clinicians are educated, trained, and have practiced the appropriate use of PPE prior to caring for a patient, including attention to correct use of PPE and prevention of contamination of clothing, skin, and environment during the process of removing such equipment.
- Ensure EMS clinicians are medically cleared, trained, and fit tested for respiratory protection device use (e.g., N95 filtering facepiece respirators), or medically cleared and trained in the use of an alternative respiratory protection device (e.g., Powered Air-Purifying Respirator, PAPR) whenever respirators are required. OSHA has a number of respiratory training videosexternal icon.
- EMS units should have an adequate supply of PPE.
- Ensure an adequate supply of or access to EPA-registered hospital grade disinfectants (see above for more information) for adequate decontamination of EMS transport vehicles and their contents.
- Ensure that EMS clinicians and biohazard cleaners contracted by the EMS employer tasked to the decontamination process are educated, trained, and have practiced the process according to the manufacturer’s recommendations or the EMS agency’s standard operating procedures.
Additional Resources
The EMS Infectious Disease Playbook, published by the Office of the Assistant Secretary for Preparedness and Response’s Technical Resources, Assistance Center, Information Exchange (TRACIE) is a resource available to planners at https://www.ems.gov/pdf/ASPR-EMS-Infectious-Disease-Playbook-June-2017.pdfpdf iconexternal icon
Public Health Emergency Law Online Training
Thursday, January 30th, 2020Management of public health emergencies requires effective use of legal authorities. In these incidents, public health and emergency management responses must be coordinated under a complex set of federal, state, tribal, and local laws. CDC’s Public Health Emergency Law course prepares state, tribal, local, and territorial practitioners to make informed legal decisions related to emergency preparedness and response activities in their jurisdictions.
PHEL consists of three competency-based units and covers legal issues to consider before, during, and after public health emergencies. Each interactive unit takes about 40 minutes to complete.
Public Health Emergency Law Online Trainingexternal icon
- Unit 1—Introduction to Emergency Management Systems Preparedness and Response
Covers the legal underpinnings of emergency management systems - Unit 2—Emergency Powers: Protection of Persons, Volunteers, and Responders
Describes legal considerations for personnel responding to emergencies - Unit 3—Emergency Powers: Management and Protection of Property and Supplies
Examines considerations surrounding materials and property during public health emergencies
Disclaimer: These course materials are for instructional use only and are not intended as a substitute for professional legal or other advice. While every effort has been made to verify the accuracy of these materials, the legal authorities and requirements may vary from jurisdiction to jurisdiction. Always seek the advice of an attorney or other qualified professional with any questions you may have regarding a legal matter. The contents of these presentations have not been formally disseminated by the Centers for Disease Control and Prevention and should not be construed to represent any agency determination or policy.
CDC: Preventing waterborne outbreaks in refugee camps
Monday, December 16th, 2019Hundreds of thousands of ethnic Rohingyas crossed the border into Cox’s Bazar, Bangladesh to escape violence in Rakhine State in Myanmar. More than 900,000 forcibly displaced Myanmar nationals live in refugee camps in Bangladesh. Because conditions are crowded and the area is prone to flooding, the risk of Acute Watery Diarrhea (AWD) and other waterborne disease outbreaks had to be reduced during the 2018 monsoon season. Humanitarian partners distributed household water treatment products throughout the camps and combined this with messages to promote good hygiene. However, a recent water, sanitation and hygiene (WASH) survey estimated that only 13% of households treat household water. Of the 182 households that reported to treat water using chlorine tablets, only 53 (21%) had detectable chlorine in their stored water, an indicator of whether water was treated and was protected from recontamination during storage in households. Bucket chlorination, where an attendant sitting by the well directly chlorinates each bucket of water as it is collected was also implemented, but only at a small number of wells. Because of low levels of household water treatment in the camps, the water, sanitation, and hygiene (WASH) team recommended to scale-up bucket chlorination to ensure households were using chlorinated water during the monsoon season.

The WASH team within CDC’s Emergency Response and Recovery Branch (ERRB) worked with UNICEF and non-governmental partners to increase bucket chlorination from June to September 2018. In July, ERRB WASH specialists measured chlorine levels in one camp to provide a snapshot of current levels of chlorine in the water. After this, the WASH team started a program to monitor bucket chlorination, using mobile phone surveys to ensure chlorinators were present and that chlorine was in water in nearby households. In addition, they piloted guidelines to help identify which drinking water wells should receive bucket chlorination first. Finally, the WASH team provided guidance to implementing partners on how to scale-up and improve bucket chlorination based on assessment and monitoring results.
In addition, CDC supported the WASH Sector in Cox’s Bazar and UNICEF by training local staff on how to conduct water quality testing and drafting guidance on water quality monitoring, including a system to monitor E. coli levels in wells through the dry and monsoon seasons.
The Rohingya face extremely challenging circumstances as they seek refuge in makeshift camps. The 2019 UN World Water Day theme is “leaving no one behind” and CDC seeks to assist partners in providing safe, treated drinking water to the world’s most vulnerable communities.