Archive for the ‘Food-borne diseases’ Category
Reports of 11 more Escherichia coli O157:H7 illnesses linked to the Romaine lettuce outbreak.
Wednesday, November 28th, 2018Based on new information, CDC is narrowing its warning to consumers. CDC is advising that U.S. consumers not eat and retailers and restaurants not serve or sell any romaine lettuce harvested from the Central Coastal growing regions of northern and central California. If you do not know where the romaine is from, do not eat it.
- Romaine lettuce products will be labeled with a harvest location by region. It may take some time before these labels are available.
- If the romaine lettuce is not labeled with a harvest growing region, do not buy, serve, sell, or eat it.
- Check bags or boxes of romaine lettuce for a label indicating where the lettuce was harvested. Romaine lettuce labeled with a harvest region outside of the Central Coastal growing regions of northern and central California (such as the desert growing region near Yuma, the California desert growing region near Imperial County and Riverside County, the state of Florida, and Mexico) is not linked to this outbreak.
- If you do not know where your romaine lettuce was harvested, do not eat it and throw it away.
- This advice includes all types or uses of romaine lettuce, such as whole heads of romaine, hearts of romaine, and bags and boxes of precut lettuce and salad mixes that contain romaine, including baby romaine, spring mix, and Caesar salad.
- If you do not know if the lettuce is romaine or whether a salad mix contains romaine, do not eat it and throw it away.
- Wash and sanitize drawers or shelves in refrigerators where romaine was stored. Follow these five steps to clean your refrigerator.
- Restaurants and retailers should check the label on bags or boxes of romaine lettuce, or ask their suppliers about the source of their romaine lettuce.
- Do not sell or serve any romaine lettuce harvested from the Central Coastal growing regions of northern and central California.
- If you do not know where your romaine lettuce was harvested, do not sell or serve it.
- Hydroponically or greenhouse-grown romaine lettuce has not been linked to this outbreak.
- Take action if you have symptoms of an E. coli infection:
- Talk to your healthcare provider.
- Write down what you ate in the week before you started to get sick.
- Report your illness to the health department.
- Assist public health investigators by answering questions about your illness.
Advice to Clinicians
- Antibiotics are not recommended for patients with E. coli O157 infections. Antibiotics are also not recommended for patients in whom E.coli O157 infection is suspected, until diagnostic testing rules out this infection.
- Some studies have shown that administering antibiotics to patients with E. coli O157 infections might increase their risk of developing hemolytic uremic syndrome (a type of kidney failure), and the benefit of antibiotic treatment has not been clearly demonstrated.
Latest Outbreak Information

At A Glance
- Reported Cases: 43
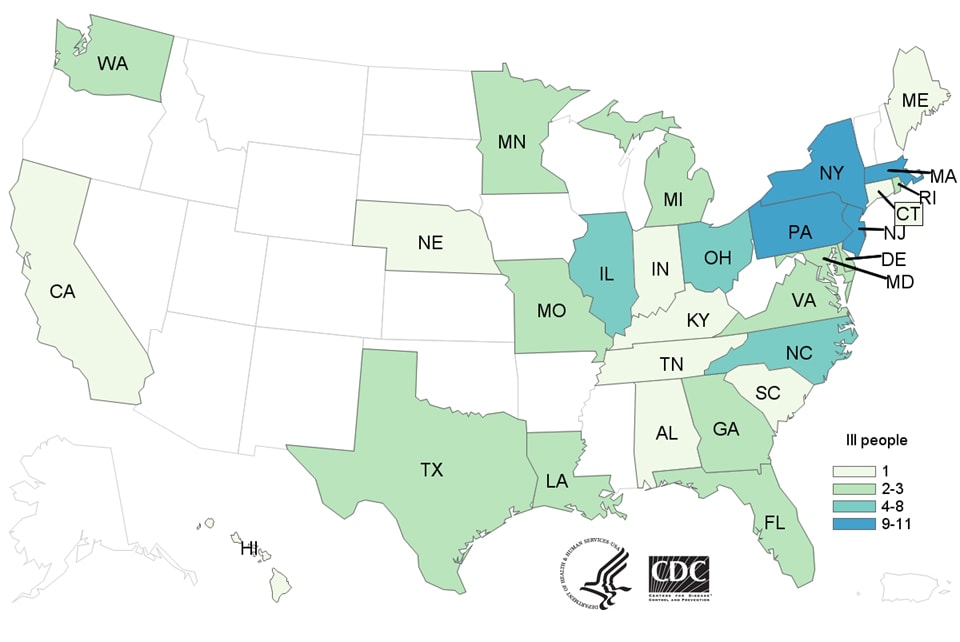
- States: 12
- Hospitalizations: 16
- Deaths: 0
- Recall: No
- Since the last update on November 20, an additional 11 ill people have been included in this investigation.
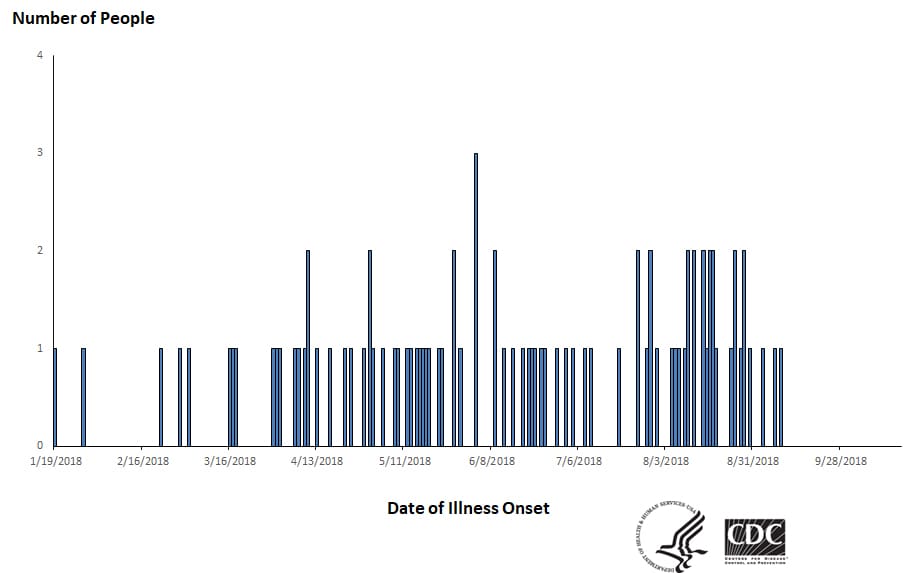
- Forty-three people infected with the outbreak strain of Shiga toxin-producing E. coli O157:H7 have been reported from 12 states.
- Illnesses started on dates ranging from October 8, 2018 to October 31, 2018.
- Sixteen people have been hospitalized, including one person who developed hemolytic uremic syndrome, a type of kidney failure. No deaths have been reported.
- The Public Health Agency of Canada has identified ill people infected with the same DNA fingerprint of E. coli O157:H7 bacteria in Canada.
- Epidemiologic and traceback evidence from the United States and Canada indicates that romaine lettuce harvested from the Central Coastal growing regions of northern and central California is a likely source of the outbreak.
- Ill people in this outbreak were infected with E. coli bacteria with the same DNA fingerprint as the E. coli strain isolated from ill people in a 2017 outbreak linked to leafy greens in the United States and to romaine lettuce in Canada. The current outbreak is not related to a spring 2018 multistate outbreak of E. coli O157:H7 infections linked to romaine lettuce.
- CDC is advising that consumers not eat any romaine lettuce harvested from the Central Coastal growing regions of northern and central California. No common grower, supplier, distributor, or brand of romaine lettuce has been identified.
- This investigation is ongoing, and CDC will provide more information as it becomes available.
Symptoms of E. coli Infection

- People usually get sick from Shiga toxin-producing E. coli (STEC) 2–8 days (average of 3–4 days) after swallowing the germ.
- Some people with a STEC infection may get a type of kidney failure called hemolytic uremic syndrome (HUS).
- E. coli infection is usually diagnosed by testing a stool sample.
- Antibiotics are not recommended for patients with suspected E. coli infections until diagnostic testing can be performed and E. coli infection is ruled out. Some studies have shown that administering antibiotics to patients with E. coli infections might increase their risk of developing HUS, and a benefit of treatment has not been clearly demonstrated.
- For more information, see Symptoms of E. coli Infection.
Investigation Details
November 26, 2018
CDC, public health and regulatory officials in several states, Canada, and the FDA are investigating a multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (E. coli O157:H7) infections.
As of November 26, 2018, 43 people infected with the outbreak strain of E. coli O157:H7 have been reported from 12 states. A list of the states and the number of cases in each can be found on the Map of Reported Cases page.
Illnesses started on dates ranging from October 8, 2018 to October 31, 2018. Ill people range in age from 1 to 84 years, with a median age of 25. Sixty-nine percent of ill people are female. Of 38 people with information available, 16 (42%) have been hospitalized, including one person who developed hemolytic uremic syndrome, a type of kidney failure. No deaths have been reported.
Illnesses that occurred after October 31, 2018, might not yet be reported due to the time it takes between when a person becomes ill with E. coli infection and when the illness is reported. This takes an average of two to three weeks.
Investigation of the Outbreak
Epidemiologic and traceback evidence indicates that romaine lettuce from the Central Coastal growing regions of northern and central California is a likely source of this outbreak.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. Twenty-two (88%) of 25 people interviewed reported eating romaine lettuce. This percentage is significantly higher than results from a survey[PDF – 787 KB] of healthy people in which 47% reported eating romaine lettuce in the week before they were interviewed. Ill people reported eating different types of romaine lettuce in several restaurants and at home.
Preliminary traceback information from the FDA indicates that ill people in this outbreak ate romaine lettuce harvested from the Central Coastal growing regions of northern and central California. At this time, no common grower, supplier, distributor, or brand of romaine lettuce has been identified. CDC is advising that consumers not eat and restaurants and retailers not sell any romaine lettuce from the Central Coastal growing regions of northern and central California.
This investigation is ongoing, and CDC will provide more information as it becomes available.
Statement from FDA Commissioner Scott Gottlieb, M.D., on the current romaine lettuce E. coli O157:H7 outbreak investigation
Tuesday, November 27th, 2018For Immediate Release
November 26, 2018
Statement
The U.S. Food and Drug Administration, along with the Centers for Disease Control and Prevention and state authorities, continues to investigate a multistate outbreak of E. coli O157:H7 infections associated with consumption of romaine lettuce in the U.S. As of Nov. 26, 2018, this outbreak has resulted in 43 people becoming ill in 12 states, with the last reported illness onset date being Oct. 31, 2018. An additional 22 people in Canada have become ill, and the FDA and our partners are also coordinating the investigation with Canadian health and food safety authorities.
As we continue to investigate this outbreak, today the FDA is announcing new steps to help consumers better identify where their romaine is grown through voluntary labeling.
To prevent additional cases of E. coli O157:H7, on Nov. 20, 2018 the CDC advised the public not to consume romaine lettuce and to destroy any romaine lettuce in their homes. At the same time, the FDA requested that all romaine lettuce on the market, including in restaurants and other commercial establishments, should be withdrawn and destroyed. The FDA made this request because initial information available at that time had not identified a likely source for the outbreak that would allow a targeted request, it was likely romaine lettuce contaminated with E. coli O157:H7 that could cause illness was still available on the market, and a market withdrawal was the fastest way to remove potentially contaminated product. The romaine lettuce industry agreed to comply with the FDA’s request to withdraw any romaine lettuce on the market on that date, and available information suggests this action was effective in removing potentially contaminated romaine lettuce from retail establishments.
Over the Thanksgiving holiday, the FDA continued to investigate the outbreak. Our investigation at this point suggests that romaine lettuce associated with the outbreak comes from areas of California that grow romaine lettuce over the summer months, and that the outbreak appears to be related to “end of season” romaine lettuce harvested from these areas. The involved areas include the Central Coast growing regions of central and northern California.
The FDA is continuing tracebacks of romaine lettuce from locations where impacted consumers purchased or consumed romaine lettuce before they became ill in order to identify specific locations that are the likely source of the outbreak and to determine the factors that resulted in contamination. Through laboratory studies we have identified that the E. coli O157:H7 strain causing the outbreak is similar to one that produced an outbreak of E. coli O157:H7 in the fall of 2017 that also occurred in the U.S. and Canada, which was associated with consumption of leafy greens in the U.S. and specifically romaine lettuce in Canada.
Based on further discussions with the leafy greens industry and with agricultural authorities, we have begun to narrow the location in which we believe the contaminated romaine in the current outbreak was grown. At the time of the outbreak, the vast majority of the romaine on the market was being grown in the Central Coast region of California. Since, then harvesting of romaine lettuce from this region has ended for the year. Growing and harvesting of romaine lettuce is now shifting to the winter growing regions of the U.S., which include mainly the California desert region of the Imperial Valley, the desert region of Arizona in and around Yuma, and Florida. Romaine lettuce grown in Mexico is exported to the U.S. during the winter months. Smaller quantities of romaine lettuce are grown in other states. At this time, the FDA has no information to suggest any of these growing areas are involved in the current outbreak, which began well before any romaine lettuce from these winter growing locations was available for harvest. In addition, hydroponic romaine lettuce and romaine lettuce grown in green-houses is also marketed in the U.S., but there is no information to suggest these products are implicated in any identified E. coli O157:H7 outbreak.
The FDA believes it was critically important to have a “clean break” in the romaine supply available to consumers in the U.S. in order to purge the market of potentially contaminated romaine lettuce related to the current outbreak. This appears to have been accomplished through the market withdrawal request of Nov. 20, 2018.
Knowing the growing origin of produce will continue to play an important role in allowing consumers to avoid contaminated products and facilitating market withdrawals and tracebacks. That’s why we previously called on the romaine lettuce industry to provide unambiguous and clear information to consumers regarding where their lettuce was grown and when it was harvested.
To this end, the FDA recently participated in discussions with the major producers and distributors of romaine lettuce in the U.S. and with the major trade associations representing the produce industry regarding product labeling and dating to assure consumers that any romaine lettuce that will come onto the market is not associated with the current outbreak of E. coli O157:H7. The labeling will identify the origin of the romaine based on harvest region, along with the date of harvest. This can improve the ability of the FDA to provide more targeted information to consumers in the event of a future outbreak of illness. The FDA also has commitments from the romaine lettuce industry that such labeling will continue into the future and become the standard for their products.
In addition, the leafy greens industry has agreed to establish a task force to find solutions for long term labeling of romaine lettuce and other leafy greens for helping to identify products and to put in place standards for traceability of product. The task force will also examine information from this outbreak to identify measures that led to its occurrence and how to prevent ongoing safety problems with romaine lettuce. One outcome could be to extend the commitment for labeling for origin and date of harvest to other leafy greens.
Therefore, the FDA is issuing the following updated advice as part of our investigation and public warning:
Based on discussions with major producers and distributors, romaine lettuce entering the market will now be labeled with a harvest location and a harvest date. Romaine lettuce entering the market can also be labeled as being hydroponically or greenhouse grown. If it does not have this information, you should not eat or use it.
If consumers, retailers, and food service facilities are unable to identify that romaine lettuce products are not affected – which means determining that the products were grown outside the California regions that appear to be implicated in the current outbreak investigation — we urge that these products not be purchased, or if purchased, be discarded or returned to the place of purchase.
Romaine lettuce that was harvested outside of the Central Coast growing regions of northern and central California does not appear to be related to the current outbreak. Hydroponically- and greenhouse-grown romaine also does not appear to be related to the current outbreak. There is no recommendation for consumers or retailers to avoid using romaine harvested from these sources.
The FDA has urged growers, processors, distributors and retailers to:
- clearly and prominently label all individually packaged romaine products to identify growing region and harvest date for romaine; and
- clearly and prominently label at the point of sale the growing region when it is not possible for romaine lettuce suppliers to label the package (e.g. individual unwrapped whole heads of romaine lettuce available in retail stores).
We hope that growers, processors, distributors and retailers will join us in our effort to protect consumers by applying these labeling recommendations to their products. We remain committed to identifying ways to decrease the incidence and impact of foodborne illness outbreaks, and will continue to provide updates on our investigation and changes to our advice on romaine lettuce as more information becomes available.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
###
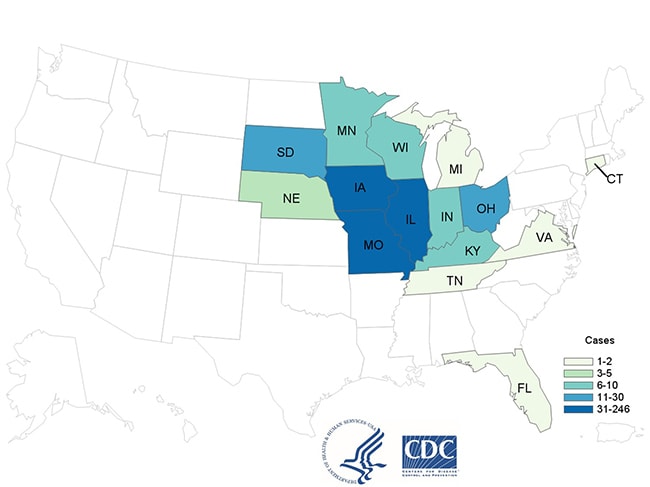
People infected with the outbreak strain of Salmonella Newport, by state of residence, as of November 15, 2018 (n=246)
Sunday, November 18th, 2018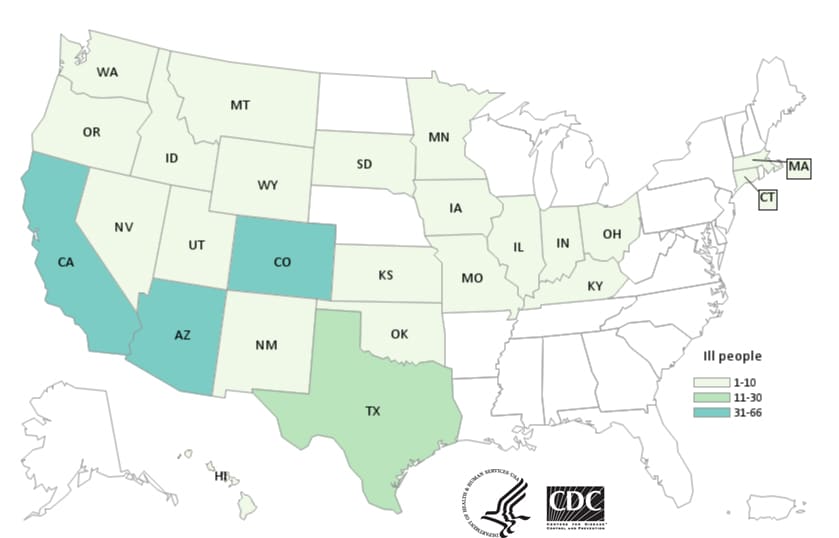
Restaurant Inspection Letter Grades and Salmonella Infections in NYC
Friday, November 16th, 2018“Rates of Salmonella infection in the United States have not changed over the past 20 years. Restaurants are frequent settings for Salmonella outbreaks and sporadic infections. Few studies have examined the effect of posting letter grades for restaurant inspections on the incidence of foodborne illness. We compared Salmonella infection rates in New York, New York, USA (NYC), with those in the rest of New York state before and after implementation of a letter grade system for restaurant inspections in NYC. We calculated a segmented regression model for interrupted time series data. After implementation of letter grading, the rate of Salmonella infections decreased 5.3% per year in NYC versus the rest of New York state during 2011–2015, compared with the period before implementation, 2006–2010. Posting restaurant inspection results as letter grades at the point of service was associated with a decline in Salmonella infections in NYC and warrants consideration for broader use.”
Firestone MJ, Hedberg CW. Restaurant inspection letter grades and Salmonella infections, New York, New York, USA. Emerg Infect Dis. 2018 Dec [date cited]. https://doi.org/10.3201/eid2412.180544
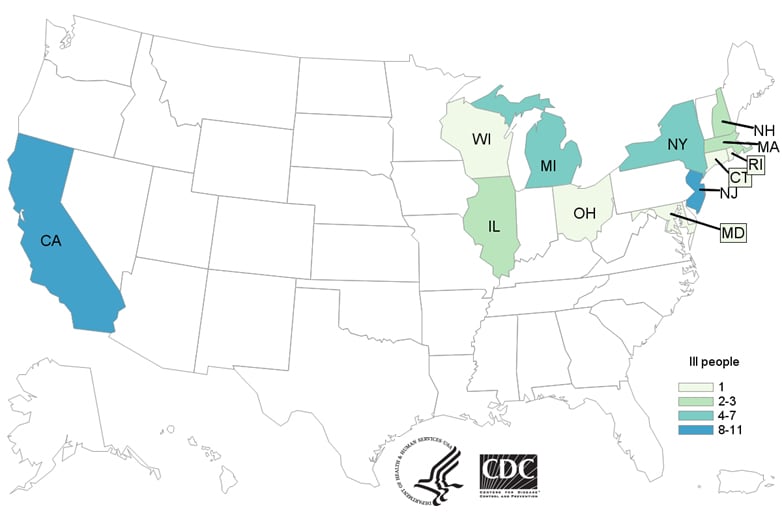
CDC: 92 people infected with the outbreak strain of Salmonella Infantis have been reported from 29 states after coming in contact with raw chicken products
Thursday, October 18th, 2018Latest Outbreak Information

At A Glance
- Reported Cases: 92
- States: 29
- Hospitalizations: 21
- Deaths: 0
- Ninety-two people infected with the outbreak strain of Salmonella Infantis have been reported from 29 states.
- Twenty-one people have been hospitalized, and no deaths have been reported.
- Epidemiologic and laboratory evidence indicates that many types of raw chicken products from a variety of sources are contaminated with Salmonella Infantis and are making people sick.
- In interviews, ill people report eating different types and brands of chicken products purchased from many different locations.
- The outbreak strain has been identified in samples taken from raw chicken pet food, raw chicken products, and live chickens.
- Antibiotic resistance testing conducted by CDC on Salmonella bacteria isolated from ill people shows that the outbreak strain is resistant to multiple antibiotics. Read the Advice to Clinicians.
- A single, common supplier of raw chicken products or of live chickens has not been identified.
- The outbreak strain of Salmonella Infantis is present in live chickens and in many types of raw chicken products, indicating it might be widespread in the chicken industry. CDC and USDA-FSIS have shared this information with representatives from the chicken industry and asked about steps that they may be taking to reduce Salmonella contamination.
The Insect Allies program: A bioweapon?
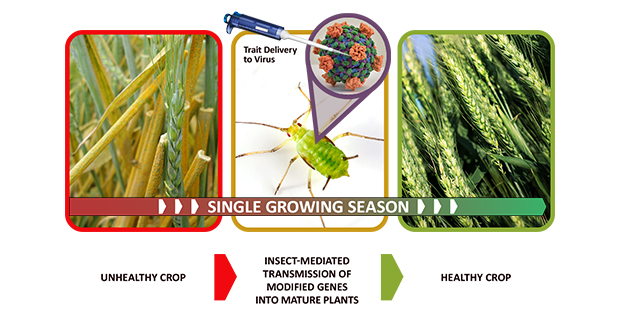
Friday, October 5th, 2018DARPA Enlists Insects to Protect Agricultural Food Supply
New program aims for insect delivery of protective genes to modify mature plants within a single growing season
It may not be obvious to humans, but the life of a plant is full of peril. Viruses, pests, fungi, herbicides, drought, pollution, salinity, flooding, and frost—the plants that we depend on for food, clean air, and materials are challenged by myriad threats, natural and man-made. By extension, human populations are put at risk when food security is challenged and the agricultural underpinnings of our economies are destabilized, especially when threats emerge rapidly or unexpectedly.
Farmers and others responsible for plant health use longstanding tools such as crop rotation, selective breeding, pesticides, slash-and-burn clearing, and quarantine to shelter plants and defend against the worst effects of pathogens, pests, and environmental insults, but these methods can be slow, inefficient, and damaging to the environment, and may require extensive and expensive infrastructure. And while scientists and farmers are increasingly turning to molecular techniques to improve resilience in plant varieties, today’s genomic tools generally do not allow for alteration of mature plants.
A new DARPA program is poised to provide an alternative to traditional agricultural threat response, using targeted gene therapy to protect mature plants within a single growing season. DARPA proposes to leverage a natural and very efficient two-step delivery system to transfer modified genes to plants: insect vectors and the plant viruses they transmit. In the process, DARPA aims to transform certain insect pests into “Insect Allies,” the name of the new effort.
“Insects eat plants and insects transmit the majority of plant viruses,” said Blake Bextine, the DARPA program manager for Insect Allies. “DARPA plans to harness the power of this natural system by engineering genes inside plant viruses that can be transmitted by insects to confer protective traits to the target plants they feed upon.”
Insect Allies’ three technical areas—trait design, insect vector optimization, and selective gene therapy in mature plants—layer together to support the goal of rapidly transforming mature plants to protect against natural or intentional agricultural disruption without the need for extensive infrastructure. The foundational knowledge and generalizable tools developed under the program could also support future agricultural innovation.
One of the most effective existing methods for protecting plants—selective breeding of disease resistance—typically involves five to seven years of work to identify the relevant protective genes and another 10 years or more to propagate the desired traits throughout plant populations. Insect Allies aims to effect the expression of desired traits within a single season. Performers will be challenged to develop compatible systems of naturally occurring plant viruses, herbivorous insects, and target crops, then genetically tune these systems to maximize transmission and uptake of traits across the entire target plant population with zero transmission to non-target plants.
“Genetic modification of plants has historically been done only to plant embryos inside of laboratories using tissue cultures,” Bextine said. “Transforming mature plants en masse would be an enormous achievement and pave the way for future breakthroughs in agriculture.”
Insect Allies will emphasize biosafety and biosecurity. All work will be conducted inside closed laboratories, greenhouses, or other secured facilities.
DARPA will host a Proposers Day on November 18, 2016, at the Executive Conference Center in Arlington, Va., to further clarify the program vision and answer questions from potential proposers. There is a webcast option for the Proposers Day. Advance registration is required: http://www.sa-meetings.com/InsectAlliesProposersDay. Additional details are provided in a Special Notice: https://www.fbo.gov/spg/ODA/DARPA/CMO/DARPA-SN-16-73/listing.html. Full program details, including instructions for submitting a proposal, are available in the Broad Agency Announcement: https://www.fbo.gov/spg/ODA/DARPA/CMO/HR001117S0002/listing.html.
Canada: Public Health Notice – Outbreaks of Salmonella infections linked to raw chicken, including frozen raw breaded chicken products
Sunday, September 16th, 2018Public Health Agency of Canada
Why you should take note
The Public Health Agency of Canada is collaborating with provincial and territorial public health partners, the Canadian Food Inspection Agency and Health Canada to investigate outbreaks of Salmonella infections across Canada linked to raw chicken, including frozen raw breaded chicken products.
On September 13, 2018, Canada’s Council of Chief Medical Officers of Health issued a statement advising Canadians to follow proper food safety practices when handling, preparing or consuming frozen raw breaded chicken products such as chicken nuggets, chicken strips, chicken burgers, popcorn chicken and chicken fries.
When not thoroughly cooked, frozen breaded chicken products containing raw chicken pose an increased health risk to individuals who handle, prepare or consume them. These products may appear to be pre-cooked or browned, but they should be handled and prepared with caution. Illnesses can be avoided by following cooking instructions carefully and verifying the internal temperature after cooking, as recommended, before consuming these products. Frozen raw breaded chicken products and raw chicken pieces must be cooked to an internal temperature of at least 74°C (165°F) to ensure that they are safe to eat. Whole chicken needs to be cooked to an internal temperature of 82°C (180°F).
Summary of investigations
In May 2017, Government of Canada scientists began using a new technology called “whole genome sequencing” to help identify and respond to outbreaks. Over the past year and a half, federal, provincial and territorial health and food safety partners have investigated 12 national outbreaks linked to raw chicken, including frozen raw breaded chicken products. The Canadian Food Inspection Agency has issued food recall warnings for seven products linked to some of these outbreak investigations.
As of September 13, 2018, there have been 419 laboratory-confirmed cases of Salmonella illness investigated as part of the illness outbreaks across the country: British Columbia (36), Alberta (60), Saskatchewan (13), Manitoba (19), Ontario (146), Quebec (98), New Brunswick (23), Nova Scotia (9), Prince Edward Island (1), Newfoundland and Labrador (10), Northwest Territories (1), Yukon (1), and Nunavut (2). There have been 86 individuals hospitalized as part of these outbreaks. Three individuals have died; however, Salmonella was not the cause of death for two of those individuals, and it was not determined whether Salmonella contributed to the cause of death for the third individual. Infections have occurred in Canadians of all ages and genders.
All current and future Salmonella outbreak investigations linked to raw chicken, including frozen raw breaded chicken products, and related food recall warnings will be listed in the next section of the public health notice to remind Canadians of the ongoing risk associated with these types of food products.
Active investigations
Active national Salmonella outbreak investigations linked to raw chicken including frozen raw breaded chicken products, coordinated by the Public Health Agency of Canada:
September 13, 2018 (update) – Salmonella Enteritidis
September 13, 2018 (update) – Salmonella Enteritidis
Canadians are advised not to consume the recalled products, and retailers and restaurants are advised to not sell or serve the recalled products.
Information about previously investigated and currently closed national Salmonella outbreak investigations linked to raw chicken including frozen raw breaded chicken products, coordinated by the Public Health Agency of Canada since May 2017 is available at the end of this notice.
Who is most at risk
Anyone can become sick with a Salmonella infection, but infants, children, seniors and those with weakened immune systems are at higher risk of serious illness because their immune systems are more fragile.
Most people who become ill from a Salmonella infection will recover fully after a few days. It is possible for some people to be infected with the bacteria and to not get sick or show any symptoms, but to still be able to spread the infection to others.
What you should do to protect your health
Check to see whether you have the recalled frozen raw breaded chicken products in your home or place of business. If you do:
- Do not use or eat the recalled products. Secure the recalled products in a plastic bag and then either throw them out or return them to the store where they were purchased.
- If you do not have the original packaging of a frozen raw breaded chicken product and you are unsure of whether it is included in the food recall warnings, throw it out just to be safe.
Wash your hands with soap and warm water immediately following any contact with a recalled product.
Beyond recalled food items, frozen raw breaded chicken products may appear to be pre-cooked or browned, but they may contain raw chicken and should be handled and prepared no differently from other raw chicken products.
If you are preparing breaded chicken products, such as nuggets, strips, burgers or fries, the following precautions should be taken to protect your health:
- Do not eat raw or undercooked frozen breaded chicken products. Cook all frozen raw breaded chicken products to an internal temperature of at least 74°C (165°F) to ensure that they are safe to eat. Use a digital food thermometer to verify the temperature. Insert the digital food thermometer through the side of the product, all the way to the middle. Oven-safe meat thermometers that are designed for testing whole chicken and roasts during cooking are not suitable for testing nuggets, strips or burgers.
- Microwave cooking of frozen raw breaded chicken products—including chicken nuggets, strips, burgers, popcorn chicken or chicken fries—is not recommended because of the possibility of uneven heating.
- Always follow the cooking instructions on the package, including for products labelled Uncooked, Cook and Serve, Ready to Cook, and Oven Ready.
- Wash your hands thoroughly with soap and warm water before and after handling frozen raw breaded chicken products.
- Use a separate plate, cutting board and utensils when handling frozen raw breaded chicken products to prevent the spread of harmful bacteria.
- Do not re-use plates, cutting boards or utensils that have come in contact with frozen raw breaded chicken products to serve the cooked product unless they have been thoroughly washed.
Foods carrying Salmonella may look, smell and taste normal, so it’s important to follow safe food-handling tips for buying, chilling, thawing, cleaning, cooking, and storing any chicken products:
- Wash your hands thoroughly with soap and warm water before and after handling all types of raw chicken.
- Always follow the cooking instructions provided on the package. Cook chicken to a safe internal temperature that has been checked using a digital thermometer. Raw chicken pieces should be cooked to an internal temperature of 74°C (165°F). Whole chicken should be cooked to an internal temperature of 82°C (180°F).
- Keep raw chicken away from other food while shopping, storing, repackaging, cooking and serving foods.
- Never rinse chicken before using it because the bacteria can spread everywhere the water splashes, creating more of a hazard.
- Use warm, soapy water to clean knives, cutting boards, utensils, your hands, and any surfaces that have come in contact with food, especially meat, chicken and fish.
- If you have been diagnosed with a Salmonella infection or any other gastrointestinal illness, do not cook food for other people.
- For more information, read our poultry safety fact sheet.
Symptoms
Symptoms of a Salmonella infection, called salmonellosis, typically start 6 to 72 hours after exposure to Salmonella bacteria from an infected animal or contaminated product.
Symptoms include:
- fever
- chills
- diarrhea
- abdominal cramps
- headache
- nausea
- vomiting
These symptoms usually last for four to seven days. In healthy people, salmonellosis often clears up without treatment. In some cases, severe illness and hospitalization may occur. In some cases, antibiotics may be required. People who are infected with Salmonella bacteria can be infectious from several days to several weeks. People who experience symptoms, or who have underlying medical conditions, should contact their health care provider if they suspect they have a Salmonella infection.
What the Government of Canada is doing
The Government of Canada is committed to food safety. The Public Health Agency of Canada leads the human health investigation into an outbreak and is in regular contact with its federal, provincial and territorial partners to monitor the situation and to collaborate on steps to address an outbreak.
Health Canada provides food-related health risk assessments to determine whether the presence of a certain substance or microorganism poses a health risk to consumers.
The Canadian Food Inspection Agency conducts food safety investigations into the possible food source of an outbreak.
The Government of Canada will continue to update Canadians as new information related to these investigations becomes available.
Additional information
- New Requirements for Industry to Reduce Salmonella
- Frozen Raw Breaded Chicken Fact Sheet
- Salmonella Fact Sheet
- Poultry Safety Fact Sheet
- General Food Safety Tips
- Recalls and safety alerts mobile application
Media Contact
Public Health Agency of Canada
Media Relations
(613) 957-2983
hc.media.sc@canada.ca
Public Inquiries
Call toll-free: 1-866-225-0709
Email: info@hc-sc.gc.ca
The Publix supermarket chain voluntarily recalls ground chuck shipped to stores in two dozen Florida counties.
Saturday, September 1st, 2018“On August 30, 2018, Publix Super Markets Inc. issued a voluntary recall on an undetermined amount of ground beef products made from chuck that may be contaminated with Escherichia coli, according to a U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) release. To date, there are 15 E. coli cases in Florida associated with the recalled ground beef product.….”
CDC: 40 more cases in a Cyclospora outbreak linked to McDonald’s salads, pushing the illness total to 476.
Saturday, August 18th, 2018At least 350 people including women and children have been poisoned after eating food in a funeral reception.
Monday, August 13th, 2018“…..Gulab Shah, a resident of the area, said the people fallen ill were in critical situation as there were no transportation facilities to shift the poisoned people to healthcare centers.….”