Archive for the ‘Food-borne diseases’ Category
Madagascar’s health service ministry says 8 children have died after suffering acute food poisoning believed to have been caused by eating sea turtle meat in northern Madagascar.
Saturday, January 20th, 2018Abstract
Poisoning from eating sea turtles, medically known as chelonitoxism, is seen especially in coastal areas. It remains a public health problem in Madagascar, despite a ban on hunting these animals. The objective of this study was to describe its epidemiological and clinical aspects and outcome to improve knowledge and prevention of this type of poisoning. Chelonitoxism occurred in May 2014, affecting the population in Antsanitia, a fishing village in northwest Mahajanga, Madagascar. All patients came first to the CSB I basic health center in Antsanitia and were subsequently hospitalized at the Mahajanga CHU Pzaga, 51 in the adult emergency department and 25 in the pediatrics department. These 76 patients ranged in age from 3 months to 79 years. The predominant clinical signs were gastrointestinal and neurological disorders. ENT-oral signs characterized the poisoning. Ingestion of the turtle fat caused intermediate and severe disease forms in adults. Breastfeeding was a prognostic factor in children. Signs of severity appeared within 72 hours in adults. After intensive resuscitation, the signs of poisoning disappeared after 12 days. The severe form predominated in children; death was either early or delayed to the second to sixth day after consumption. It is essential to develop awareness of this danger among the entire coastal population of Madagascar to prevent this kind of poisoning.
Multistate Outbreak of Salmonella Infections Linked to Coconut Tree Brand Frozen Shredded Coconut
Wednesday, January 17th, 2018Posted January 16, 2018 3:45 PM ET
Multistate Outbreak of Salmonella Infections Linked to Coconut Tree Brand Frozen Shredded Coconut
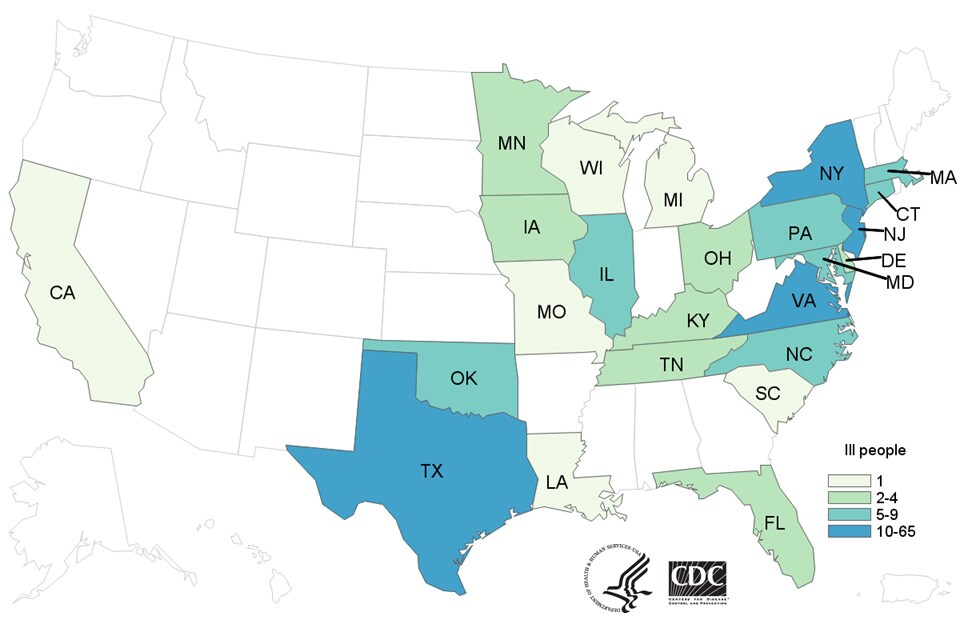
![People infected with the outbreak strains of Salmonella I,4,[5],12:b:- or Salmonella Newport, by state of residence, as of January 12, 2018](https://www.cdc.gov/salmonella/coconut-01-18/images/map/big-map-1-12-18.jpg)
Highlights
- CDC, public health and regulatory officials in several states, and the U.S. Food and Drug Administration are investigating a multistate outbreak of Salmonella infections.
- Twenty-five people infected with the outbreak strains of Salmonella I 4,[5],12:b:- or Salmonella Newport have been reported from nine states.
- Six ill people have been hospitalized. No deaths have been reported.
- Epidemiologic, laboratory, and traceback evidence(https://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/index.html) indicates that Coconut Tree Brand Frozen Shredded Coconut, distributed by Evershing International Trading Company, is the likely source of this multistate outbreak.
- On January 3, 2018, Evershing International Trading Company recalled all 16 oz. Coconut Tree Brand Frozen Shredded Coconut after Salmonella was identified in the product by officials in Massachusetts.
- CDC recommends that retailers not sell, restaurants not serve, and consumers not eat recalled frozen shredded coconut.
- The recalled product was packaged in 16-ounce plastic bags labeled as Coconut Tree Brand Shredded Coconut.
- If you have recalled frozen shredded coconut in your home, you can return it to the place of purchase for a refund.
- If you aren’t sure if the frozen coconut you bought is Coconut Tree Brand frozen Shredded Coconut, you can ask the place of purchase. Restaurants and retailers can ask their supplier.
- When in doubt, don’t eat, sell, or serve it. Throw it out.
- Wash and sanitize countertops as well as drawers or shelves in freezers or refrigerators(https://www.cdc.gov/foodsafety/communication/clean-refrigerator-steps.html) where frozen shredded coconut was stored.
- This investigation is ongoing. CDC will provide updates when more information is available.
Initial Announcement
January 16, 2018
CDC, public health and regulatory officials in several states, and the U.S. Food and Drug Administration (FDA) are investigating a multistate outbreak of Salmonella infections.
Public health investigators are using the PulseNet(https://www.cdc.gov/pulsenet/index.html) system to identify illnesses that may be part of this outbreak. PulseNet is the national subtyping network of public health and food regulatory agency laboratories coordinated by CDC. DNA fingerprinting is performed on Salmonella bacteria isolated from ill people by using techniques called pulsed-field gel electrophoresis(https://www.cdc.gov/pulsenet/pathogens/pfge.html) (PFGE) and whole genome sequencing(https://www.cdc.gov/ncezid/dfwed/keyprograms/tracking-foodborne-illness-wgs.html) (WGS). CDC PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. WGS gives a more detailed DNA fingerprint than PFGE.
As of January 12, 2018, 25 people infected with the outbreak strains of Salmonella I 4,[5],12:b:- (24 people) or Salmonella Newport (1 person) have been reported from 9 states. A list of the states and the number of cases in each can be found on the Case Count Map(https://www.cdc.gov/salmonella/coconut-01-18/map.html) page. One more ill person infected with the outbreak strain of Salmonella I 4,[5],12:b:- has been reported from Canada.
Signs & Symptoms
What are the signs and symptoms of Salmonella infection?
Most people infected with Salmonella develop the following signs and symptoms 12-72 hours after being exposed to the bacteria:
- Diarrhea
- Fever
- Abdominal cramps
How long does the illness last?
- The illness usually lasts 4 to 7 days, and most people recover without treatment.
- In some people, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other places in the body.
- In rare cases, Salmonella infection can cause death unless the person is treated promptly with antibiotics.
Who is more likely to have a severe illness?
- Children younger than 5 years
- Adults older than 65
- People with weakened immune systems
More information about Salmonella and steps people can take to reduce their risk of infection with Salmonella in general can be found on the CDCSalmonella(https://www.cdc.gov/salmonella/general/index.html) website.
WGS showed that isolates from people infected with Salmonella I 4,[5],12:b:- are closely related genetically. This close genetic relationship means that people in this outbreak are more likely to share a common source of infection.
Illnesses started on dates ranging from May 11, 2017 to November 4, 2017. Ill people range in age from 1 year to 82, with a median age of 19. Among ill people, 19 (76%) are male. Six people (24%) report being hospitalized. No deaths have been reported.
This outbreak can be illustrated with a chart showing the number of people who became ill each day. This chart is called an epidemic curve, or epi curve(https://www.cdc.gov/salmonella/coconut-01-18/epi.html).
Investigation of the Outbreak
Epidemiologic, laboratory, and traceback evidence(https://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/index.html) indicates that Coconut Tree Brand frozen Shredded Coconut is the likely source of this multistate outbreak. This investigation is ongoing.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. Ten (63%) of 16 people interviewed reported eating or maybe eating coconut. Of these 10 people, 8 (80%) reported having an Asian-style dessert drink that contained frozen shredded coconut.
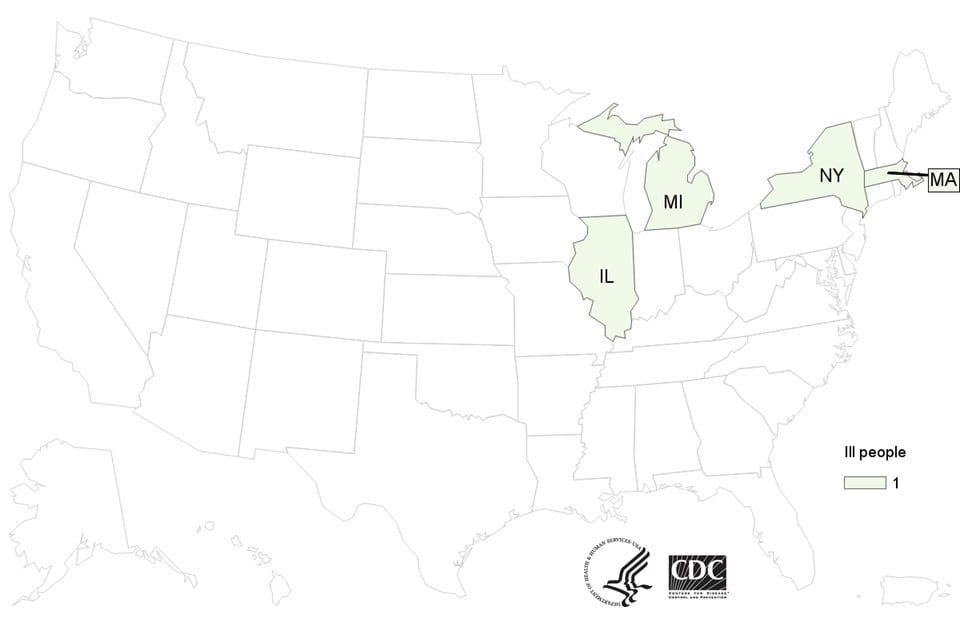
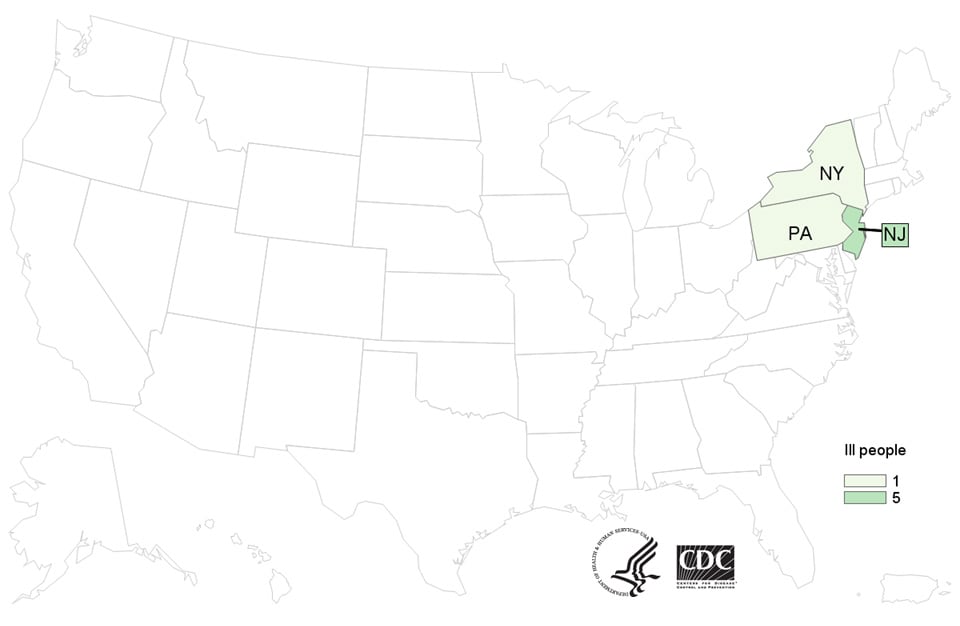
Throughout the outbreak investigation, state and local health officials have collected different food items from restaurants where ill people consumed Asian-style dessert drinks. In November 2017, laboratory testing of a sample from coconut milk made in one restaurant in New York did not identify the outbreak strain of Salmonella I 4,[5],12:b:-, but did identify a strain of Salmonella Newport. This sample was from coconut milk made with Coconut Tree Brand frozen Shredded Coconut, as well as other ingredients. WGS showed that the Salmonella Newport isolated from the coconut milk was closely related genetically to a Salmonella Newport isolate from an ill person from Massachusetts who had consumed an Asian-style dessert drink.
In December 2017, officials in Massachusetts collected food items from a restaurant where that ill person had consumed Asian-style dessert drinks. One sample from frozen shredded coconut identified a strain of Salmonella that was new to the PulseNet database and has not been linked to any illnesses. This sample was from an unopened package of Coconut Tree Brand Frozen Shredded Coconut. As a result, on January 3, 2018, Evershing International Trading Company recalled all Coconut Tree Brand Frozen Shredded Coconut. The recalled product was packaged in 16-ounce plastic bags.
Officials in Massachusetts returned to the restaurant and collected more Coconut Tree Brand frozen Shredded Coconut in January 2018. On January 12, laboratory testing confirmed that samples from that frozen shredded coconut identified the outbreak strain of Salmonella I 4,[5],12:b:-. Laboratory testing of other samples identified several types of Salmonella bacteria, including Salmonella Javiana, Salmonella Rissen, and Salmonella Thompson. These samples were from unopened packages of Coconut Tree Brand Frozen Shredded Coconut sold before January 3, 2018. CDC is reviewing the PulseNet database to determine if the other Salmonella isolates from the frozen shredded coconut are linked to any illnesses.
The frozen shredded coconut linked to this outbreak was used as an ingredient in Asian-style dessert drinks served at restaurants. The product was also sold in grocery stores and markets in several states. Frozen shredded coconut can last for several months if kept frozen and may still be in retail stores or in people’s homes. CDC recommends that retailers not sell, restaurants not serve, and consumers not eat recalled Coconut Tree Brand frozen Shredded Coconut.
This investigation is ongoing and we will provide updates when they are available.
Tainted sea turtles allegedly killed 10 Madagascaris including a 1-year old.
Monday, January 15th, 2018Translation: “….After returning from
fishing, the villagers divided the meat from 2 sea turtles.
Immediately after the meal the 1st symptoms of food poisoning
appeared. People could not stop vomiting and were taken to hospital.
In spite of intensive care of the ill, 10 people, including a baby of
one year, did not survive…..”


FDA: Information about E. coli O157:H7 Outbreak Likely Linked to Leafy Greens
Friday, January 12th, 2018January 10, 2018
The U.S. Food and Drug Administration is working with the Centers for Disease Control and Prevention (CDC), and state and local authorities in an investigation of an outbreak of Shiga toxin-producing Escherichia coli (E. coli) O157:H7 illnesses. The FDA has also been in contact with Canadian food safety authorities on this outbreak, since cases were first identified in Canada. ![]()
Whole genome sequencing showed that the U.S. and Canadian E. coli O157:H7 strains are closely related, suggesting a common source of illness. Canadian health officials identified romaine lettuce as the likely source of their outbreak. CDC has been working to determine the source of the outbreak in the U.S., and today announced it believes that this outbreak is likely linked to leafy greens. Health officials have not identified a specific type of leafy greens that sick people ate in common.
The known illnesses in the U.S. had illness onsets in late November and early December. This suggests that suspect leafy greens linked to this outbreak are likely no longer in the food supply.
The FDA’s outbreak investigation team is working with CDC and state and local officials to determine what ill people ate, where they bought it, and the distribution chain — all with the goal of reaching where these foods were produced, to see if there’s any common food or point where the food might have become contaminated. At this point, we have not identified a common or single point of origin for the food that made people ill. We want to make sure the information we provide is accurate and when we have information that consumers can use – such as any foods to avoid – we will share it immediately.
French baby milk formula maker Lactalis has ordered a global product recall over fears of salmonella contamination because 26 infants in the country have become sick since early December.
Monday, December 11th, 2017“…..Lactalis is one of the world’s biggest dairy producers. Company spokesman Michel Nalet told AFP “nearly 7,000 tonnes” of production may have been contaminated….”
CDC recommendations to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas during the period of September 2017 – March 2018.
Wednesday, October 25th, 2017Advice for Providers Treating Patients in or Recently Returned from Hurricane-Affected Areas, Including Puerto Rico and US Virgin Islands
Distributed via the CDC Health Alert Network
October 24, 2017, 1330 ET (1:30 PM ET)
CDCHAN-00408
Summary
The Centers for Disease Control and Prevention (CDC) is working with federal, state, territorial, and local agencies and global health partners in response to recent hurricanes. CDC is aware of media reports and anecdotal accounts of various infectious diseases in hurricane-affected areas, including Puerto Rico and the US Virgin Islands (USVI). Because of compromised drinking water and decreased access to safe water, food, and shelter, the conditions for outbreaks of infectious diseases exist.
The purpose of this HAN advisory is to remind clinicians assessing patients currently in or recently returned from hurricane-affected areas to be vigilant in looking for certain infectious diseases, including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. Additionally, this Advisory provides guidance to state and territorial health departments on enhanced disease reporting.
Background
Hurricanes Irma and Maria made landfall in Puerto Rico and USVI in September 2017, causing widespread flooding and devastation. Natural hazards associated with the storms continue to affect many areas. Infectious disease outbreaks of diarrheal and respiratory illnesses can occur when access to safe water and sewage systems are disrupted and personal hygiene is difficult to maintain. Additionally, vector borne diseases can occur due to increased mosquito breeding in standing water; both Puerto Rico and USVI are at risk for outbreaks of dengue, Zika, and chikungunya.
Health care providers and public health practitioners should be aware that post-hurricane environmental conditions may pose an increased risk for the spread of infectious diseases among patients in or recently returned from hurricane-affected areas; including leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza. The period of heightened risk may last through March 2018, based on current predictions of full restoration of power and safe water systems in Puerto Rico and USVI.
In addition, providers in health care facilities that have experienced water damage or contaminated water systems should be aware of the potential for increased risk of infections in those facilities due to invasive fungi, nontuberculous Mycobacterium species, Legionella species, and other Gram-negative bacteria associated with water (e.g., Pseudomonas), especially among critically ill or immunocompromised patients.
Cholera has not occurred in Puerto Rico or USVI in many decades and is not expected to occur post-hurricane.
Recommendations
These recommendations apply to healthcare providers treating patients in Puerto Rico and USVI, as well as those treating patients in the continental US who recently traveled in hurricane-affected areas (e.g., within the past 4 weeks), during the period of September 2017 – March 2018.
- Health care providers and public health practitioners in hurricane-affected areas should look for community and healthcare-associated infectious diseases.
- Health care providers in the continental US are encouraged to ask patients about recent travel (e.g., within the past 4 weeks) to hurricane-affected areas.
- All healthcare providers should consider less common infectious disease etiologies in patients presenting with evidence of acute respiratory illness, gastroenteritis, renal or hepatic failure, wound infection, or other febrile illness. Some particularly important infectious diseases to consider include leptospirosis, dengue, hepatitis A, typhoid fever, vibriosis, and influenza.
- In the context of limited laboratory resources in hurricane-affected areas, health care providers should contact their territorial or state health department if they need assistance with ordering specific diagnostic tests.
- For certain conditions, such as leptospirosis, empiric therapy should be considered pending results of diagnostic tests— treatment for leptospirosis is most effective when initiated early in the disease process. Providers can contact their territorial or state health department or CDC for consultation.
- Local health care providers are strongly encouraged to report patients for whom there is a high level of suspicion for leptospirosis, dengue, hepatitis A, typhoid, and vibriosis to their local health authorities, while awaiting laboratory confirmation.
- Confirmed cases of leptospirosis, dengue, hepatitis A, typhoid fever, and vibriosis should be immediately reported to the territorial or state health department to facilitate public health investigation and, as appropriate, mitigate the risk of local transmission. While some of these conditions are not listed as reportable conditions in all states, they are conditions of public health importance and should be reported.
For More Information
- General health information about hurricanes and other tropical storms: https://www.cdc.gov/disasters/hurricanes/index.html
- Information about Hurricane Maria: https://www.cdc.gov/disasters/hurricanes/hurricane_maria.html
- Information for Travelers:
- Travel notice for Hurricanes Irma and Maria in the Caribbean: https://wwwnc.cdc.gov/travel/notices/alert/hurricane-irma-in-the-caribbean
- Health advice for travelers to Puerto Rico: https://wwwnc.cdc.gov/travel/destinations/traveler/none/puerto-rico?s_cid=ncezid-dgmq-travel-single-001
- Health advice for travelers to the U.S. Virgin Islands: https://wwwnc.cdc.gov/travel/destinations/traveler/none/usvirgin-islands?s_cid=ncezid-dgmq-travel-leftnav-traveler
- Resources from CDC Health Information for International Travel 2018 (the Yellow Book):
- Post-travel Evaluation: https://wwwnc.cdc.gov/travel/yellowbook/2018/post-travel-evaluation/general-approach-to-the-returned-traveler
- Information about infectious diseases after a disaster: https://www.cdc.gov/disasters/disease/infectious.html
- Dengue: https://www.cdc.gov/dengue/index.html
- Hepatitis A: https://www.cdc.gov/hepatitis/HAV/index.htm
- Leptospirosis: https://www.cdc.gov/leptospirosis/
- Typhoid fever: https://www.cdc.gov/typhoid-fever/index.html
- Vibriosis: https://www.cdc.gov/vibrio/index.html
- Information about other infectious diseases of concern:
- Conjunctivitis: https://www.cdc.gov/conjunctivitis/
- Influenza: https://www.cdc.gov/flu/index.htm
- Scabies: https://www.cdc.gov/parasites/scabies/index.html
- Tetanus and wound management: https://www.cdc.gov/disasters/emergwoundhcp.html
- Tetanus in Areas Affected by a Hurricane: Guidelines for Clinicians https://emergency.cdc.gov/coca/cocanow/2017/2017sept12.asp
CDC: 14 new Salmonella cases tied to papayas. The case total now stands at 235, with 78 hospitalizations and 2 deaths (1 in New York and 1 in California).
Saturday, September 16th, 2017CDC: Raw milk from the K-Bar Dairy in Paradise, Texas, tested positive for Brucella RB51, a rare bacterium that can cause serious illness.
Saturday, September 16th, 2017“People who consumed raw milk or raw milk products from one Texas dairy should contact their health care provider immediately, warn health investigators from the Centers for Disease Control and Prevention (CDC) and the Texas Department of State Health Services (DSHS). Raw milk from the K-Bar Dairy in Paradise, Texas (northwest of Fort Worth), tested positive for a rare but potentially serious bacteria known as Brucella RB51.
CDC advises that people who consumed raw milk or milk products from the K-Bar Dairy between June 1 and Aug. 7, 2017, should get antibiotic treatment to avoid the risk of lifelong, chronic infections. Initially, people with brucellosis experience fever, sweats, aches and fatigue. If not treated, Brucella RB51 infection can result in long-term complications, like arthritis; heart problems; enlargement of the spleen or liver; and, in rare cases, nervous system problems, like meningitis RB51 can cause severe illness in people with weakened immune systems and miscarriages in pregnant women…..”

Salmonella Kiambu Infections Linked to Yellow Maradol Papayas: 47 ill in 12 States & 1 Death
Saturday, July 22nd, 2017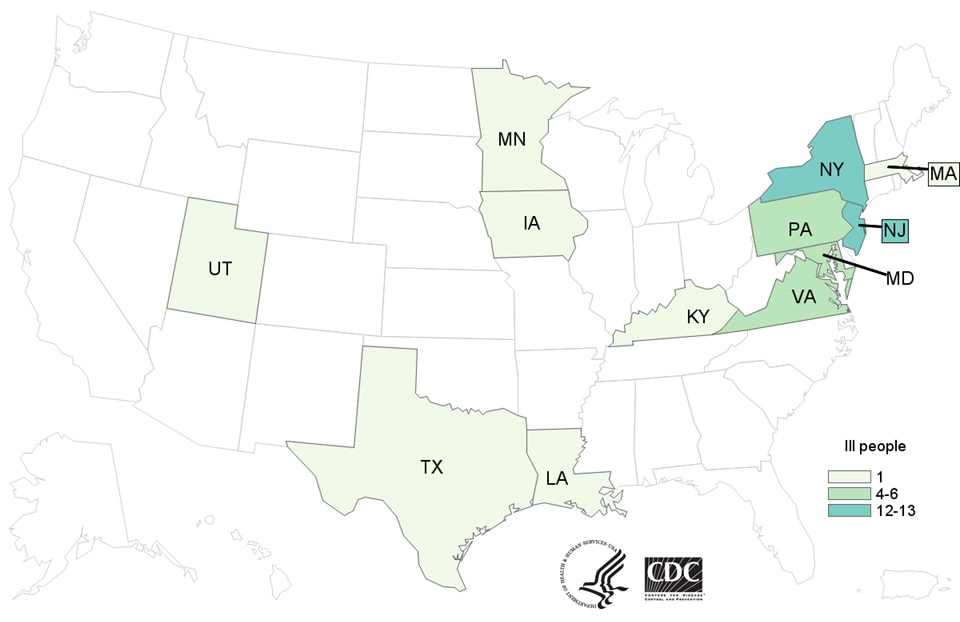
What are the signs and symptoms of Salmonella infection?
Most people infected with Salmonella develop the following signs and symptoms 12-72 hours after being exposed to the bacteria:
- Diarrhea
- Fever
- Abdominal cramps
How long does the illness last?
- The illness usually lasts 4 to 7 days, and most people recover without treatment.
- In some people, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other places in the body.
- In rare cases, Salmonella infection can cause death unless the person is treated promptly with antibiotics.
Who is more likely to have a severe illness?
- Children younger than 5 years
- Adults older than 65
- People with weakened immune systems
More information about Salmonella and steps people can take to reduce their risk of infection with Salmonella in general can be found on the CDCSalmonella(https://www.cdc.gov/salmonella/general/index.html) website.
Advice to Consumers, Restaurants, and Retailers

Yellow Maradol Papaya: Maradol papayas are a large, oval fruit that weighs 3 or more pounds, with green skins that turn yellow when the fruit is ripe. The flesh inside the fruit is salmon-colored.
CDC recommends that consumers not eat, restaurants not serve, and retailers not sell yellow Maradol papayas until we learn more.
- If you aren’t sure if the papaya you bought is a yellow Maradol papaya, you can ask the place of purchase. Restaurants and retailers can ask their supplier.
- When in doubt, don’t eat, sell, or serve them and throw them out.
- Wash and sanitize countertops as well as drawers or shelves in refrigerators where papayas were stored.
Contact a healthcare provider if you think you got sick from eating contaminated papaya.
- Most people infected with Salmonella develop the following signs and symptoms 12-72 hours after being exposed to the bacteria:
- Diarrhea
- Fever
- Abdominal cramps
Grilling safely: CDC
Friday, July 14th, 2017
Get Ready to Grill Safely

Food poisoning peaks in the summer months when warmer temperatures cause foodborne germs to flourish. Follow these steps for a safe and enjoyable grilling season.
Separate
When shopping, pick up meat, poultry, and seafood last, right before checkout. Separate them from other food in your shopping cart and grocery bags. To guard against cross-contamination, put packages of raw meat and poultry into individual plastic bags.
Chill
Keep meat, poultry, and seafood refrigerated until ready to grill. When transporting, keep below 40°F in an insulated cooler.
Clean
Wash your hands with soap before and after handling raw meat, poultry, and seafood. Wash work surfaces, utensils, and the grill before and after cooking.
Check your grill and tools
Use a moist cloth or paper towel to clean the grill surface before cooking. If you use a wire bristle brush, thoroughly inspect the grill’s surface before cooking. Wire bristles from grill cleaning brushes may dislodge and stick into food on the grill.
Don’t cross-contaminate
Throw out marinades and sauces that have touched raw meat juices, which can spread germs to cooked foods. Use clean utensils and a clean plate to remove cooked meat from the grill.
Cook
Use a food thermometer to ensure meat is cooked hot enough to kill harmful germs. When smoking, keep temperatures inside the smoker at 225°F to 300°F to keep meat a safe temperature while it cooks.
- 145°F – whole cuts of beef, pork, lamb, and veal (stand-time of 3 minutes at this temperature)
- 145°F – fish
- 160°F – hamburgers and other ground beef
- 165°F – all poultry and pre-cooked meats, like hot dogs
Smoking:
- 250°F – 300°F – inside smoke
After Grilling:
- 140°F or warmer – until it’s served
Refrigerate
Divide leftovers into small portions and place in covered, shallow containers. Put in freezer or fridge within two hours of cooking (one hour if above 90°F outside).
Learn More: